 |
 |
| Korean J Intern Med > Volume 22(2); 2007 > Article |
|
Abstract
Background
Most of the known risk factors associated with ischemic heart disease are based on studies from Western countries; there is only limited information on Korean populations. This study was designed to analyze age related differences in epidemiologic and clinical characteristics in patients who were admitted for coronary angiography for the evaluation of ischemic heart disease.
Methods
As part of the multicenter KCAR (Korean Coronary Artery disease Registry) Study, the clinical data of 6,549 patients, who were evaluated at the cardiac catheterization laboratory by coronary angiography, at seven university hospitals in Korea from March 1999 to December 2005, were registered into the KCAR database and analyzed. All patients were divided into three groups according to age: age Ōēż40, age 41-70 and age Ōēź71. All demographic and coronary angiographic features were analyzed for the different groups.
Results
The demographic data showed that compared to the older patients young patients Ōēż40 had a higher prevalence of males and smokers, but a lower prevalence of hypertension, diabetes and prior history of stroke and myocardial infarction. For the lipid profiles, the younger patients had much higher levels of total cholesterol, triglycerides and LDL-cholesterol than the older groups; however, there was no difference in the HDL-cholesterol levels among the three age groups. The most common component of the metabolic syndrome was obesity (79%) in the younger patients and hypertension (92%) in the older patients. The most common reason for presentation was ST-segment elevated myocardial infarction in the younger patients and unstable angina in the older patients.
Age-linked epidemiology of disease generally differs in prevalence, incidence and severity at presentation. The causes and outcome of coronary artery disease differ by age1). Younger patients <40 with an acute myocardial infarction have different clinical characteristics and a different prognosis than older patients2). Patients older than 70 have been shown to be at risk for overt coronary artery disease and for exercise- induced silent ischemia based on age alone even when asymptomatic3). Many risk factors have been identified for the development of ischemic heart disease (IHD) in elderly patients. In addition, the prevalence of IHD has been closely associated with sociodemographic, biological, psychological, and behavioral risk factors4). To date there is only limited information available on the clinical characteristics of ischemic heart disease in different age groups in the Korean population.
The KCAR (Korean Coronary Artery disease Registry) Study is a registry study initiated in 1999 to investigate the clinical characteristics of IHD in Korea. The purpose of the present study was to assess the differences in epidemiology, clinical characteristics and treatment modalities for IHD in Koreans based on age.
This study was a prospective, multicenter registry-based study performed from March 1999 to December 2005. The KCAR (Korean Coronary Artery disease Registry) Study was initiated in 1999 to determine and record the clinical characteristics of ischemic heart disease in the Korean population. Nationwide, seven university hospitals in Korea (Yeungnam University Hospital, Daegu: Chungnam University Hospital, Daejeon: Kyunghee University Hospital, Seoul: Chungbuk University Hospital, Cheongju: Chonnam University Hospital, Gwangju: Hanrim University Hospital, Seoul: Donga University Hospital, Busan) participated in this study. Research coordinators registered all patients, evaluated at the cardiac catheterization laboratory for the purpose of assessment or treatment of ischemic heart disease. This registry included all consecutive patients who had coronary angiography with one of the following: 1) evidence of myocardial ischemia on exercise electrocardiography (ECG) and myocardial perfusion scanning ; 2) induced coronary spasm with the ergonovine or acetylcholine provocation test 3) clinical evidence of myocardial infarction based on clinical symptoms, cardiac enzymes and ECG. The different patient diagnoses included syndrome X, variant angina, stable angina, unstable angina, ST-elevated MI (STEMI), and non-ST elevated MI (NSTEMI). All diagnoses were determined by expert consensus after review of the available clinical data. Patients with atypical chest pain and normal angiographic findings, without evidence of myocardial ischemia, were excluded from this study. On the day after admission, a detailed medical history was obtained from subjects and doctors and study coordinators performed a physical examination. The physical examination included height and weight recorded according to standard methods; the body mass index was calculated by weight (kg)/height (m)2. The total serum cholesterol and triglyceride levels were measured by enzymatic calorimetric testing after overnight fasting on the day after admission. The low-density lipoprotein cholesterol was calculated using the Friedewald formula. A coordinator at each hospital entered data collected from each institution into a standardized computerized database provided by the KCAR committee. The data coordinators attended meetings four times a year; at the meetings, the study protocol was reviewed and discussed. From March 1999 to December 2005, 6,549 patients were registered into the database. All patients were divided into three groups according to age: young patients, Ōēż40 (n=134), middle-aged patients, 41-70 (n=4451) and older patients, Ōēź71 (n=1778). We compared the baseline clinical characteristics and angiographic findings among these groups.
