 |
 |
| Korean J Intern Med > Volume 29(5); 2014 > Article |
|
To the Editor,
Acute aortic occlusion by a thrombus is an uncommon vascular emergency during percutaneous coronary intervention (PCI), which may lead to shock and death. We report on a patient who experienced acute thrombosis at the aortoiliac bifurcation and was treated by aspirating a thrombus and implanting a stent in the aorta.
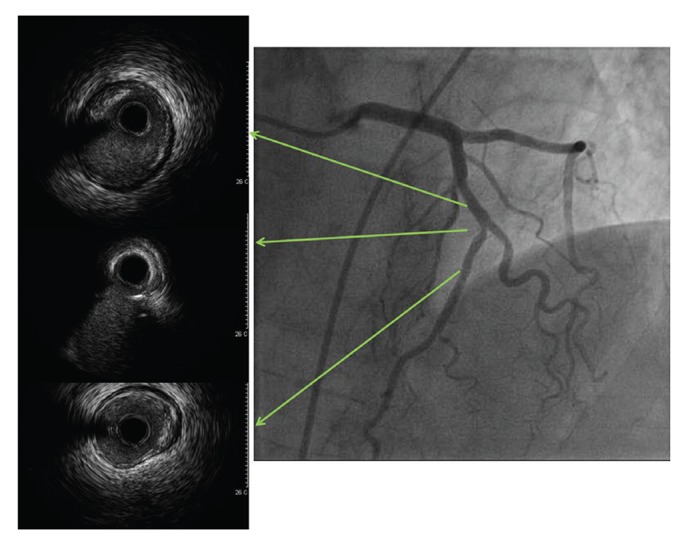
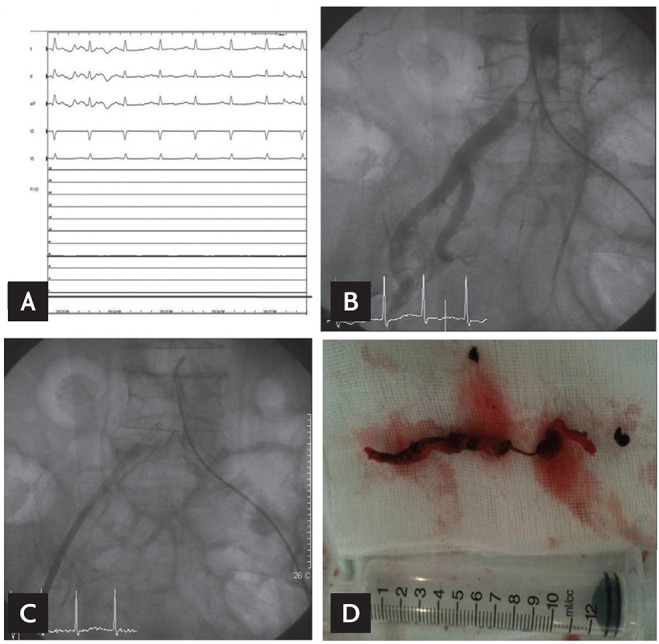
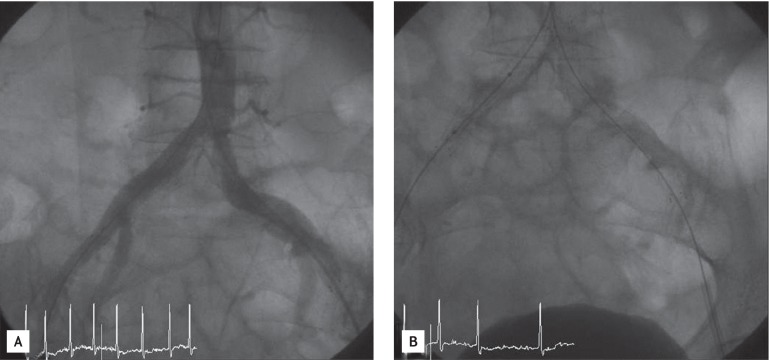
An 82-year-old female with a history of hypertension, diabetes, atrial fibrillation, and cerebral infarction was referred to the Cardiology Department due to chest discomfort and elevated cardiac biomarkers (creatinine kinase/creatinine kinase-MB, 33/7.0 IU/L; troponin I, 0.18 ng/mL) before a colorectal fistula operation. Coronary angiography was performed under the impression of a non-ST elevation myocardial infarction, which clearly showed a high-grade stenosis in the mid-portion of the left anterior descending (LAD) artery with minimal luminal area < 2 mm2 on the intravascular ultrasound evaluation (Fig. 1). Unfractionated heparin (70 units/kg) was administered initially. Then, activated clotting time was monitored and maintained at 200 to 300 seconds by an additional injection of heparin during PCI. When a guiding catheter (JL 7 Fr) was engaged into the LAD artery, central blood pressure decreased and unusual flat pattern pressure curves appeared, together with dizziness (Fig. 2A). We retracted the guiding catheter and performed aortography through the contralateral femoral artery. No aortic dissection was detected in the ascending or descending aorta. However, aortography showed a huge, lumen-occluding thrombi at the level of aortoiliac bifurcation (Fig. 2B). We initially infused 200,000 U tissue plasminogen activator into the aortic bifurcation through the guiding catheter and manually aspirated using a 9-Fr long sheath, but huge thrombi remained in the aortoiliac bifurcation, and an angiogram showed no pathological evidence of abdominal aorta bifurcation such as severe occlusive disease, aortic dissection, or abdominal aortic aneurysm (Fig. 2C). The aspirated material was a 6-cm black-colored thrombus (Fig. 2D). We inserted a stent in the aorta and two self-expandable aortic stents (10 mm ├Ś 6 cm at the left side and 10 mm ├Ś 8 cm at the right side (Zilver, Cook Medical, Bloomington, IN, USA) were implanted at the aortoiliac bifurcation. After deployment of the stents, additional ballooning (8 mm ├Ś 4 cm, Rider, Cook Medical) was performed. A final angiogram showed a good result (Fig. 3). The patient recovered well after stent implantation, with blood pressure of 110/70 mmHg. She underwent PCI successfully at the mid-LAD artery and was discharged uneventfully 7 days later.
Acute thrombotic occlusion of the aorta during PCI is a rare event, resulting in disastrous consequences unless an early diagnosis is made and appropriate management initiated [1]. The cause of an occlusion is a saddle embolus at the aortoiliac bifurcation or acute in situ thrombosis on a background of severe occlusive disease, aortic dissection, acute thrombosis of an abdominal aortic aneurysm, vasculitis, hypercoagulability, or aortic trauma [2]. Other uncommon causes include a fungal infection, acute thrombosis of abdominal aortic stent-graft in heparin-induced thrombocytopenia, or chemotherapy-related thrombosis [3,4,5].
