Influence of Helicobacter pylori Colonization on Histological Grading of Chronic Gastritis in Korean Patients with Peptic Ulcer
Article information
Abstract
Objectives:
We conducted an analysis of correlation between histological grading of chronic gastritis and the presence of H. pylori infection to investigate if H. pylori influences histological severity of chronic gastritis in Korean patients with peptic ulcers.
Methods:
Gastroscopic antral biopsy specimens and peripheral venous blood were taken from 80 patients with gastric or duodenal ulcers. H. pylori was identified microscopically in sections with Giemsa staining and quantitative grading of cultured H. pylori was reported on a scale 0 to 3. The histopathological features of biopsy specimens were reported according to the Sydney classification of chronic gastritis. Serum gastritis and pepsinogen concentrations were measured by radioimmunoassay.
Results:
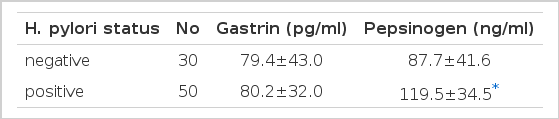
H. pylori was identified in 62.5% (20 of 32 GU, 30 of 48 DU) of the study group. Gastric clonization rate of H. pylori did not increased with age. Forty of 50 biopsy specimens with H. pylori and also 23 of 30 biopsy specimens without H. pylori showed active chronic gastritis. There was no significant correlation overall between the presence of H. pylori and histological grading of chronic gastritis, including activity, and also no association was found between the quantitative grading of H. pylori and the histological grading of chronic gastritis. With and without H. pylori, a mean of serum gastritis concentration (79.4±43.0 pg/ml and 80.2±31.9 pg/ml) showed no significant difference, but a mean of serum pepsinogen concentration (87.7±41.6 ng/ml and 119±34.4 ng/ml) showed significant difference between the populations with and without H. pylori (p=0.001)
Conclusions:
The influence of H. pylori on histological grading of chronic gastritis in Korean is less than that in prior studies of Western countries, and further investigation of pathogenesis of H. pylori in chronic gastritis and peptic ulceration is necessary.
INTRODUCTION
Following the discovery and isolation of the organism by Marshall and Warren1), the evidence that Helicobacter pylori (H. pylori) causes non-erosive gastritis comes from studies in which eradication has been achieved with antibiotics. In these studies there is usually a marked lessening in the severity of the gastritis2–4). Probably more than 80% of cases of chronic gastritis are associated with coexisting H. pylori infection, and both the H. pylori and the gastritis are strongly linked with peptic ulcer5). Gastric colonization with H. pylori has been reported in 90 percent of patients with duodenal ulcer (DU) and in 60% of patients with gastric ulcer (GU)6).
Koch’s postulates concerning the causal relationship between H. pylori and chronic gastritis seem to be satisfactorily fulfilled7) but the cause of chronic gastritis is various. In general, prevalence of H. pylori in Western countries is low and increases with age but in underdeveloped countries, it is not decidedly checked and most adults may be infected8). Since this is so, there is a possibility that the role of H. pylori in the pathogenesis of chronic gastritis may be different between Western and developing countries, in which the prevalence rate of chronic gastritis is high. Thus, it is still a matter of controversy that H. pylori is really an significant cause in chronic gastritis and associated with the severity of chronic gastritis in developing countries.
The aim of our study was to investigate if H. pylori influences the histological severity of chronic gastritis in Korean peptic ulcer patients. We conducted an analysis of correlation between histological grading of chronic gastritis and the presence of H. pylori infection.
MATERIAL AND METHODS
We studied 80 patients, attending a gastrointestinal clinic of Chung-Ang University Hospital, for investigation of epigastric soreness, hunger pain or dyspepsia with duodenal or benign gastric ulcer as identified from routine gastrofiberscopic examination. The patients who had been taking anti-ulcer treatment in the month before the gastroscopy were excluded from the study. Peptic ulcer staging was reported, according to the Japanese classification of gastrointestinal endoscopy, by two endoscopists.
