 |
 |
| Korean J Intern Med > Volume 30(1); 2015 > Article |
|
Abstract
Hypoglycemia is a major barrier to achieving the glycemic goal in patients with type 2 diabetes. In particular, severe hypoglycemia, which is defined as an event that requires the assistance of another person to actively administer carbohydrates, glucagon, or take other corrective actions, is a serious clinical concern in patients with diabetes. If severe hypoglycemia is not managed promptly, it can be life threatening. Hypoglycemia-associated autonomic failure (HAAF) is the main pathogenic mechanism behind severe hypoglycemia. Defective glucose counter-regulation (altered insulin secretion, glucagon secretion, and an attenuated increase in epinephrine during hypoglycemia) and a lack of awareness regarding hypoglycemia (attenuated sympathoadrenal activity) are common components of HAAF in patients with diabetes. There is considerable evidence that hypoglycemia is an independent risk factor for cardiovascular disease. In addition, hypoglycemia has a significant influence on the quality of life of patients with diabetes. To prevent hypoglycemic events, the setting of glycemic goals should be individualized, particularly in elderly individuals or patients with complicated or advanced type 2 diabetes. Patients at high-risk for the future development of severe hypoglycemia should be selected carefully, and intensive education with reinforcement should be implemented.
The dramatic and rapid increase in the number of people with type 2 diabetes worldwide is no longer surprising. Accordingly, strict glycemic control with lifestyle modifications has been emphasized to prevent microvascular and macrovascular diabetic complications [1,2]. However, three large clinical trials, Action in Diabetes and Vascular Disease (ADVANCE), Action to Control Cardiovascular Risk in Diabetes (ACCORD), and the Veterans Affairs Diabetes Trial, failed to demonstrate that intensive glucose control improved the primary cardiovascular outcomes in patients with type 2 diabetes [3,4,5]. In addition, patients who were assigned randomly into the intensive treatment group experienced more frequent episodes of hypoglycemia than did those assigned to the standard treatment group. Moreover, all three trials revealed that episodes of severe hypoglycemia were associated with an increased risk of subsequent mortality and morbidity [6].
Intensive glucose control is always accompanied by an increased risk of hypoglycemic episodes, and an increased incidence of hypoglycemic events is accompanied by direct and indirect health and economic burdens [7]. Hypoglycemic events, even if not severe, have negative effects on diabetes self-management, sleep quality, and the daily function of patients with both type 1 and type 2 diabetes [8]. The mean medical cost per severe hypoglycemic event was reported to be ~1.35-fold higher than the annual treatment cost for a patient with diabetes without complications in Korea [7]. Considering the indirect costs such as productivity, missed work, and the time lost by patients and their family members, the overall economic and social costs are huge. Therefore, the identification of measures to prevent hypoglycemia in patients with type 2 diabetes is needed urgently.
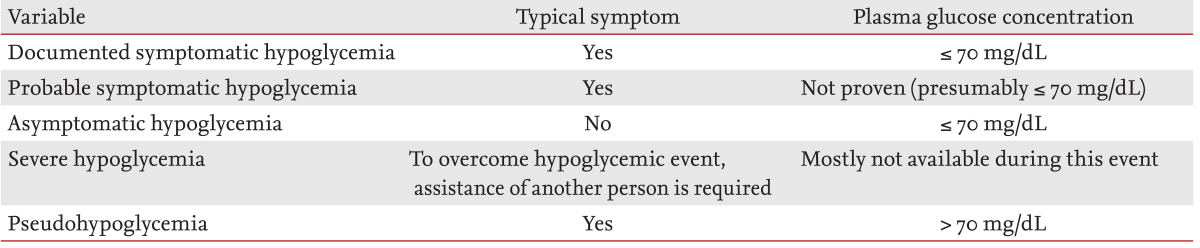
Hypoglycemia was described originally by Whipple, and is known as Whipple's triad: symptoms consistent of hypoglycemia, a low plasma glucose level, and relief of the symptoms when the plasma glucose concentration is raised [9]. Generally, a plasma glucose concentration ≤ 70 mg/dL is the cut-off value for the definition of hypoglycemia [10]. Because the glycemic thresholds for hypoglycemic symptoms could be lower in patients who experience recent antecedent hypoglycemia and higher in diabetic patients with uncontrolled plasma glucose concentrations [11,12], this simple biochemical cut-off method cannot be used to define hypoglycemia accurately, particularly in diabetic patients with recurrent or uncontrolled hyperglycemia. Hypoglycemic symptoms can occur in patients with biochemically normoglycemia or uncontrolled, prolonged hyperglycemia, even within the normoglycemic range [13].
According to a report by a workshop of the American Diabetes Association and the Endocrine Society, hypoglycemia in diabetes could be defined and classified as shown in Table 1 [10]. Among the categories of hypoglycemia hypoglycemia, severe hypoglycemia could be defined as an event that requires the assistance of another person to actively administer carbohydrates, glucagon, or take other corrective actions [10]. It is a serious clinical situation in subjects with both type 1 diabetes and advanced type 2 diabetes. If severe hypoglycemia is not managed promptly, it can be life threatening.
The brain uses glucose as its primary energy source. Under normal physiological conditions, the brain is unable to synthesize or store glucose and is vulnerable to glucose deprivation. Several physiological mechanisms have evolved to protect the integrity of the brain to respond to and limit the effects of hypoglycemia.
