Clinical Experience in 200 Renal Transplants at Catholic Medical Center
Article information
Abstract
Between March, 1969, and April, 1986, two hundred of renal allograft recipients were treated with either cyclosporine (CsA) + prednisone (n=53) or azathioprine (Aza) + prednisone (n = 147). On October 31, 1986, the actuarial patient survival rate at two years was 75% for all patient group. The corresponding graft survival rate at two years was 68 % for all patients. The actuarial patient survival rate at two years was 71% in the Aza group, and 94% in the CsA group including recipients converted from CsA to Aza (3 cases), which was statistically significant (p<.001), and the corresponding graft survival rate was 65% and 80%: the difference was not statistically significant. In the CsA-treated group, excluding converter from CsA to Aza (3 cases), however, the graft survival rate at two years was 91%, which was statistically significant (p = .0056). There was no significant difference of graft survival rate between the recipients who received DST vs non-DST in CsA-treated group. It was difficult to evaluate the recipients who were given DST due to a small number of cases and short follow-up period. In either, the Aza-or the CsA-treated group, the graft survival rates were higher in HLA identical LRD group than in either haplo-identical or mismatched LRD group. Total of 63 patients, who received kidney transplantation expired. The most frequent cause of death in 17.5% of cases was uremia per se due to graft failure, followed by infection (14.7%), vascular (14.3%), and cardiac (11.1%). The most commonly encountered posttransplant complications in order of frequency were as follows: erythrocytosis (18.0%), pneumonia (15.0%), urinary tract infections (14.0%), herpetic infections (12.0%), fungal infection (11.5%), posttransplant diabetes (8.5%), technical (5.0%) and others.
INTRODUCTION
The first successful kidney transplant was performed between identical twins at the peter Bent Brigham Hospital on December 23, 19541). During the last 3 decades, developments in surgical technique and increased expertise in immune modulation-by the first use of azathioprine (Aza) by Calne and Zukoski (1961): prednisone (PDN) by Goodwin et al. (1961): ALG by Monaco et al. (1965): HLA system by Van Rood et al. (1974): the benefits of transfusion by Terasaki et al. (1972): and cyclosporine (CsA) by Calne (1978)-provided marked improvement in the treatment of end stage renal disease2–5). The kidney transplantation in South Korea was first successfully performed in March, 1969, at the Catholic Medical Center (CMC), and since then, a total of approximately 700 transplants have been completed in South Korea6–9). The renal transplant team at CMC has been using cyclosporine (CsA) in allograft recipients since early 1984. The authors report the results of the 200 consecutive renal transplants performed using Aza + PDN therapy between March 25, 1969, and March 31, 1984 and CsA + PDN therapy between April, 1984, and April, 1986.
1. Patient Population and Selection
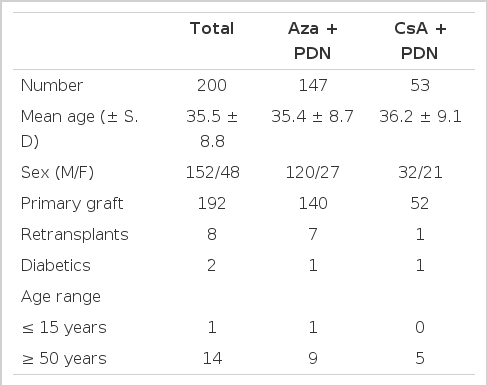
The study group represents two hundred patients who received transplants between March, 1969, and April, 1986, at CMC. Two hundred patients consisting of 152 men and 48 women with age range of 15 and 59 (mean 35.5 + 8.8) [2 with and 198 without diabetes; 168 recipients of living related donor graft, 23 recipients of non-related donor (NRD) graft and 9 recipients of cadaver donor (CAD); 192 recipients of primary and 8 recipients of secondary grafts] were divided into two treatment groups; 147 into an Aza group between March, 1969, and April, 1984, and 53 into a CsA group. All patients were followed for at least six months (Table 1). Of the 200 cases, 123 recipient donor pairs (107 LRD, 16 NRD) were typed for HLA-A,B,C, and DR antigens since July, 1979. Mixed lymphocyte cultures were done on 131 recipient-donor pairs.
2. Underlying Renal Diseases
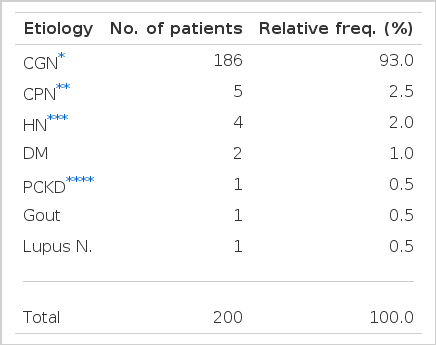
The most frequent disease among the transplant recipients was chronic glomerulonephritis with 186 cases (93.0%), followed by chronic pyelonephritis with 5 cases (2.5%), and hypertensive nephrosclerosis with 4 cases (2.0%) and others (Table 2).
3. Sex Distribution in Recipients and Donors
While the most of the recipients were males with 152 cases as opposed to only 48 females, most of the donors were females with 111 cases and 89 males (Table 3).
4. Age Distribution in Recipients and Donors
The fourth decade age group had the highest number of recipients with 85 cases, and the age group 20 through 49 represented 91% of a total (182 cases). The youngest recipient was 15 years of age, while the oldest was 59 years old. The age of the donors was relatively evenly distributed in 20 to 69 range. The youngest donor was 18, while the oldest was 78 years of age (Table 4).
