Prognostic Evaluation of Endoscopic Sclerotherapy on Bleeding Esophageal Varices
Article information
Abstract
From November 1981 to March 1984, 100 patients with esophageal varices bleeding were treated by endoscopic sclerotherapy.
The combined peri and intravasal method was applied, using Äthoxysclerol as a sclerosant.
The 79 cases were followed after sclerotherapy over a period ranging from 3 months to 26 months.
The amount of transfused blood on presclerotherapy was 4–5 pints and in 2/3 cases 1–2 pints were needed on postsclerotherapy.
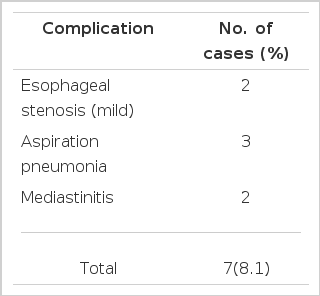
Seven cases (8.1 per cent) had complications; 2 cases developed esophageal stenosis, 3 cases aspiration pneumonia, and 2 cases mediastinitis.
Fortunately, all 7 cases recovered. Rebleeding occurred in 15 cases (19.0 per cent); namely 3 cases (3.8 per cent) within 6 months, 5 cases (6.3 per cent) in the period from 6 months to 12 months and 7 cases (8.9 per cent) after 12 months.
During the follow up period, 14 cases died. Their causes of death were as follows: 6 cases died of hepatic failure, 5 cases died of hepatoma, and 3 cases expired from uncontrollable bleeding.
Based on data, it appears to be possible to control the bleeding in 97 per cent of the esophageal varices bleeding on their (first) bleeding.
INTRODUCTION
Hemorrhage from esophageal varices, which is caused by severe bleeding itself as well as further hepatic dysfunction due to decrease in circulating blood volume, has represented the highest mortality among all the upper gastrointestinal bleedings.
Up to now, the most effective therapy of hemorrhage from esophageal varices has not been found, so that hemorrhagic patients were managed by emergent portosystemic shunt operations or various non-shunt operations. The operative mortality, however, has exceeded 50 percent.1–3) Although these operations were performed on selected patients, they failed to reduce the complication such as postoperative encephalopathy in many cases. Thus, Warren’s shunt operation was applied to a small number of selected patients in order to reduce postoperative complications, but the effect was limited.4–8)
The mortality of conservative treatment, using Sengstaken Blakemore or Linton Nachlas Tube, was as high as 20 to 60 percent. In addition, the ratio of rebleeding when removing the balloon tube reached from 20 to 80 percent.9–12)
Like the preceding results, infusion of vasopressin had a temporary hemostatic effect, so that we need a new method combined with other methods for management of esophageal bleeding.
More recently, variceal hemorrhage has been treated by endoscopic sclerotherapy and transhepatic sclerosis for better control of bleeding.5,13–16) However, between two methods, transhepatic sclerosis was not practiced by a great number of medical centers because of its technical difficulty and its frequent side effects. In conclusion, we have considered endoscopic sclerotherapy as the most effective method for the treatment of bleeding from esophageal varices.17–20)
METHODS
From November 1981 to March 1984, we controlled 100 patients with bleeding from esophageal varices, who were treated by endoscopic sclerosis. In addition, we selected 79 patients among 90 patients who received the first sclerotherapy until December 1983, for the purpose of evaluating the incidence of rebleeding after sclerosis, because they (79 patients) were followed up over a period ranging from 3 months to 26 months after the first successful sclerotherapy.
We applied the combined peri and intravasal method, whose procedure was as follows:
The endoscope was passed to the distal esophagus and the first injection was applied 5 cm above the cardio-esophageal junction and the second injection was applied at 1cm above the junction. In case of a large solitary esophageal varix, the modified method of sclerotherapy was applied.5,16,21–23)
Sclerosant used was 1 percent of polidocanol (hydroxy polyathoxydedocan: Krussler Co, GmBH) which could cause edema of vascular intimal layer within a few minutes as well as necrosis or fibrosis of vessels.
The amount of injected sclerosant per injection was 25 ml to 70 ml. In case of a large solitary varix, 25 ml was enough, although in case of severe multiple esophageal varices, an average of 60 ml was needed.
The endoscope for sclerotherapy, Olympus D4 was used because it could magnify edema effect as well as hemostatic effect against bleeding. During the follow up periods, we used Olympus P3. For infusion of sclerosant, we made cannula by our own efforts but the selling of cannula is now under way.
RESULTS
From November 1981 to March 1984, 100 patients (79 males and 21 females) with bleeding esophageal varices were treated with endoscopic sclerotherapy which was carried out 142 times in all. The male to female ratio was 3.8:1 and 80 patients (80 percent) were between the ages of 40 and 50 (Table 1).