Peripheral venous blood and gastroscopic antral biopsy specimens were taken from 80 patients. Blood was collected after gastroscopy and kept at 5°C. Serum was separated within two hours and frozen at −20°C until analysis. During endoscopy, four antral biopsy specimens were obtained from the lesser gastric curvature, 2 cm proximal to the pylorus. Two biopsy specimens were used for histological examination(H & E staining, Giemas staining) and two biopsy specimens were taken for the culture of H. pylori. Serum gastritis concentration was measured by the radioimmunoassay technique, using the GammaDab-I125 Gastritis RIA kit(INCSTAR Co., UK) and serum pepsinogen concentration was measured by pepsinogen radioimmunoassay kit, Pepsik (Sorin Biomedical, France). Each examination was duplicated.
1. Assessment of H. pylori
Antral biopsy specimens for histological examination were fixed in formalin and routinely processed, and specimens for culture were embedded in sterile saline and processed by the methods in our previous report9). H. pylori was identified microscopically in sections with Giemsa staining and by culture in blood agar medium. After routine culture, quantitative grading of cultured H. pylori was reported on a scale 0 to 3 (none, few, some, many).
2. Histological Assessment of Gastritis
For histological grading of chronic gastritis, sections were stained with hematoxylin and eosin. The histopathological features of biopsy specimens were reported according to the Sydney classification10) of chronic gastritis (inflammation, activity, atrophy and metaplasia were each graded on a scale 0 to 3) by one histopathologist without knowledge of the clinical and endoscopic findings.
3. Statistical Analysis
Data were expressed in means and standard deviations. X2 test was used to determine the significance of differences between means. A value of p<0.05 was considered to be statistically significant. The Spearman rank correlation test was used to determine whether there was a relationship between increasing grade of gastritis and increasing H. pylori concentration, and we used ANOVA in analysis of multiple groups. All analysis were done with SPSS/PC+.
RESULT
A total 80 patients were evaluated in the study. Fifty nine patients were male and 21 were female with a mean age of 44.3±13.1 years (range 18–81). Thirty two (40%) had gastric ulcer (30 active or healing stage, 2 scar stage) and 48 (60%) had duodenal ulcer (42 active or healing stage, 6 scar stage) among 80 patients endoscoped. H. pylori was identified in 62.5% (20 of 32 GU, 30 of 48 DU) of the study group. Percentages of gastritis colonization of H. pylori were the same in GU and DU.
There was no significant difference between with and without gastric colonization of H. pylori, with respect to age, sex and underlying type of peptic ulcer (Table 1). Gastric colonization rate of H. pylori among patients did not increase with age (Fig. 1).
None of the biopsy specimens showed inflammation grade 0 and so all were chronic gastritis. Seventeen of 80 patients had chronic gastritis without any sign of activity. Forty of 50 biopsy specimens with H. pylori showed active chronic gastritis, whereas 23 of 30 biopsy specimens without H. pylori showed active chronic gastritis. Association of activity of chronic inflammation with H. pylori concentration was not statistically significant (Fig. 2). There was no significant correlation overall between the presence of H. pylori and histological grading of chronic gastritis (p>0.1), and also no association was found between the quantitative grading of H. pylori and the histological grading of chronic gastritis (p>0.1) (Table 2).
Increased H. pylori concentration is not associated with increased activity of chronic inflammation.

Overall Correlation between Histological Grading of Chronic Gastritis and Gastric Colonization of H. pylori
With and without H. pylori, a mean of serum gastritis concentration was 79.4±43.0 pg/ml and 80.2±31.9 pg/ml respectively, and there was no significant difference with respect to the presence of H. pylori. A mean of serum pepsinogen concentration was 87.7±41.6 ng/ml and 119.5±34.4 ng/ml with and without H. pylori, and the statistical analysis, excluding the influence of peptic ulcer, showed significant difference of serum pepsinogen concentrations between the populations with and without H. pylori (p = 0.001) (Table 3).
