1. Sarin SK, Kumar A. Gastric varices: profile, classification, and management. Am J Gastroenterol 1989;84:1244ŌĆō1249PMID : 2679046.


2. News notes. Can Vet J 1960;1:330ŌĆō332PMID : 17421208.


3. Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology 1992;16:1343ŌĆō1349PMID : 1446890.


4. Sarin SK. Long-term follow-up of gastric variceal sclerotherapy: an eleven-year experience. Gastrointest Endosc 1997;46:8ŌĆō14PMID : 9260698.


5. Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W. Practice Guidelines Committee of the American Association for the Study of Liver Diseases. Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922ŌĆō938PMID : 17879356.


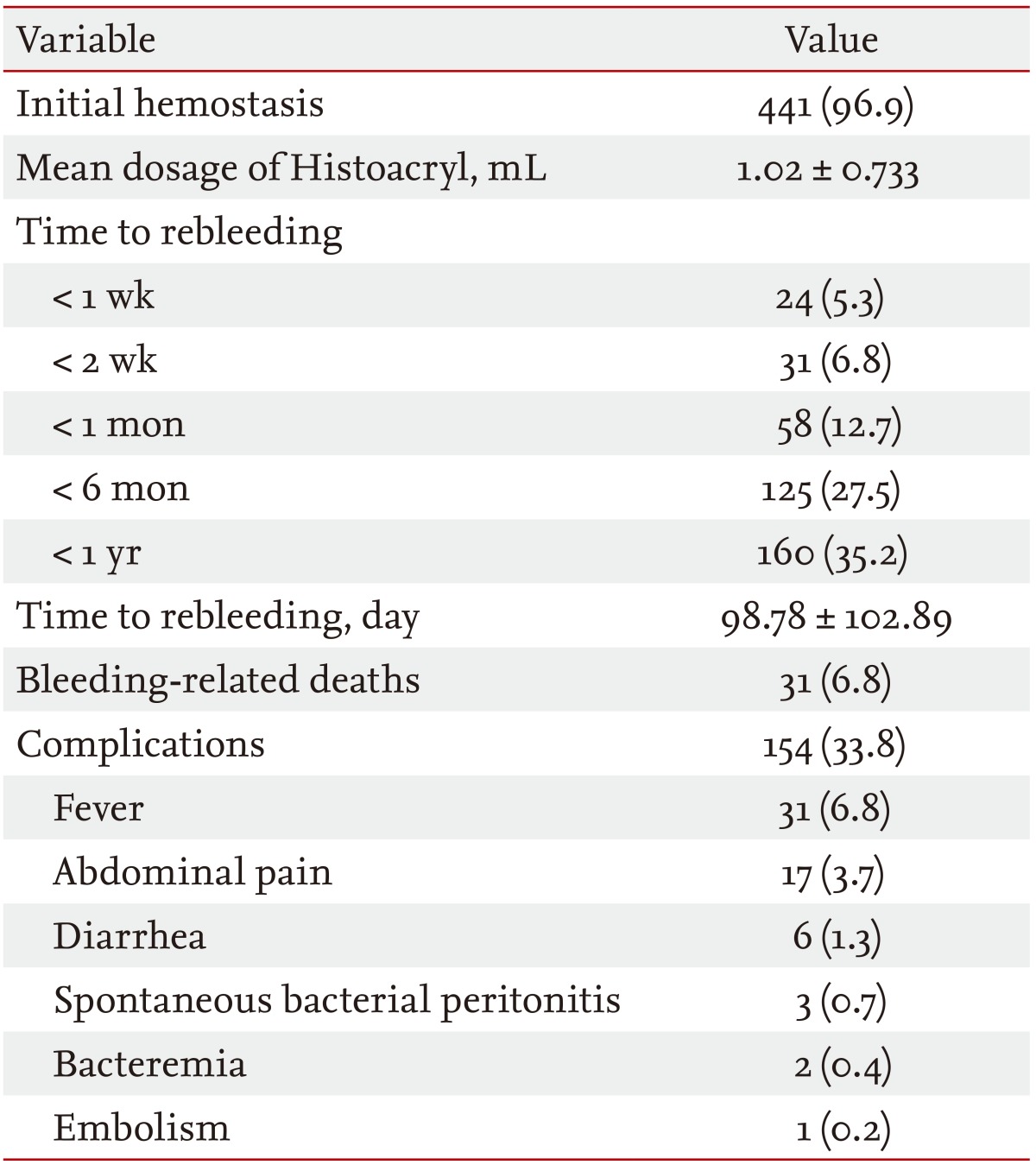
6. Huang YH, Yeh HZ, Chen GH, et al. Endoscopic treatment of bleeding gastric varices by N-butyl-2-cyanoacrylate (Histoacryl) injection: long-term efficacy and safety. Gastrointest Endosc 2000;52:160ŌĆō167PMID : 10922085.