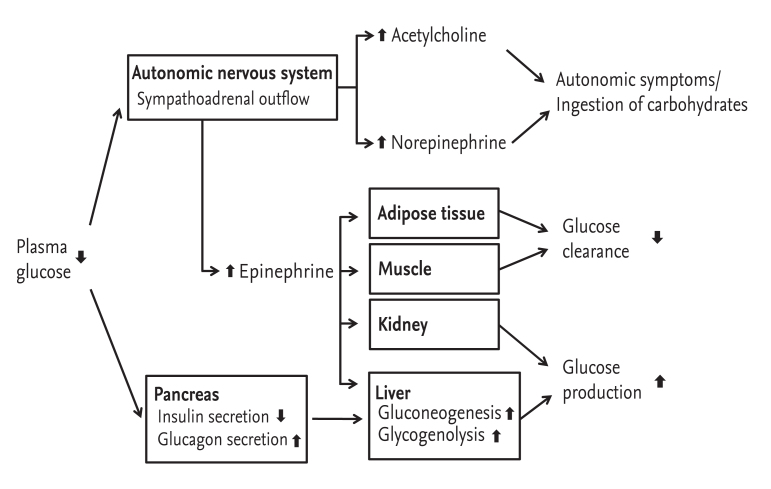
If blood glucose concentrations fall below the normal range, physiological defense mechanisms to overcome hypoglycemia become activated in nondiabetic individuals. This includes a consecutive decrease in insulin secretion, an increase in glucagon secretion and, in the absence of an increase in glucagon, enhanced secretion of adrenomedullary epinephrine (Fig. 1) [14]. The clinical symptoms and signs of hypoglycemia are derived from these counter-regulatory hormonal responses. The typical symptoms of hypoglycemia can be classified into two groups: autonomic (nervousness, anxiety, tremulousness, sweating, palpitation, shaking, dizziness, hunger, and tingling) and neuroglycopenic (confusion, weakness, tiredness, drowsiness, difficulty with concentration, speech difficulty, odd behavior, and incoordination) [15,16,17,18]. In serious cases stupor, seizure, coma, or death can occur. Diaphoresis, pallor, increased heat rate or systolic blood pressure, disorientation, hypothermia, and focal neurological deficits are often observed, but these symptoms are not specific to hypoglycemia; instead, they are the result of a perception of the physiological changes caused by the central nervous system-mediated sympathoadrenal discharge triggered by hypoglycemia [18].
The subjective recognition of the hypoglycemia is fundamental for effective patient self-management and preventing severe progression [19]. A lack of awareness of hypoglycemia can be defined as onset of the neuroglycopenic symptoms before the onset of autonomic warning symptoms [20]. If the sympathoadrenal response to hypoglycemia is delayed the autonomic warning symptoms are not recognized, which allows the patient to fall into severe neuroglycopenia (Fig. 2) [21]. Impaired autonomic symptoms during hypoglycemia are warning signs of hypoglycemic unawareness, and results in an ~6-fold higher frequency of severe hypoglycemia [22].
Patients with type 1 diabetes and long-standing type 2 diabetes with β-cell failure or absolute insulin deficiency have compromised defense mechanisms against hypoglycemia. This results in a lack of endogenous insulin secretion and subsequent glucagon secretion, and impaired epinephrine release (Fig. 2). Therefore, plasma glucose levels fall but hypoglycemic symptoms are absent, which reflects an attenuated sympathetic neural response [14,23].
In patients with hypoglycemia unawareness, the subjective responses to early hypoglycemia fail and so cognitive impairment is the first response [9]. Individual experience of severe hypoglycemia or a self-reported history of impaired perception of autonomic symptoms during hypoglycemia is important clue for diagnosing hypoglycemia unawareness [24,25,26,27]. It is largely the result of reduced sympathetic neural, rather than adrenomedullary, responses to hypoglycemia [28]. Hypoglycemia-associated autonomic failure is a functional disorder that differs from classical diabetic autonomic neuropathy, and is caused most frequently by recent antecedent hypoglycemia [29]. However, it is partly reversible by avoiding hypoglycemia [30,31], which restores the autonomic symptoms of hypoglycemia within 2 weeks, and reverses hypoglycemic unawareness by 3 months [24,31].
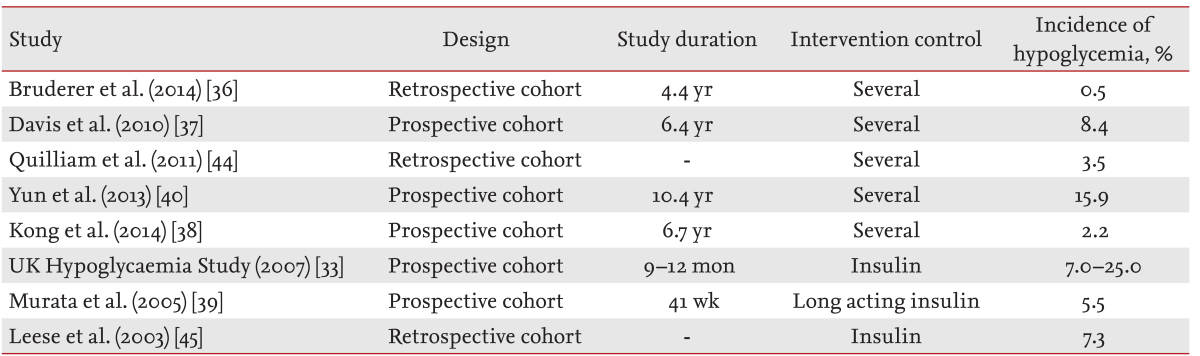
Non-severe hypoglycemia occurs commonly in patients with both type 1 and type 2 diabetes. A recent study by Wendel et al. [32] reported that 84% of individuals with type 2 diabetes experienced at least one hypoglycemic event, and that 42% of hypoglycemic episodes were asymptomatic. Severe hypoglycemia caused by glucose-lowering treatment (sulfonylurea, glinide, or insulin) occurs more frequently in type 1 than type 2 diabetes [33,34]. In a population-based study of type 1 diabetes, the overall rate of severe hypoglycemia was 1.3 episodes/patient-year (36.7% of subjects) [35]. The incidence of severe hypoglycemia in patients with type 2 diabetes has been reported to be 0.1 to 35 per 100 patient-years (Tables 2 and 3) [3,4,33,36,37,38,39,40,41,42,43,44,45]. In addition, the mean incidence of mild hypoglycemia was also reported to be 1 to 2 and 0.3 to 0.7 episodes/patient/week in patients with type 1 diabetes and insulin-treated type 2 diabetes, respectively [17]. However, the distribution of severe hypoglycemia is highly skewed, since 5% of subjects accounted for 54% of all episodes [35]. We reported recently that the incidence of severe hypoglycemia was 1.55 per 100 patient-years, and that ~25% of type 2 diabetic patients with severe hypoglycemic events experienced antecedent hypoglycemia within 3 to 6 months [40]. However, ethnic differences regarding the prevalence of hypoglycemic events are unknown.