DISCUSSION
The most obvious disease associated with H. pylori is peptic ulcer. The report that more than 90% of duodenal ulcers and about 70% of gastric ulcers were caused by H. pylori is accepted in Western countries8). But in Korea, the infection rates of H. pylori in GU and DU were 62%–81%11–13) and 62%–83%9,11–13), respectively, and our study showed 62.5% infection rate of H. pylori, similar to other results of the Korean prevalence study of H. pylori. The role of H. pylori on peptic ulcer is assuredly less in Korea than in Western countries.
In Western countries, H. pylori is uncommon in young children and affects about 20% of persons below the age of 40 yr and 50% of those above the age of 60 yr. Low socio-economic status predicts H. pylori infection8). But in most developing countries like Korea, an endemic of H. pylori goes unchecked, and most adults are infected. In the present study, gastric colonization rate of H. pylori did not increase with age, as suggested in one report dealing with infection rate of H. pylori in Korean children14). The epidemiology reported by Megraud15) that, in countries such as Asia, Africa and Easten Europe, most are infected by their teens may be applicable to Korean cases.
Delineating the normal cellular content of the lamina propria of the gastric mucosa is difficult and disagreement between pathologists on what is an acceptable normal background is the basis of many discrepant reports in the literatures. An even distribution of very small numbers of lymphocytes and plasma cells is acceptable10). In our study, all biopsy specimens showed an increase in lymphocytes and plasma cells within the lamina propria, but 17 of 80 specimens did not show the increased neutrophil polymorphs in the lamina propria, gastric pits and surface epithelium. Endoscopically, many adults in Korea showed chronic gastritis, but the exact prevalence of endoscopic and histological chronic gastritis of Koreans is not available.
There is marked variation between the intensity of inflammation and the number of organisms in a histologic section. When there is intense epithelial change with marked mucus depletion, organisms may be sparse and more easily seen in adjacent areas, where there are more normal mucous cells16). Activity of chronic gastritis is known as a useful measure of response to therapy and can be particularly related to the presence and concentration of H. pylori2,8,17–19). But, in the present study, H. pylori concentation did not affect the activity of chronic gastritis and overall histological grading of chronic gastritis, and atrophy of chronic gastritis did not affect the presence of H. pylori. There is one possibility that a small number of patients in our study may affect the statistical result, and another possibility that the role of H. pylori on the pathogenesis of chronic gastritis in endemic countries of H. pylori may differ from that in Western countries. Further studies for host reaction to H. pylori and for a causal sequence of H. pylori and chronic gastritis are necessary.
H. pylori causes gastritis and a number of perturbation of gastric and duodenal function. H. pylori-related changes of gastric function are hypergastrinemia, hyperpepsinogenemia and on increase in acid secretion. H. pylori gastritis is associated with a decrease in the number of antral D cells and G cells, although the proportion of G cells to D cells appears to be unchanged, and the exaggerated gastritis release associated with the H. pylori infection appears to be secondary to the production of cytokines20). We reported that eradication of the organism resulted in a significant fall in serum gastritis concentration21) but, in the present study, H. pylori infection did not affect serum gastritis concentration. Because there was a possibility that this outcome may result from the effect of underlying peptic ulcers, we have a plan to study the role of H. pylori on chronic gastritis without peptic ulcer. Asaka M, et al22) reported that pepsinogen I and II levels was increased in association with H. pylori infection and our study showed the same result. But the mechanisms of H. pylori-related hyperpepsinogenemia is uncertain.
On the basis of our observations, we conclude that the influence of H. pylori on the histological grading of chronic gastritis in Korea is less than that in prior studies of Western countries, and further investigation of the pathogenesis of H. pylori in chronic gastritis and peptic ulceration is necessary.
Notes
This research was supported by the Chung-Ang University research grants in 1993