To the Editor,
Acute right heart failure is caused commonly by acute right ventricular (RV) pressure overload from acute pulmonary thromboembolism, acute RV infarction, or acute exacerbation of preexisting RV failure from various causes [1]. However, acute right heart failure due to acute RV volume overload caused by arteriovenous fistula (AVF) between the brachiocephalic artery (BCA) and left brachiocephalic vein (BCV) has been described rarely.
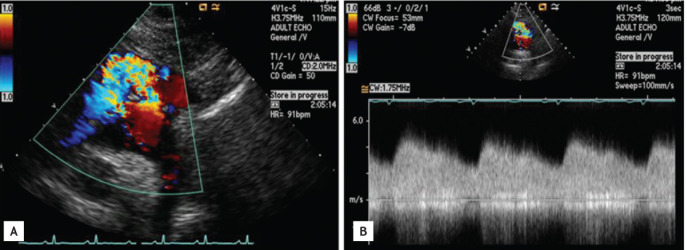
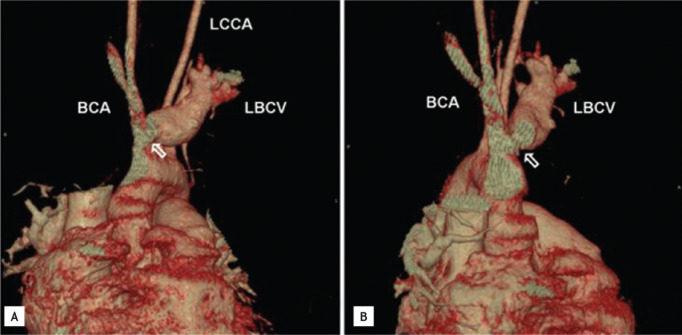
A 37-year-old female presented to our institution with a sudden onset of left arm and facial swelling, worsening fatigue, jaundice, and abdominal discomfort accompanied by an elevation in liver enzymes (aspartate aminotransferase, 582 U/L; alanine aminotransferase, 610 U/L; and bilirubin, 7.4 mg/dL). She underwent orthopedic surgery at a private clinic 2 weeks prior for dislocation of the left sternoclavicular joint caused by a traffic accident. Left arm and facial swelling developed suddenly the day following her surgery and had not improved despite 2 weeks of medical treatment. Upon admission icteric sclera, jugular venous distension, hepatomegaly, leg edema, and f luid waves on the abdomen were noted. A previously overlooked continuous murmur with thrill was heard along the left upper sternal border and suprasternal notch. A chest roentgenogram revealed bulging of the right cardiac border, and electrocardiography revealed sinus tachycardia, enlarged RV size, tricuspid regurgitation with a peak velocity of 2.9 m/sec, and persistently dilated inferior vena cava. No abnormal findings explaining these irregularities were noted upon cardiac examination. However, abnormal continuous f low with a peak velocity of 4.7 m/sec from BCA to the venous structure was noted in the suprasternal window (Fig. 1). Computed tomographic angiography (CTA) showed no abnormal findings in the pulmonary artery and demonstrated the AVF between BCA and left BCV near the previous surgery site (Fig. 2). We concluded that iatrogenic AVF might be the cause of acute right heart failure and congestive hepatopathy. The patient underwent corrective surgery for the AVF and the operative finding was identical to those of CTA. The patient recovered and was discharged following corrective surgery.
AVF is an abnormal connection between the arterial and venous system that may be congenital or acquired [2]. With the increase in various diagnostic, interventional, or surgical procedures, the incidence of the iatrogenic AVF has increased [3]. The symptoms of AVF range from asymptomatic to mildly symptomatic depending on their location and the blood vessels involved, but may cause serious problems such as myocardial or cerebral ischemia, high output cardiac failure, or death [2].
Although AVF may develop in any location, the formation of AVF between the BCA and left BCV is extremely rare and few cases have been described [4,5]. Duara et al. [4] reported a case of AVF between the BCA and left innominate vein following median sternotomy for surgery of an atrial septal defect. Clarkson et al. [5] also reported a case of right brachiocephalic AVF, which was made initially as the vascular route for hemodialysis, but the fistula chronically induced pulmonary hypertension, RV enlargement, and tricuspid regurgitation for 2 years and these complications were reversed following corrective surgery. The clinical manifestations of the present case were similar to those of the case reported by Clarkson et al. [5] except that the onset of right heart failure was acute and combined with congestive hepatopathy. The acute onset of left arm and facial swelling was also a unique feature of this case, and was possibly caused by the backward transmission of shunt flow to the left sided venous system. To our knowledge, this is the first case of acute right heart failure and congestive hepatopathy caused by AVF between the BCA and left BCV following orthopedic surgery. Therefore, health care providers should keep in mind these potential complications of AVF, particularly in a patient with unexplained heart failure who has undergone recent or remote invasive medical procedures.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