Table 2 shows the distribution of Child’s Scale.45) As we can see, 11 cases belonged to Scale A, 30 cases Scale B and 59 cases Scale C. We concluded that patients were suffering from advanced hepatic dysfunction in the majority of cases who underwent sclerotherapy.
The etiology of bleeding from esophageal varices was, most frequently, postnecrotic cirrhosis in 58 cases (58 percent), alcoholic liver cirrhosis in 7 cases (7 percent), portal hypertension of unknown origin in 4 cases (4 percent), and unidentified in 31 cases (31 percent), a few of them with hepatoma (Table 3).
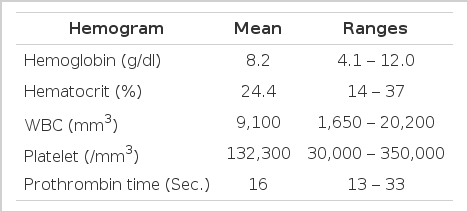
In the West, the number of patients with bleeding due to alcoholic cirrhosis (60 to 80 per cent), has been contrastly higher than that of the East. On admission all patients were severely anemic; the average level of hemoglobin was reduced to 8.2 gm and the prothrombin time was markedly prolonged to a 16 sec. in average (Table 4).
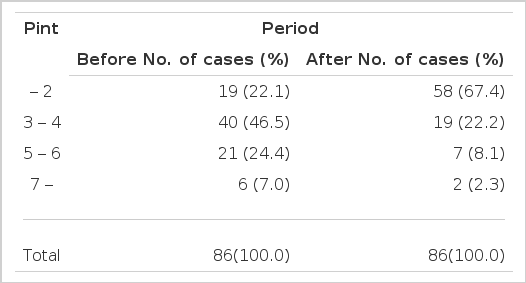
From the time of admission to that of discharge, we observed the amount of blood transfusion before and after endoscopic sclerotherapy. According to Table 5, the average amount of transfused blood prior to performing sclerotherapy was four to five pints, but in two-thirds of the cases, one or two pints was sufficient after sclerotherapy.
The side effects after sclerotherapy such as mild febrile sensation, chest pain, abdominal pain or ascites, were mild in general, and were considered physiological responses as the general condition was poor. Except these physiological responses, we could observe complications of the sclerotherapy in 7 cases (8.1 per cent) among 86 survivals. The complications included 2 cases of esophageal stenosis, 3 cases of aspiration pneumonia, and 2 cases of mediastinitis (Table 6). In several days complications subsided and esophageal stenosis was not a hindrance in eating habits.
The most important concern after successful sclerotherapy was rebleeding during a fixed period. Hence, we observed the incidence of rebleeding after 3 months from the first sclerotherapy. For there was a risk of rebleeding due to residual varices among bleeding patients. So, it was necessary among those patients to perform sclerotherapy again.
In these conditions, among 79 survivals after the first sclerotherapy, the recurrence of bleeding varices was noted in 15 cases (19.0 per cent). Among those 15 cases, 3 cases (3.8 per cent) were within 6 months, 5 cases (6.3 per cent) were from 6 months to 12 months, and 7 cases (8.9 per cent) were after 12 months (Table 7).
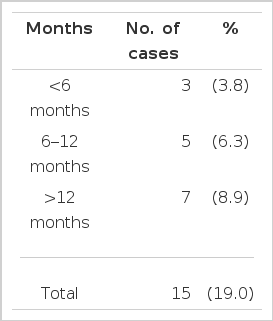
Incidence of rebleeding after 3 months from successful sclerotherapy (79 survivals from Nov.’81 to Dec.’83)
Fourteen of 100 patients died after endoscopic sclerotherapy and their causes of death were as follows: 6 cases of hepatic failure, 5 cases of hepatoma, and 3 cases of uncontrolled bleeding which was caused by the failure of hemostasis or the persistent bleeding from severe multiple esophageal varices (Table 8).