Hypoglycemia can be fatal [46,47], and the increased mortality is mediated via an increased risk of cardiovascular death. In the ADVANCE and ACCORD trials, severe hypoglycemia was associated with a significantly increased risk of major cardiovascular events and a 1.4 to 3-fold higher risk of mortality [6,48]. Hypoglycemia changed cardiac repolarization and induced arrhythmias in patients with type 1 and type 2 diabetes [49,50,51]. The previously reported EURODIAB IDDM complication study demonstrated that severe hypoglycemia events were independently associated with a prolonged corrected QT (QTc) interval in type 1 diabetic patients [52]. A prolonged QTc interval reflects abnormalities in ventricular myocardial repolarization, and is an independent risk factor for mortality in patients with type 1 diabetes [53]. Similarly, myocardial ischemic changes with a prolonged QT interval have been also observed during insulin-induced hypoglycemia in patients with type 2 diabetes [49,50,54].
A study using a continuous glucose-monitoring device revealed that most hypoglycemic episodes occurred overnight (between 10:00 PM and 6:00 AM), and were not likely to result in recognized hypoglycemic symptoms [55]. During sleep the sympathoadrenal response to hypoglycemia is blunted [56]. Attenuated sympathoadrenal activity at night leads to compensatory activation of the parasympathetic system [17]. These factors contribute to induce ventricular arrhythmia, bradycardia, and atrial or ventricular ectopic beats during nighttime hypoglycemia [57].
The stress hormones that are secreted in response to hypoglycemia increase blood viscosity and promote coagulation, leading to endothelial dysfunction and the release of inflammatory cytokines into the circulation. The recovery from such an inflammatory response could take upto 1 week [17,58]. The cardiovascular outcome of patients who experience nighttime hypoglycemia might be related to the increased circulating levels of inflammatory markers, vascular adhesion molecules, and markers of thrombosis and platelet activation [59].
The effects of severe hypoglycemia on the structure and function of the brain have not been well defined. The ACCORD-MIND (ACCORD-Memory in Diabetes) MRI trial showed that severe symptomatic hypoglycemic events in treated type 2 diabetic patients were not associated with the accentuated loss of total brain volume and/or increased abnormal white matter volume compared with patients with type 2 diabetes without hypoglycemia [60]. However, a meta-analysis demonstrated that, compared with diabetic children without hypoglycemia, children with type 1 diabetes and recurrent severe hypoglycemia had slightly lower performance in some cognitive domains, including intelligence, memory, learning, and verbal fluency/language. The highest impairment was found in memory and learning [61]. In the Edinburgh Type 2 Diabetes Study, both the history and incidence of hypoglycemia were associated with a greater cognitive decline after adjusting for vascular risk factors and cardiovascular and microvascular disease [62]. Although there was a gross lack of structural changes in the brain, functional changes related to recurrent or severe hypoglycemic events should not be neglected and should be avoided.$
Hypoglycemia was a significant factor for the incidence of patient adherence to medication and glycemic control [63]. The fear of hypoglycemia might make many patients using insulin reluctant to use the recommended insulin dose or achieve the target range of glycemic control [64]. Individuals who experienced recent hypoglycemia, also reported an increased interference with social activities, missed work, work impairment, and decreased overall health-related quality of life [63]. Approximately one in seven patients with type 2 diabetes complained that they missed a work appointment or meeting or did not finish a task on time due to their recent non-severe nocturnal hypoglycemic events [8]. The loss of productivity was estimated to range from US $15 to $94 per non-severe hypoglycemic event, corresponding to 8.3 to 16 hours of lost work time per month and a mean 4.2 to 5.6 additional blood glucose test strips [7,65].
According to the recently published Hong Kong Diabetes Registry, cancer occurred more frequently among type 2 diabetic patients who experienced severe hypoglycemia. This suggests that severe hypoglycemia might reflect the coexistence of concurrent medical conditions that require additional clinical attention [66].
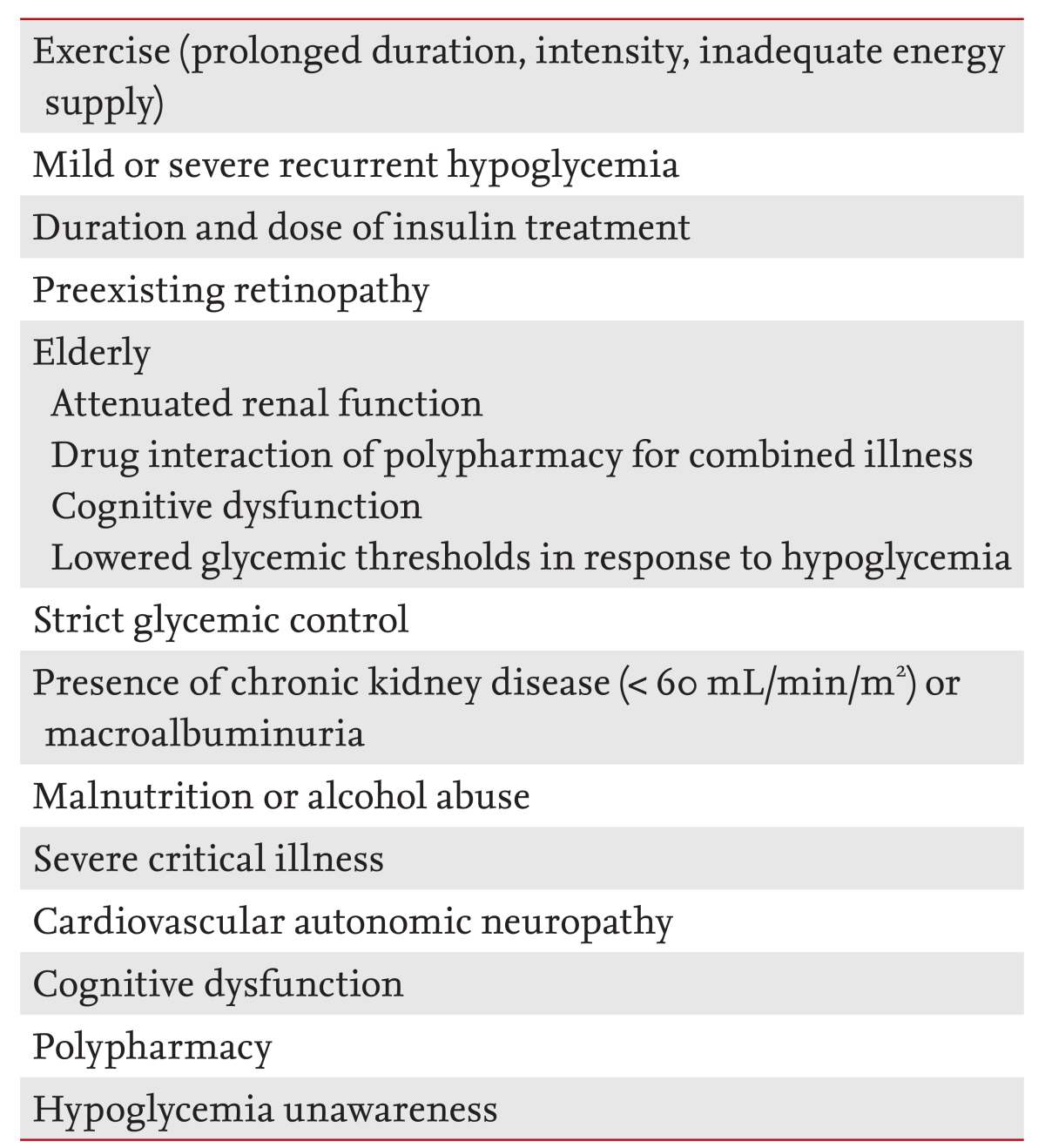
The causes of most hypoglycemic episodes are related to exercise, missing a meal or excessive dieting, and changes in medication; however, 56% of hypoglycemic events have an unknown cause [32]. The previous experience of hypoglycemia should be evaluated in all patients treated with insulin, sulfonylurea, or glinide. If patients complain of a history of recurrent hypoglycemia or hypoglycemia unawareness, they will require additional attention. Elderly diabetic patients, and individuals decreased performance in self-care activity, cognitive impairment, or advanced diabetic vascular complications are vulnerable to hypoglycemia, and the clinical outcomes of their hypoglycemic episodes are serious [67,68]. They also exhibit a higher risk of hypoglycemia that is associated with multiple medications and a reduced glycemic threshold in response to hypoglycemia. Diabetic patients with chronic kidney disease have a higher risk of hypoglycemia [66,69], due to the prolonged clearance of renal insulin or hypoglycemic agents and reduced renal gluconeogenesis (Table 4) [69].