Based on the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC) VII guidelines, hypertension was defined as known hypertension or a blood pressure (BP) Ōēź140/90 mmHg5). The diagnosis of diabetes mellitus was based on fasting plasma glucose levels Ōēź126 mg per dL (7.0 mmol per L) or two-hour postprandial plasma glucose (2hrPPG) readings Ōēź200 mg per dL (11.1 mmol per L)6). The metabolic syndrome was defined according to a modification of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)7). Since the cutoff values for the definition of obesity in Asian populations have been revised, the criteria for the metabolic syndrome was modified8). The metabolic syndrome was diagnosed if three or more of the following were present: (a) Obesity defined by a body mass index >25 kg/m2 (b) hypertriglyceridemia if the TG Ōēź150 mg/dL (c) low HDL-C : HDL-C<40 mg/dL in men or <50 mg/dL in women (d) hypertension as known hypertension or a BP Ōēź130/85 mmHg and (e) dysglycemia was defined as known diabetes (DM) or a fasting plasma glucose Ōēź110 mg/dL. Cardiac syndrome X was present in patients with typical exertional chest pain, a positive response to stress testing and normal coronary angiograms.
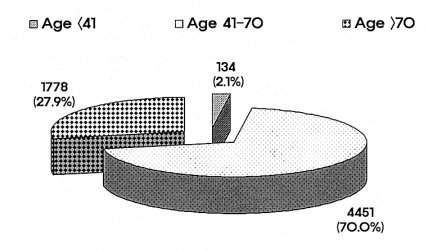
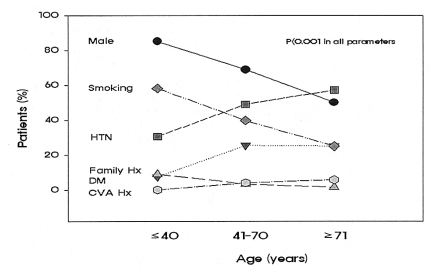
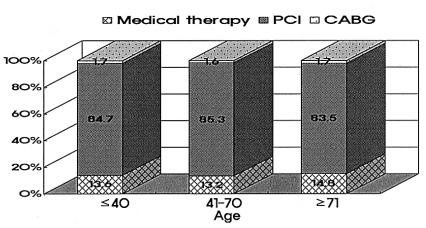
Of the 6,349 patients enrolled: 70% of the patients were in the 41-70 age group 2.1% in the Ōēż40 age group, and 27.9% in the Ōēź71 age group (Figure 1). The Ōēż40 age group had a higher number of males than the 41-70 and Ōēź71 age groups (85.1%, 68.9% and 50.1%, respectively, p<0.01). Furthermore, the 40 age group had a higher frequency of smoking and family history of ischemic heart disease than did the other groups (p<0.01, respectively). However, the over 41 age groups had a higher frequency of age-related risk factors such as diabetes mellitus, hypertension and stroke than did the Ōēż40 age group (p<0.01, respectively) (Table 1) (Figure 2).
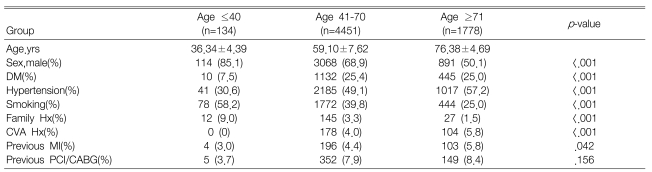
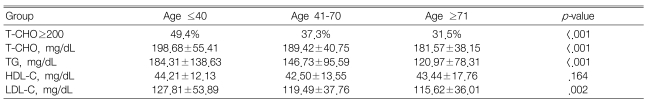
Hypercholesterolemia defined as a serum total cholesterol 200 mg/dL or more was more common in the Ōēż40 age group than in the 41-70 and Ōēź71 age groups (49.4%, 37.3% and 31.5%, respectively, p<0.01). The levels of total cholesterol, triglycerides and LDL-C were significantly higher in younger patients than in the older patients. However, the HDL-C was not significantly different among the three groups (Table 2). To determine the frequency and contributing factors for the metabolic syndrome, all risk factors were identified and compared in the different groups; the metabolic syndrome for the total study population was identified in 55% of the Ōēż40, 66% of the 41-70 and 57% of the Ōēź71. The highest prevalence of the metabolic syndrome was in the middle age group (p<0.001) (Table 3). The frequency of contributing factors for the metabolic syndrome, according to age group was analyzed. In the Ōēż40 age group, obesity (79%) and hypertension (79%) were the most common contributing factors identified for the metabolic syndrome; hypertension and high fasting glucose were the most common contributing factors in the older age groups (Table 3).
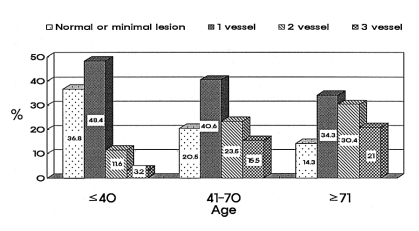
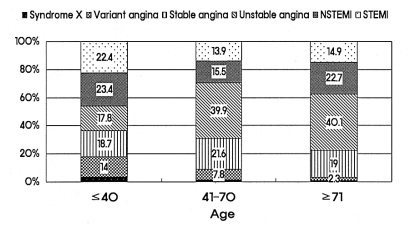
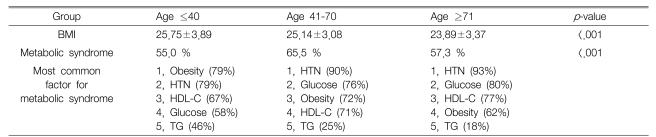
Coronary angiography showed normal or minimal stenosis in 37% and one vessel disease in 48% in the Ōēż40 age group. The prevalence of multivessel disease was dramatically increased with advancing age; 51% of the patients had more than two vessel disease in the Ōēź71 age group (Figure 3). Young patients frequently presented with a myocardial infarction (MI), non-ST elevated MI (23%) and ST elevated MI (22%). However, older patients were most frequently admitted with unstable or stable angina (Figure 4). The treatment modalities were not different among the different age groups. About 13~14% of patients were treated by medication only. Percutaneous coronary intervention (PCI) was performed in more than 80% of the patients in each group. Coronary artery bypass graft surgery (CABG) was performed in 1.7% of all patients (Figure 5).