Compared with other causes of acute aortic occlusion, acute thrombosis at the aortoiliac bifurcation during PCI is extremely rare. As a prerequisite check before guiding catheter engagement, we assessed the activated partial thromboplastin time and flushed the femoral sheath with saline, but no abnormal findings were detected. In this case, no abnormal findings in the aorta were observed, including aneurysm, dissection, or trauma. We also examined protein C and S activity, erythrocyte sedimentation rate, C-reactive protein, complement 3 and 4, and antineutrophil cytoplasmic antibody to evaluate hypercoagulability and vasculitis, but no abnormal results were found. No fungal infection was identified. Atrial fibrillation was another possible contributor to embolic occlusion but there was no thrombus in the left atrial appendage or left ventricle on echocardiography. Therefore, we finally suspected a saddle embolus originating from the femoral sheath and an in situ thrombosis at the aortoiliac bifurcation as a possible cause of this PCI-related aortic complication.
Anticoagulation should be initiated immediately once the diagnosis of acute thrombotic occlusion in aorta is made, and early revascularization should be the goal. Possible revascularization approaches include thromboembolectomy, aortic reconstruction, anatomic or extra-anatomic bypass, and thrombolysis. The choice of approach depends on the etiology, anatomy, and patient factors. Surgical thrombectomy has frequently been used for treatment of an acute aortic occlusion. However, recent advances in endovascular techniques could decrease the high mortality rate associated with surgical treatment of this disease and warrants consideration as a treatment option. In this case, we decided on endovascular treatment for revascularization with thrombolysis, thrombus aspiration, and stent implantation using a contralateral approach.
In conclusion, acute thrombosis can occur at the aortoiliac bifurcation during PCI. Therefore, operators should pay attention to the development of aortic complications upon encountering an abnormal central blood pressure pattern and consider an appropriate treatment method-including an endovascular approach-for acute aortic thrombosis.
References
1. Dossa CD, Shepard AD, Reddy DJ, et al. Acute aortic occlusion: a 40-year experience. Arch Surg 1994;129:603ŌĆō607PMID : 8204034.


2. Babu SC, Shah PM, Nitahara J. Acute aortic occlusion: factors that influence outcome. J Vasc Surg 1995;21:567ŌĆō572PMID : 7707562.


3. Kalayjian RC, Herzig RH, Cohen AM, Hutton MC. Thrombosis of the aorta caused by mucormycosis. South Med J 1988;81:1180ŌĆō1182PMID : 3420451.


Figure┬Ā1
Coronary angiogram and intravascular ultrasound examination showed significant stenosis in the mid left anterior descending artery.
Figure┬Ā2
(A) Blood pressure monitoring connected to a femoral sheath showed decreased aortic pressure, followed by appearance of unusual pressure curves of a flat-curved pattern. (B) Aortogram showed a huge and lumen-occluding thrombus at the aortoiliac bifurcation. (C, D) Thrombus removed by manual aspiration through a 9-Fr long sheath.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