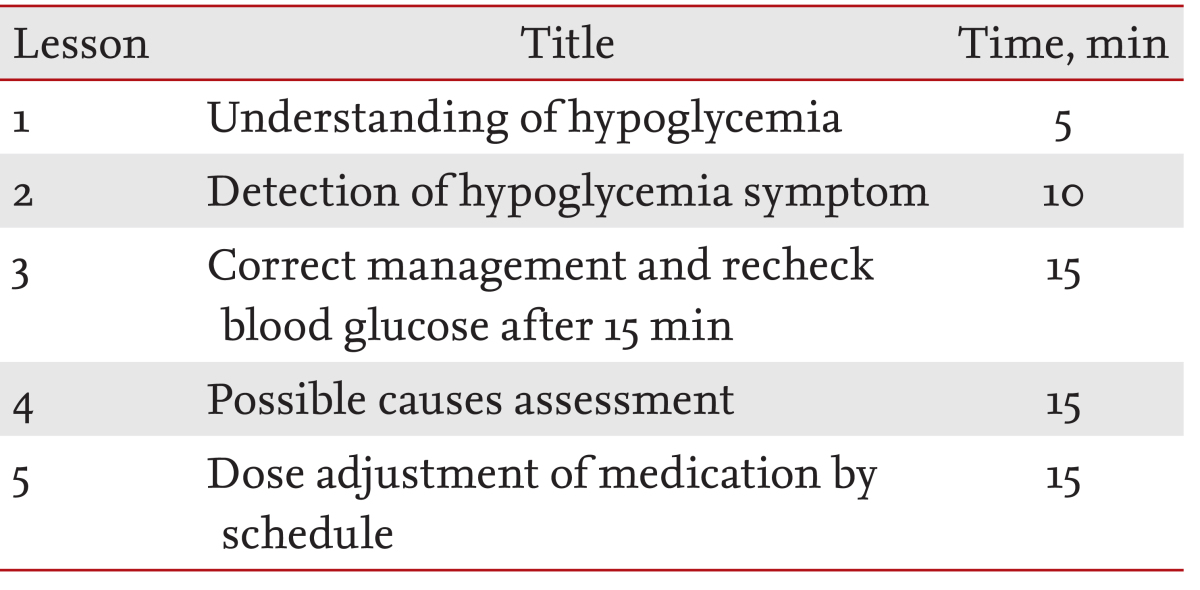
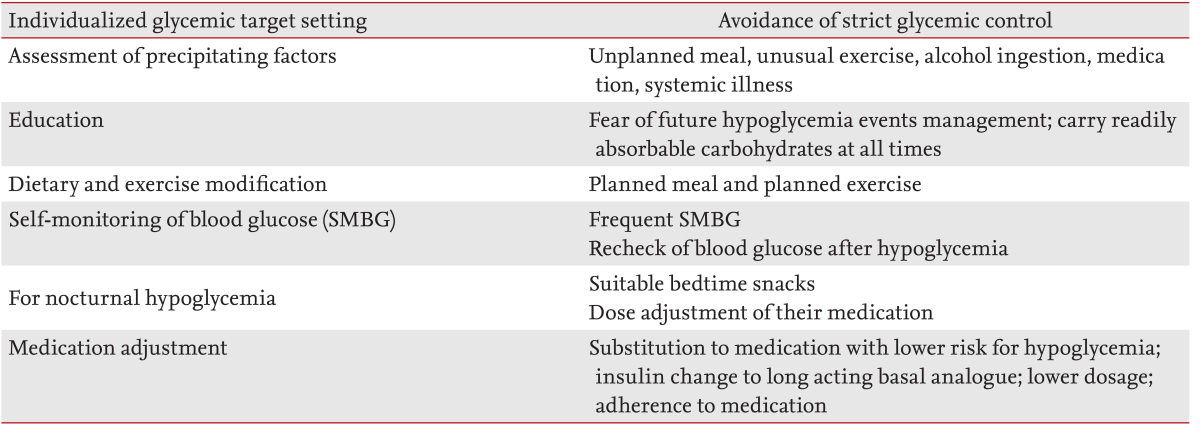
Structured diabetes education is an essential start for diabetes care [70]. Education is particularly important for patients with a higher risk of hypoglycemia. A structured education program can improve hypoglycemia awareness and the self-management ability of patients to reduce the incidence of hypoglycemia [71]. For intensive education, patients should be trained in hypoglycemia management skills, including the frequent self-monitoring of blood glucose (SMBG), glucose supplementation, re-checking blood glucose after a hypoglycemic episode, and dose adjustment of their medication. We found previously that intense individualized education programs improved the skills by which patients managed hypoglycemia as well as dose adjustment according to fasting glucose levels significantly [72]. In particular, education regarding the dose adjustment schedule for medications after a hypoglycemic event played an important role for preventing recurrent hypoglycemia. Similar to individualized glycemic goal setting according to the individual clinical situation, the educational curriculum and reinforcement should be individualized to focus on preventing hypoglycemia (Table 5).
Meal plans should also be individualized according to the patients' hypoglycemic medications. Patients taking long-acting sulfonylureas or a fixed insulin regimen are instructed not to skip or delay their meals. If patients are treated with postprandial insulin injections, the dose and meal times should be coupled [10]. Long-acting basal analogs, such as insulin glargine, insulin detemir, and insulin degludec, are preferable to neutral protamine Hagedorn because of their more physiological profiles and lower variability [73,74]. These analogs reduce the incidence of symptomatic hypoglycemic events by ~30% in patients with type 2 diabetes [74]. In addition, healthcare professionals should train patients to recognize and respond promptly to early neuroglycopenic symptoms [10].
SMBG using a point-of-care glucose meter is mandatory in patients at risk of hypoglycemia. Specifically, SMBG allows patients treated with glucose-lowering medication to detect hypoglycemic events, even in the absence of symptoms. In particular, nocturnal hypoglycemia can cause major problems with therapeutic management due to challenges with the detection and prevention [64,75]. Therefore, patients with nocturnal hypoglycemia, especially those with pre-existing ischemic heart disease or recurrent hypoglycemia, are encouraged to perform SMBG more frequently, and greater clinical attention is needed.
Elderly patients are at an increased risk of impaired renal function, cognitive impairment, and presenting with atypical hypoglycemic symptoms such as delirium or neurological events. Cognitive dysfunction is an important risk factor for hypoglycemia, and hypoglycemic events might further worsen cognitive function [76,77]. In older patients with poorly controlled diabetes, the most common barrier to achieving proper glycemic targets was inadequate medication caused by patient reluctance to make changes to their medication doses between clinical visits or during conditions such as illnesses [78]. Poor medication adherence in patients with type 2 diabetes and hypoglycemia might be caused by fear of further episodes of hypoglycemia [63]. Physicians educate and make recommendations to patients regarding self dose adjustment. Therefore, a practical approach that provides safe and helpful care using phone calls or more frequent patient contact is important. The total approach for type 2 diabetic patients with frequent hypoglycemia is summarized in Table 6.
The management of hypoglycemia is a critical clinical issue for patients with type 2 diabetes. If possible, hypoglycemia and severe hypoglycemia should be avoided in all patients with type 2 diabetes. However, a considerable number of diabetic patients are at risk of hypoglycemic episodes during their daily lives. Recurrent hypoglycemic or severe hypoglycemic attacks usually have unfavorable and serious clinical consequences; therefore, health care providers should recognize the risk of hypoglycemia and its clinical importance when making decisions. A considerable number of hypoglycemic episodes are asymptomatic and usually occur at night. Only a small number of patients experience multiple events of hypoglycemia, but these individuals might be prone to developing severe hypoglycemia. For patients at a higher risk of hypoglycemia glycemic goals should be determined according to their clinical situations. At the same time, diabetic education should be implemented promptly and appropriately.
References
1. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986PMID : 8366922.


2. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853PMID : 9742976.


3. Action to Control Cardiovascular Risk in Diabetes Study Group. Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–2559PMID : 18539917.



4. ADVANCE Collaborative Group. Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–2572PMID : 18539916.


5. Abraira C, Duckworth W, McCarren M, et al. Design of the cooperative study on glycemic control and complications in diabetes mellitus type 2: Veterans Affairs Diabetes Trial. J Diabetes Complications 2003;17:314–322PMID : 14583175.


6. Bonds DE, Miller ME, Bergenstal RM, et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the ACCORD study. BMJ 2010;340:b4909. PMID : 20061358.



7. Ha WC, Oh SJ, Kim JH, et al. Severe hypoglycemia is a serious complication and becoming an economic burden in diabetes. Diabetes Metab J 2012;36:280–284PMID : 22950059.



8. Brod M, Christensen T, Bushnell DM. Impact of nocturnal hypoglycemic events on diabetes management, sleep quality, and next-day function: results from a four-country survey. J Med Econ 2012;15:77–86PMID : 22029460.


9. Amiel SA, Dixon T, Mann R, Jameson K. Hypoglycaemia in type 2 diabetes. Diabet Med 2008;25:245–254PMID : 18215172.



10. Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care 2013;36:1384–1395PMID : 23589542.