In this multicenter registry based study of 6,549 patients hospitalized for ischemic heart disease, we found age-related variations in epidemiologic characteristics and clinical presentation. This is the first large scale study evaluating the epidemiologic features of ischemic heart disease in the Korean population.
The age group of 65 and over is currently the fastest growing age group in Korea; ischemic heart disease is an age-related disease and its prevalence is increasing with the aging population. Race and socioeconomic status are also associated with the prevalence and clinical outcome of ischemic heart disease9). The risk factors associated with atherosclerotic disease are different in elderly patients when compared to younger patients10). However, currently we do not have sufficient data to assess the specific risk factors contributing to the development of ischemic heart disease in the Korean population. In this study, we analyzed epidemiologic and clinical data from patients with ischemic heart disease who were treated at seven Korean university hospitals.
We analyzed epidemiologic variables in three different age groups. For the younger patients we found a higher frequency of males than in the older patients; the gender differences equalized after 70, similar to the data from Western countries11, 12). The menopausal age of Korean women is on average 4913). This suggests that the antiatherogenic effects associated with female gender are no longer present by about 20 years after menopause. The smoking rate was 58% in the younger age group, and it dropped to 25% in the old patient group. Therefore, smoking is still a major risk factor for coronary artery disease in young Korean males. However, the older group showed a higher prevalence of age related diseases such as hypertension and diabetes.
As for the lipid profiles, the younger patients had dyslipidemia more commonly than the older patients did. This may have been related to the higher incidence of obesity in the younger patients. This also suggests the possibility of a genetic predisposition related to the metabolic abnormalities observed in younger patients.
Recently, the clinical significance of the metabolic syndrome for the development of cardiovascular disease has been emphasized; the prevalence of metabolic components such as high blood sugar, obesity and hypertension are increasing in Korea. The incidence of the metabolic syndrome depends on the definition used14, 15). In this study, the definition introduced by the National Cholesterol Education Program (NCEP) Expert Panel was used16). The definition of obesity was modified according to the Asian criteria developed for the body mass index (BMI) Ōēź25 kg/m2 8). It is well known that the prevalence of the metabolic syndrome, in the general population, varies based on race, gender and geographic region. The prevalence of the metabolic syndrome, in Korea, using the ATP III-BMI25 definition was reported to be 13%, based on Korean health data17), which included 20.1% men and 23.9% women from the Korean nutritional health survey18). In this study, the prevalence of the different components of the metabolic syndrome differed by age group. For the less than 40 group, obesity was the most common contributing factor. However, for the older groups age-related factors such as hypertension and diabetes were the most frequent factors.
The angiographic severity of coronary artery disease appears to differ in younger patients compared to the older patients; the younger patients showed a preponderance of normal findings, minimal lesions or single-vessel disease. For the Ōēź71 age group there was a significantly higher prevalence of three-vessel disease, up to 21%.
Recently, with improvements in coronary intervention and surgical skills, treatment is available at any age. However, our data showed that older patients were less likely to undergo percutaneous coronary intervention or bypass surgery during their hospital admission1, 19); although the medical treatment options were similar for the different age groups. In routine clinical practice in Korea, about 84% of patients with ischemic heart disease and significant coronary artery stenosis have percutaneous coronary intervention.
The limitations of this study included the following: not all clinical parameters were routinely noted and the treating physician recorded most of the diagnostic criteria; since we intended to determine general patient patterns in Korea, site selection was not random.
In conclusion, the KCAR study provides important information on age-related trends in the epidemiologic characteristics of ischemic heart disease in Korea. Coronary artery disease in younger adults showed different demographic characteristics and different clinical presentation compared to older patients.
References
1. Yan RT, Yan AT, Tan M, Chow CM, Fitchett DH, Ervin FL, Cha JY, Langer A, Goodman SG. Age-related differences in the management and outcome of patients with acute coronary syndromes. Am Heart J 2006. 151:352ŌĆō359PMID : 16442898.