DISCUSSION
In 1939, Crafoord and Franckner were the first two men which succeeded in obliterating hemorrhage from esophageal varices by sclerotherapy.24 Their first patient for sclerotherapy was a 16 years old girl. They used a stiff endoscope and quinine as sclerosant. Since then, the most remarkable research for sclerotherapy was achieved by Denck,25,26) Paquet27,28) and Soehendra.5,16,21,29,30)
The development in endoscopic sclerotherapy was in parallel with that of sclerosant simultaneously. Consequently, sclerotherapy could be performed, using not stiff endoscope but flexible endoscope, which was a great achievement.29)
The selection of sclerosant was necessary to perform successful sclerotherapy. Recently, many types of sclerosant have already been in production from so many countries. The frequently used ones as sclerosants are sodium morrhuate, ethanolamine oleate, polidocanol, sodium tetradecyl sulphate and phenol oil.25,30–39) Sclerosant requires a few conditions to be used in endoscopic sclerotherapy. Sclerosant should be excellent in hemostatic effect and sclerotic effect. In addition, sclerosant should cause minimal inflammatory changes in tissue and minimal systemic side effects within the limit of possibility. Lastly, aqueous is more useful than mucous solution. In these respects, polidocanol can be acceptable as sclerosant, even though not perfect.21,27–30,40,41)
For patients assigned to endoscopic sclerotherapy, the matter of procedure should be considered after selection of sclerosant. In fact, the technical methods could be divided into some ways, according to the types of sclerosant, the morphology of esophageal varices, and to the degree of esophageal varices. Now, we can classify the methods of sclerotherapy into three methods, namely, paravasal method, intravasal method and combined peri and intravasal method.21,23,29,36,42,43)
The paravasal method, is by injection of small amounts of sclerosant into nonvariceal esophageal mucosa. But when we performed this method, we should repeat the trial of sclerotherapy regularly, every 6 months and once this method was applied, bleeding was frequent by the change of necrosis in esophageal mucosa.29)
The intravasal method is by the injection of sclerosant into the intravariceal directly. However, this procedure requires special devices such as a tube to prevent bleeding from spreading around the part where sclerosant was injected.42–44)
The combined peri and intravasal method is by the injection of sclerosant into perivascular in advance in order to prevent the risk of bleeding during the trial of this method and then is by the direct injection of the sclerosant into the intravasal of varices.21,23,24,40) Generally, in this method, the sclerosant used was 50 to 60 ml of 1 per cent polidocanol at a time.16,21,23,40)
Regardless of the East or the West, it was a well known fact that bleeding from esophageal varices has been frequent in males, especially in his thirties or forties. The most frequent etiology of bleeding varices (about 90 per cent) was portal hypertension due to liver cirrhosis. In Korea, postnecrotic liver cirrhosis after viral B hepatitis has commanded the majority of causes of bleeding from esophageal varices.40) However, in the West, alcoholic liver cirrhosis (60 to 80 per cent) was the major cause of esophageal varices.21,41) At the time of admission, we examined hepatic reserve of all of the patients. According to the results of examination, patients belonged to Child’s Scale11,45) B in 30 per cent and scale C in 59 per cent, which showed that 89 per cent of all of the patients had severe hepatic dysfunction, so that surgical therapy was impossible to those patients. Theoretically, it is exceedingly difficult to compare the prognosis of patients after sclerotherapy with the patients after shunt operations. During the initial hospitalization, hematological findings explained that fact very well. Especially, the prothrombin time was markedly prolonged to an average 16 sec. (control 13 sec). More recently, the injection of blood coagulation factors was tried with an attempt to avoid the prolonged prothrombin time. However the duration of effect was too short and it could be obtained only by the imports from abroad.
At the time of bleeding from esophageal varices, massive bleeding was expected, so we had to prepare considerable amount of blood. Especially, fresh whole blood was very helpful because they could supply blood coagulation factors to some degree.5,12,15,16,23,40)
For patients assigned to endoscopic sclerotherapy, the average amount of transfused blood prior to perform sclerotherapy was 5 pints, but in most cases (67.4 per cent), one or two pints were enough after sclerotherapy, which suggested that sclerotherapy could minimize the complication due to blood transfusion.
The complications of sclerotherapy were mild in general, as in mild febrile sensation, chest pain, and abdominal pain, which could be vanished in a few hours or recovered naturally. We also could find a severe complication such as esophageal stricture, which could be shown in case of performing sclerotherapy twice or more because of frequent recurrent bleeding. Even though in this case, patients could live without any difficulty in eating habits. Sometimes we could find aspiration pneumonia or mild mediastinitis as complications, which would be recovered in a few days by medical treatment.21,40,41)
The main concern after sclerotherapy has been rebleeding in prognostic evaluation of endoscopic sclerotherapy.
Up to present, researches about the frequency of rebleeding after sclerotherapy were insufficient. For the history of sclerotherapy is still not long enough and the aspects of rebleeding can be altered by the abilities of performers.
From 3 months on after the first sclerotherapy, we set up a scope of observing the frequency of rebleeding, not only because it needed 2 or 3 months to recover esophageal mucosa to a normal state, if necessary, but we tried prophylactic sclerotherapy on residual varices. Sclerotherapy could not reduce the incidence of rebleeding perfectly among the patients who survived, and the risk of rebleeding was 19.0 per cent. Among those 15 cases, 8 cases were within 12 months and 7 cases were after 12 months. In conclusion, in order to prevent rebleeding for the patients with severe esophageal varices, the regular examination and prophylactic sclerotherapy are necessary from the sixth month after the first sclerotherapy.21,40,41)
During hospitalization or follow-up periods, 14 patients (14 per cent) died and their causes of death were hepatic failure with or without hepatoma in 11 cases (11 per cent) and persistent bleeding in 3 cases (3 per cent).
Consequently, the possibility of hemostasis by endoscopic sclerotherapy was 97 per cent among the trials at In-Je Medical College Hospital.