11. Boyle PJ, Schwartz NS, Shah SD, Clutter WE, Cryer PE. Plasma glucose concentrations at the onset of hypoglycemic symptoms in patients with poorly controlled diabetes and in nondiabetics. N Engl J Med 1988;318:1487–1492PMID : 3285214.


12. Dagogo-Jack SE, Craft S, Cryer PE. Hypoglycemia-associated autonomic failure in insulin-dependent diabetes mellitus. Recent antecedent hypoglycemia reduces autonomic responses to, symptoms of, and defense against subsequent hypoglycemia. J Clin Invest 1993;91:819–828PMID : 8450063.



13. El Khoury M, Yousuf F, Martin V, Cohen RM. Pseudohypoglycemia: a cause for unreliable finger-stick glucose measurements. Endocr Pract 2008;14:337–339PMID : 18463040.


14. Cryer PE. Mechanisms of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med 2013;369:362–372PMID : 23883381.


15. Graveling AJ, Frier BM. Hypoglycaemia: an overview. Prim Care Diabetes 2009;3:131–139PMID : 19782016.


16. Henderson JN, Allen KV, Deary IJ, Frier BM. Hypoglycaemia in insulin-treated type 2 diabetes: frequency, symptoms and impaired awareness. Diabet Med 2003;20:1016–1021PMID : 14632703.


17. Frier BM. Hypoglycaemia in diabetes mellitus: epidemiology and clinical implications. Nat Rev Endocrinol 2014;10:711–722PMID : 25287289.


18. Tesfaye N, Seaquist ER. Neuroendocrine responses to hypoglycemia. Ann N Y Acad Sci 2010;1212:12–28PMID : 21039590.



19. McAulay V, Deary IJ, Frier BM. Symptoms of hypoglycaemia in people with diabetes. Diabet Med 2001;18:690–705PMID : 11606166.


20. Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care 2003;26:1902–1912PMID : 12766131.


21. Zammitt NN, Frier BM. Hypoglycemia in type 2 diabetes: pathophysiology, frequency, and effects of different treatment modalities. Diabetes Care 2005;28:2948–2961PMID : 16306561.


22. Geddes J, Schopman JE, Zammitt NN, Frier BM. Prevalence of impaired awareness of hypoglycaemia in adults with type 1 diabetes. Diabet Med 2008;25:501–504PMID : 18387080.


23. Gerich JE, Langlois M, Noacco C, Karam JH, Forsham PH. Lack of glucagon response to hypoglycemia in diabetes: evidence for an intrinsic pancreatic alpha cell defect. Science 1973;182:171–173PMID : 4581053.


24. Dagogo-Jack S, Rattarasarn C, Cryer PE. Reversal of hypoglycemia unawareness, but not defective glucose counterregulation, in IDDM. Diabetes 1994;43:1426–1434PMID : 7958494.


25. Dagogo-Jack S, Fanelli CG, Cryer PE. Durable reversal of hypoglycemia unawareness in type 1 diabetes. Diabetes Care 1999;22:866–867PMID : 10332708.


26. Smith CB, Choudhary P, Pernet A, Hopkins D, Amiel SA. Hypoglycemia unawareness is associated with reduced adherence to therapeutic decisions in patients with type 1 diabetes: evidence from a clinical audit. Diabetes Care 2009;32:1196–1198PMID : 19389817.



27. Dagogo-Jack S. Hypoglycemia in type 1 diabetes mellitus: pathophysiology and prevention. Treat Endocrinol 2004;3:91–103PMID : 15743105.


28. Cryer PE. Diverse causes of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med 2004;350:2272–2279PMID : 15163777.


30. Cranston I, Lomas J, Maran A, Macdonald I, Amiel SA. Restoration of hypoglycaemia awareness in patients with long-duration insulin-dependent diabetes. Lancet 1994;344:283–287PMID : 7914259.


31. Fanelli C, Pampanelli S, Epifano L, et al. Long-term recovery from unawareness, deficient counterregulation and lack of cognitive dysfunction during hypoglycaemia, following institution of rational, intensive insulin therapy in IDDM. Diabetologia 1994;37:1265–1276PMID : 7895957.


32. Wendel CS, Fotieo GG, Shah JH, Felicetta J, Curtis BH, Murata GH. Incidence of non-severe hypoglycaemia and intensity of treatment among veterans with type 2 diabetes in the USA: a prospective observational study. Diabet Med 2014;31:1524–1531PMID : 24975871.


33. UK Hypoglycaemia Study Group. Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia 2007;50:1140–1147PMID : 17415551.



34. Donnelly LA, Morris AD, Frier BM, et al. Frequency and predictors of hypoglycaemia in type 1 and insulin-treated type 2 diabetes: a population-based study. Diabet Med 2005;22:749–755PMID : 15910627.


35. Pedersen-Bjergaard U, Pramming S, Heller SR, et al. Severe hypoglycaemia in 1076 adult patients with type 1 diabetes: influence of risk markers and selection. Diabetes Metab Res Rev 2004;20:479–486PMID : 15386817.


36. Bruderer SG, Bodmer M, Jick SS, Bader G, Schlienger RG, Meier CR. Incidence of and risk factors for severe hypoglycaemia in treated type 2 diabetes mellitus patients in the UK: a nested case-control analysis. Diabetes Obes Metab 2014;16:801–811PMID : 24612200.


37. Davis TM, Brown SG, Jacobs IG, Bulsara M, Bruce DG, Davis WA. Determinants of severe hypoglycemia complicating type 2 diabetes: the Fremantle diabetes study. J Clin Endocrinol Metab 2010;95:2240–2247PMID : 20305006.


38. Kong AP, Yang X, Luk A, et al. Hypoglycaemia, chronic kidney disease and death in type 2 diabetes: the Hong Kong diabetes registry. BMC Endocr Disord 2014;14:48. PMID : 24927961.