2. Shiraishi J, Kohno Y, Yamaguchi S, Arihara M, Hadase M, Hyogo M, Yagi T, Shima T, Sawada T, Tatsumi T, Azuma A, Matsubara H. Medium-term prognosis of young Japanese adults having acute myocardial infarction. Circ J 2006. 70:518ŌĆō524PMID : 16636483.


3. Katzel LI, Sorkin KD, Colman E, Goldberg AP, Busby-Whitehead MJ, Lakatta LE, Becker LC, Lakatta EG, Fleg JL. Risk factors for exercise-induced silent myocardial ischemia in healthy volunteers. Am J Cardiol 1994. 74:869ŌĆō874PMID : 7977116.


4. Avendano M, Kunst AE, Huisman M, Lenthe FV, Bopp M, Regidor E, Glickman M, Costa G, Spadea T, Deboosere P, Borrell C, Valkonen T, Gisser R, Borgan JK, Gadeyne S, Mackenbach JP. Socioeconomic status and ischaemic heart disease mortality in 10 western European populations during the 1990s. Heart 2006. 92:461ŌĆō467PMID : 16216862.



5. Chaturvedi S. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): is it really practical? Natl Med J India 2004. 17:227. PMID : 15372777.
6. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997. 20:1183ŌĆō1197PMID : 9203460.