7. Soehendra N, Nam VC, Grimm H, Kempeneers I. Endoscopic obliteration of large esophagogastric varices with bucrylate. Endoscopy 1986;18:25ŌĆō26PMID : 3512261.


9. Fry LC, Neumann H, Olano C, Malfertheiner P, Monkemuller K. Efficacy, complications and clinical outcomes of endoscopic sclerotherapy with N-butyl-2-cyanoacrylate for bleeding gastric varices. Dig Dis 2008;26:300ŌĆō303PMID : 19188718.


10. Akahoshi T, Hashizume M, Shimabukuro R, et al. Long-term results of endoscopic Histoacryl injection sclerotherapy for gastric variceal bleeding: a 10-year experience. Surgery 2002;131(1 Suppl):S176ŌĆōS181PMID : 11821807.


11. Hashizume M, Kitano S, Yamaga H, Koyanagi N, Sugimachi K. Endoscopic classification of gastric varices. Gastrointest Endosc 1990;36:276ŌĆō280PMID : 2365213.


12. Tan PC, Hou MC, Lin HC, et al. A randomized trial of endoscopic treatment of acute gastric variceal hemorrhage: N-butyl-2-cyanoacrylate injection versus band ligation. Hepatology 2006;43:690ŌĆō697PMID : 16557539.


13. de Franchis R, Primignani M. Natural history of portal hypertension in patients with cirrhosis. Clin Liver Dis 2001;5:645ŌĆō663PMID : 11565135.


14. Graham DY, Smith JL. The course of patients after variceal hemorrhage. Gastroenterology 1981;80:800ŌĆō809PMID : 6970703.


15. Smith JL, Graham DY. Variceal hemorrhage: a critical evaluation of survival analysis. Gastroenterology 1982;82(5 Pt 1):968ŌĆō973PMID : 7037525.


16. Soares-Weiser K, Brezis M, Tur-Kaspa R, Leibovici L. Antibiotic prophylaxis for cirrhotic patients with gastrointestinal bleeding. Cochrane Database Syst Rev 2002;(2):CD002907. PMID : 12076458.


17. D'Amico G, De Franchis R. Cooperative Study Group. Upper digestive bleeding in cirrhosis: post-therapeutic outcome and prognostic indicators. Hepatology 2003;38:599ŌĆō612PMID : 12939586.


19. Kind R, Guglielmi A, Rodella L, et al. Bucrylate treatment of bleeding gastric varices: 12 years' experience. Endoscopy 2000;32:512ŌĆō519PMID : 10917182.


20. Nguyen AJ, Baron TH, Burgart LJ, Leontovich O, Rajan E, Gostout CJ. 2-Octyl-cyanoacrylate (Dermabond), a new glue for variceal injection therapy: results of a preliminary animal study. Gastrointest Endosc 2002;55:572ŌĆō575PMID : 11923777.


21. Kim T, Shijo H, Kokawa H, et al. Risk factors for hemorrhage from gastric fundal varices. Hepatology 1997;25:307ŌĆō312PMID : 9021939.


22. Monsanto P, Almeida N, Rosa A, et al. Endoscopic treatment of bleeding gastric varices with histoacryl (N-butyl-2-cyanoacrylate): a South European single center experience. Indian J Gastroenterol 2013;32:227ŌĆō231PMID : 22766643.