39. Murata GH, Duckworth WC, Shah JH, Wendel CS, Mohler MJ, Hoffman RM. Hypoglycemia in stable, insulin-treated veterans with type 2 diabetes: a prospective study of 1662 episodes. J Diabetes Complications 2005;19:10–17PMID : 15642485.


40. Yun JS, Ko SH, Ko SH, et al. Presence of macroalbuminuria predicts severe hypoglycemia in patients with type 2 diabetes: a 10-year follow-up study. Diabetes Care 2013;36:1283–1289PMID : 23248198.



41. Abraira C, Colwell JA, Nuttall FQ, et al. Veterans Affairs Cooperative Study on glycemic control and complications in type II diabetes (VA CSDM): results of the feasibility trial. Veterans Affairs Cooperative Study in Type II Diabetes. Diabetes Care 1995;18:1113–1123PMID : 7587846.


42. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853PMID : 9742976.


43. Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129–139PMID : 19092145.


44. Quilliam BJ, Simeone JC, Ozbay AB. Risk factors for hypoglycemia-related hospitalization in patients with type 2 diabetes: a nested case-control study. Clin Ther 2011;33:1781–1791PMID : 22018449.


45. Leese GP, Wang J, Broomhall J, et al. Frequency of severe hypoglycemia requiring emergency treatment in type 1 and type 2 diabetes: a population-based study of health service resource use. Diabetes Care 2003;26:1176–1176PMID : 12663593.


46. Cryer PE. Death during intensive glycemic therapy of diabetes: mechanisms and implications. Am J Med 2011;124:993–996PMID : 22017775.



47. Lung TW, Petrie D, Herman WH, et al. Severe hypoglycemia and mortality after cardiovascular events for type 1 diabetic patients in sweden. Diabetes Care 2014;37:2974–2981PMID : 25092684.


48. Zoungas S, Patel A, Chalmers J, et al. Severe hypoglycemia and risks of vascular events and death. N Engl J Med 2010;363:1410–1418PMID : 20925543.


49. Lindstrom T, Jorfeldt L, Tegler L, Arnqvist HJ. Hypoglycaemia and cardiac arrhythmias in patients with type 2 diabetes mellitus. Diabet Med 1992;9:536–541PMID : 1643801.


50. Beom JW, Kim JM, Chung EJ, et al. Corrected QT interval prolongation during severe hypoglycemia without hypokalemia in patients with type 2 diabetes. Diabetes Metab J 2013;37:190–195PMID : 23807922.



51. Chow E, Bernjak A, Williams S, et al. Risk of cardiac arrhythmias during hypoglycemia in patients with type 2 diabetes and cardiovascular risk. Diabetes 2014;63:1738–1747PMID : 24757202.


52. Gruden G, Giunti S, Barutta F, et al. QTc interval prolongation is independently associated with severe hypoglycemic attacks in type 1 diabetes from the EURODIAB IDDM complications study. Diabetes Care 2012;35:125–127PMID : 22124713.



53. Rossing P, Breum L, Major-Pedersen A, et al. Prolonged QTc interval predicts mortality in patients with type 1 diabetes mellitus. Diabet Med 2001;18:199–205PMID : 11318840.


54. Robinson RT, Harris ND, Ireland RH, Lee S, Newman C, Heller SR. Mechanisms of abnormal cardiac repolarization during insulin-induced hypoglycemia. Diabetes 2003;52:1469–1474PMID : 12765959.


55. Hay LC, Wilmshurst EG, Fulcher G. Unrecognized hypo- and hyperglycemia in well-controlled patients with type 2 diabetes mellitus: the results of continuous glucose monitoring. Diabetes Technol Ther 2003;5:19–26PMID : 12725703.


56. Banarer S, Cryer PE. Sleep-related hypoglycemia-associated autonomic failure in type 1 diabetes: reduced awakening from sleep during hypoglycemia. Diabetes 2003;52:1195–1203PMID : 12716752.


57. Stahn A, Pistrosch F, Ganz X, et al. Relationship between hypoglycemic episodes and ventricular arrhythmias in patients with type 2 diabetes and cardiovascular diseases: silent hypoglycemias and silent arrhythmias. Diabetes Care 2014;37:516–520PMID : 24041680.


58. Wright RJ, Frier BM. Vascular disease and diabetes: is hypoglycaemia an aggravating factor? Diabetes Metab Res Rev 2008;24:353–363PMID : 18461635.


59. Clark AL, Best CJ, Fisher SJ. Even silent hypoglycemia induces cardiac arrhythmias. Diabetes 2014;63:1457–1459PMID : 24757198.



60. Zhang Z, Lovato J, Battapady H, et al. Effect of hypoglycemia on brain structure in people with type 2 diabetes: epidemiological analysis of the ACCORD-MIND MRI trial. Diabetes Care 2014;37:3279–3285PMID : 25267796.



61. Blasetti A, Chiuri RM, Tocco AM, et al. The effect of recurrent severe hypoglycemia on cognitive performance in children with type 1 diabetes: a meta-analysis. J Child Neurol 2011;26:1383–1391PMID : 21572053.


62. Feinkohl I, Aung PP, Keller M, et al. Severe hypoglycemia and cognitive decline in older people with type 2 diabetes: the edinburgh type 2 diabetes study. Diabetes Care 2014;37:507–515PMID : 24103900.


63. Lopez JM, Annunziata K, Bailey RA, Rupnow MF, Morisky DE. Impact of hypoglycemia on patients with type 2 diabetes mellitus and their quality of life, work productivity, and medication adherence. Patient Prefer Adherence 2014;8:683–692PMID : 24855344.



64. Allen KV, Frier BM. Nocturnal hypoglycemia: clinical manifestations and therapeutic strategies toward prevention. Endocr Pract 2003;9:530–543PMID : 14715482.


65. Brod M, Christensen T, Thomsen TL, Bushnell DM. The impact of non-severe hypoglycemic events on work productivity and diabetes management. Value Health 2011;14:665–671PMID : 21839404.


66. Kong AP, Yang X, Luk A, et al. Severe hypoglycemia identifies vulnerable patients with type 2 diabetes at risk for premature death and all-site cancer: the Hong Kong diabetes registry. Diabetes Care 2014;37:1024–1031PMID : 24513587.