7. The National Cholesterol Education Program. Executive summary of the third report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001. 285:2486ŌĆō2497PMID : 11368702.


8. Ko GT, Cockram CS, Chow CC, Yeung V, Chan WB, So WY, Chan NN, Chan JC. High prevalence of metabolic syndrome in Hong Kong Chinese: comparison of three diagnostic criteria. Diabetes Res Clin Pract 2005. 69:160ŌĆō168PMID : 16005365.


9. Suchday S, Krantz DS, Gottdiener JS. Relationship of socioeconomic markers to daily life ischemia and blood pressure reactivity in coronary artery disease patients. Ann Behav Med 2005. 30:74ŌĆō84PMID : 16097908.


10. Woo J, Lau E, Kay R. Elderly subjects aged 70 years and above have different risk factors for ischemic and hemorrhagic strokes compared to younger subjects. J Am Geriatr Soc 1992. 40:124ŌĆō129PMID : 1531486.


11. Gorodeski GI. Impact of the menopause on the epidemiology and risk factors of coronary artery heart disease in women. Exp Gerontol 1994. 29:357ŌĆō375PMID : 7925756.


12. Robinson K, Conroy RM, Mulcahy R. Risk factors and in-hospital course of first myocardial infarction in the elderly. Clin Cardiol 1988. 11:519ŌĆō523PMID : 3168336.


13. Park YJ, Gu BS, Kang HC, Chon SH, Yoon JW. The menopausal age and climacteric symptoms, and the related factors of Korean women. Korean J Women Health Nurs 2001. 7:473ŌĆō485.

14. Yilmaz MB, Guray Y, Guray U, Biyikoglu SF, Tandogan I, Korkmaz S. Metabolic syndrome increases the risk of significant coronary artery involvement in patients with peripheral artery disease. Coron Artery Dis 2006. 17:529ŌĆō532PMID : 16905965.


15. Schoenhagen P, Nissen SE. Identification of the metabolic syndrome and imaging of subclinical coronary artery disease: early markers of cardiovascular risk. J Cardiovasc Nurs 2006. 21:291ŌĆō297PMID : 16823283.


16. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002. 106:3143ŌĆō3421PMID : 12485966.


17. Shiwaku K, Nogi A, Kitajima K, Anuurad E, Enkhmaa B, Yamasaki M, Kim JM, Kim IS, Lee SK, Oyunsuren T, Yamane Y. Prevalence of the metabolic syndrome using the modified ATP III definitions for workers in Japan, Korea and Mongolia. J Occup Health 2005. 47:126ŌĆō135PMID : 15824477.


18. Park HS, Oh SW, Kang JH, Park YW, Choi JM, Kim YS, Choi WH, Yoo HJ, Kim YS. Prevalence and Associated Factors with Metabolic Syndrome in South Korea. J Korean Soc Study Obes 2003. 12:1ŌĆō14.
Figure┬Ā1
Age distribution of the study patients. About one third of the patients were older >70; patients <41 accounted for only 2.1%.
Figure┬Ā2
The prevalence of risk factors for ischemic heart disease. While younger patients showed a higher prevalence of male gender and smoking, older patients had a higher incidence of diabetes and hypertension. HTN, hypertension; DM, diabetes mellitus; CVA, cerebrovascular accident.
Figure┬Ā3
The distribution of the extent of coronary artery disease. Most of the younger patients showed minimal stenosis or significant stenosis in one vessel. Coronary atherosclerosis was extensive in older patients as revealed by the higher incidence of 2 or 3 vessel disease.
Figure┬Ā4
Distribution of clinical presentation of ischemic heart disease. Younger patients were more likely to present with myocardial infarction than older patients were. NSTEMI, non ST-segment elevated myocardial infarction; STEMI, ST-segment elevated myocardial infarction.
Figure┬Ā5
In-hospital management of significant coronary artery stenosis (Ōēź=50% diameter stenosis) by different ages (n=5150). The treatment strategies were similar for all age groups. About 84% of ischemic heart disease patients with significant stenosis of the coronary artery were treated with percutaneous coronary intervention. PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft surgery.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