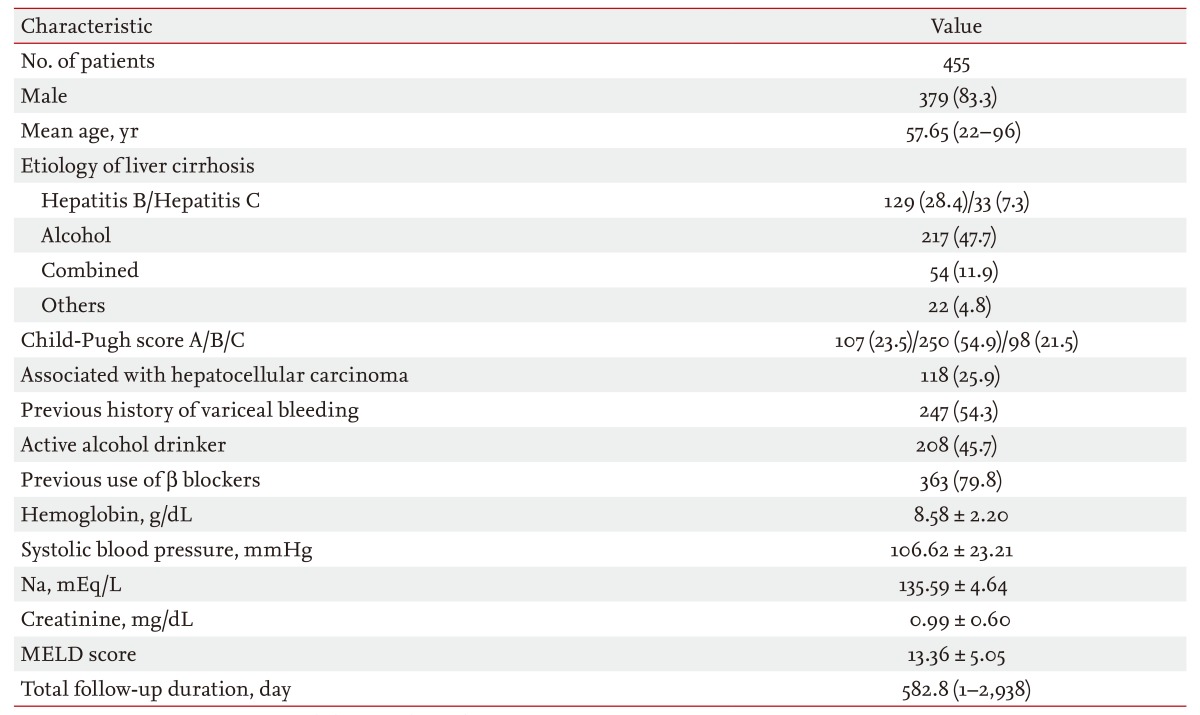
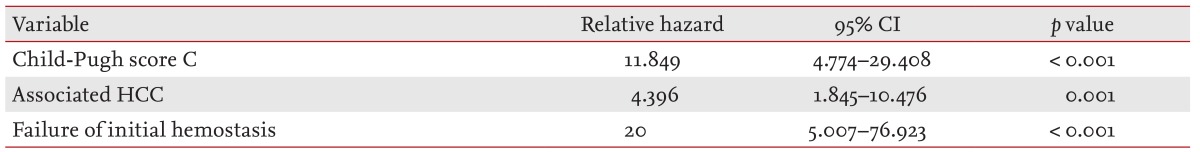
23. Lee JY, Lee JH, Kim SJ, et al. Comparison of predictive factors related to the mortality and rebleeding caused by variceal bleeding: Child-Pugh score, MELD score, and Rockall score. Korean J Hepatol 2002;8:458ŌĆō464.
24. Bambha K, Kim WR, Pedersen R, Bida JP, Kremers WK, Kamath PS. Predictors of early re-bleeding and mortality after acute variceal haemorrhage in patients with cirrhosis. Gut 2008;57:814ŌĆō820PMID : 18250126.


25. Chalasani N, Kahi C, Francois F, et al. Model for end-stage liver disease (MELD) for predicting mortality in patients with acute variceal bleeding. Hepatology 2002;35:1282ŌĆō1284PMID : 11981782.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