67. Araki A, Ito H. Diabetes mellitus and geriatric syndromes. Geriatr Gerontol Int 2009;9:105–114PMID : 19740352.


68. Munshi M, Grande L, Hayes M, et al. Cognitive dysfunction is associated with poor diabetes control in older adults. Diabetes Care 2006;29:1794–1799PMID : 16873782.



69. Moen MF, Zhan M, Hsu VD, et al. Frequency of hypoglycemia and its significance in chronic kidney disease. Clin J Am Soc Nephrol 2009;4:1121–1127PMID : 19423569.



70. Ko SH, Kim SR, Kim DJ, et al. 2011 clinical practice guidelines for type 2 diabetes in Korea. Diabetes Metab J 2011;35:431–436PMID : 22111032.



71. Hermanns N, Kulzer B, Kubiak T, Krichbaum M, Haak T. The effect of an education programme (HyPOS) to treat hypoglycaemia problems in patients with type 1 diabetes. Diabetes Metab Res Rev 2007;23:528–538PMID : 17245692.


72. Yong YM, Shin KM, Lee KM, et al. Intensive individualized reinforcement education os important for the prevention of hypoglycemia in patients with type 2 diabetes. Diabetes Metab J 2015;Forthcoming.



73. Yoo HJ, Park KY, Park KS, et al. Safety and efficacy of modern insulin analogues. Diabetes Metab J 2013;37:181–189PMID : 23807921.



74. Monami M, Marchionni N, Mannucci E. Long-acting insulin analogues versus NPH human insulin in type 2 diabetes: a meta-analysis. Diabetes Res Clin Pract 2008;81:184–189PMID : 18495286.


75. Kulzer B, Seitz L, Kern W. Real-world patient-reported rates of non-severe hypoglycaemic events in Germany. Exp Clin Endocrinol Diabetes 2014;122:167–172PMID : 24643694.


76. Lin CH, Sheu WH. Hypoglycaemic episodes and risk of dementia in diabetes mellitus: 7-year follow-up study. J Intern Med 2013;273:102–110PMID : 23003116.


Figure 2
Glycemic threshold for counter-regulatory hormones and the onset of changes in hypoglycemic symptoms in response to hypoglycemia in non-diabetic subjects.
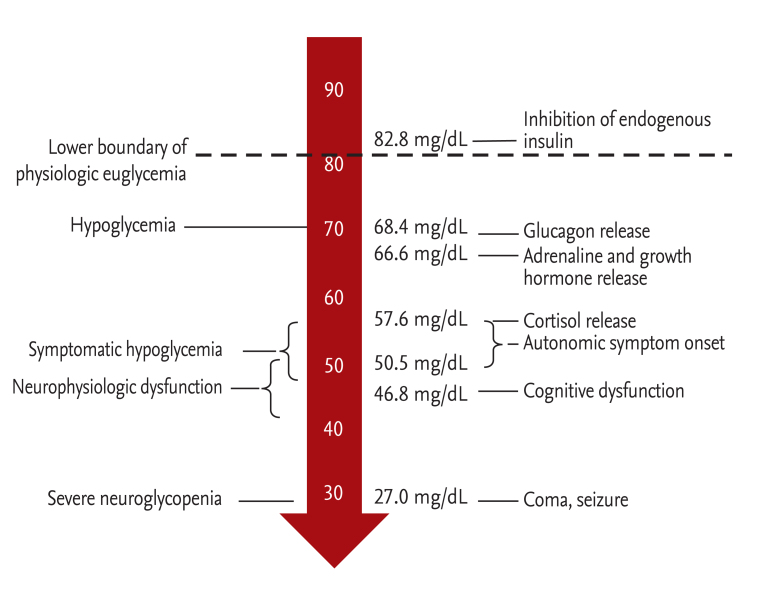
Table 2
Incidence of severe hypoglycemia in trials of intensive versus conventional glycemic control
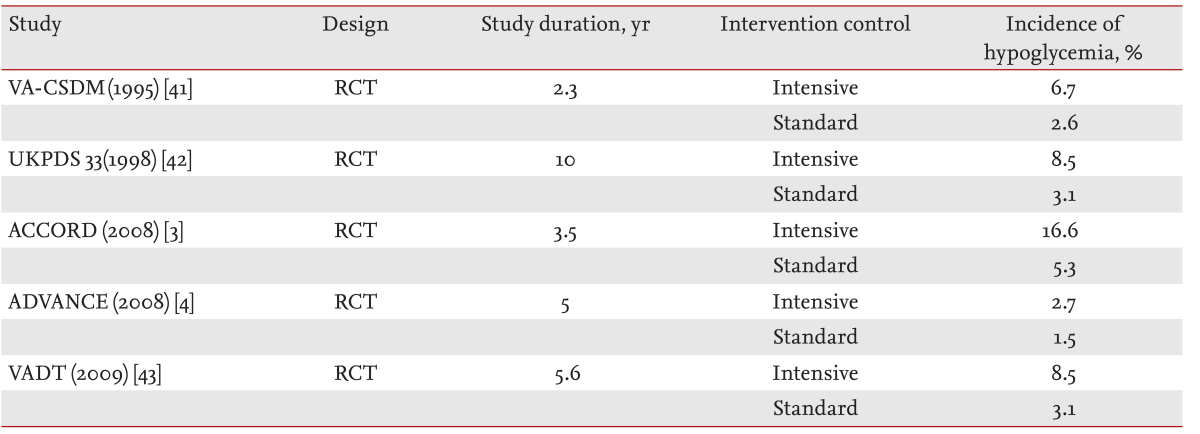
VA-CSDM, Veterans Affairs Cooperative Study on glycemic control and complications in type II diabetes; RCT, randomized controlled trial; UKPDS, UK Prospective Diabetes Study; ACCORD, Action to Control Cardiovascular Risk in Diabetes; ADVANCE, Action in Diabetes and Vascular Disease; VADT, Veterans Affairs Diabetes Trial.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