5. Donor Sources
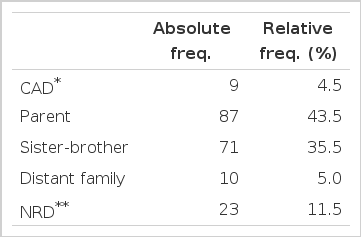
Of the 200 cases, 168 (84.0%) cases were from LRD, 23 cases (11.5%) from NRD, and 9 cases (4.5%) from CAD. Parents were the most frequent donors with 87 cases (43.5%), followed by siblings with 71 cases (35.5%). The NRD grafts were performed on one’s spouse or on individuals that volunteered (Table 5).
6. Aza Treatment
The Aza dose was 5 mg/kg preoperatively, tapered to 2 mg/kg after one week and, thereafter, adjusted according to the white blood cell count. The methylprednisolone dose was 200 mg intravenously administered on the operative day, 100 mg on the first postoperative day, and, thereafter, PDN was tapered to 0.2 to 0.3 mg/kg per day by one year.
7. CsA Treatment
CsA was taken orally in a dose 14 mg/kg prior to transplantation and daily during the first posttransplant week. The dose was then reduced to less than 12 mg/kg per day and adjusted according to serum creatinine level and according to CsA serum levels determined by radioimmunoassay technique (Sandoz. LTD Kit). The authors attempted to maintain serum creatinine concentrations less than 2 mg/dl and CsA levels between 50 and 150 ng/ml. The maintenance dose of CsA was 4 to 5 mg/kg at one and two years posttransplant. The methylprednisolone dose was 200 mg administered intravenously on the operative day, 100 mg on a first postoperative day, and was tapered to 0.2 to 0.3 mg/kg per day.
8. Analysis of Results
Patients and graft survival rates were calculated by actuarial techniques according to the groups in which the recipients were non-randomized. P values comparing the survival rate curves over the entire period of analysis were calculated using a generalized wilcoxon test. A graft loss was defined as either return to dialysis treatment or death with functioning graft. All causes of graft loss were included in the analysis, as were all deaths, including those that occurred years after graft loss and return to dialysis. Standard deviations are given with means.
RESULTS
1. Overall Patient and Graft Survival Rates
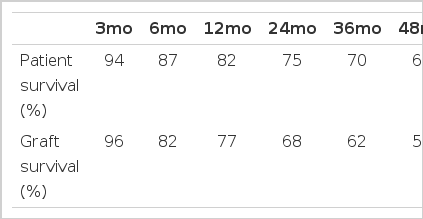
The actuarial patient survival rates at one and two years were 82% and 75% in the entire study group. The corresponding graft survival rates at one and two years were 77 % and 68 % in the patient population (Table 6, Fig. 1).
2. Results According to Immunosuppressive Regimens
The actuarial patient survival rates at one and two years were 78% and 71% respectively in the entire Aza-treated group, and 94% and 94% in the entire CsA treated group. The differences between the two groups were statistically significant at one and two year periods (p<.01, p<.001, respectively). The corresponding graft survival rates at on and two years were 74% and 65% in the entire Aza-treated group, and 87% and 80% respectively in the entire CsA-treated group which included the recipients converted from CsA to Aza (3 cases) for various reasons. The differences between the two groups were statistically significant at one year (p<.05), but not at two years. In the only CsA-treated group which was excluded the recipients converted from CsA to Aza (3 cases), however, the graft survival rates at one and two years were 91% and 91%, which was statistically significant (p = .006, p = .0056) (Table 7, Fig. 2).

Patient and Renal Allograft Survival Reates in Renal Transplant Recipient According, to Either the Aza-(n=147) or CsA-(n=53) Treated Group
3. Results According to Donor Sources
The actuarial graft survival rates at two years posttransplant in all LRD, NRD and CAD were 73 %, 42% and 56%, respectively. There was a statistically significant difference between LRD and NRD (P = .0054), however, no statistical significance was noted between LRD and CAD (p = .317), and NRD and CAD (p = .714). The actuarial graft survival rates at two years posttransplant for Aza- and CsA-treated recipients were 68% and 84 %, respectively, in all LRD group. There was no significant difference between CsA- and Aza-treated groups (p = .29). Within all CsA-treated 84 % and 67%, respectively. None of the differences in graft survival rates between LRD and NRD groups within the all CsA-treated recipient, was statistically significant (p = .56). Within all Aza-treated recipients, the actuarial graft survival rates of LRD and NRD at two years were 68% and 40%, respectively, and the differences in graft survival rates between LRD and NRD were statistically significant (p = .016) (Fig. 3,4,5).

(D) Renal allograft functional survival rates in patients according to related (N=168), non-related (N=23) and cadavers (N=9).
(E) Renal allograft functional survival rates in all related patient according to Aza-(N=I20) and CsA-treated group (N=48).
4. Results According to Primary and Secondary Transplants
The actuarial graft survival rates for the primary transplants at two years for CsA- and Aza-treated recipients were 79% and 65%, respectively. The actuarial graft survival rates for the secondary transplants at two years for CsA- and Aza-treated recipients were 100% and 57%, respectively. There were no significant differences in survival rates between CsA- and Aza-treated recipients of primary grafts (p = .016), however, there was a significant difference on survival rates between CsA- and Aza-treated recipients of secondary grafts (p = .022) (Fig. 6).
5. Results According to Transfusions
Twelve CsA treated transplants have been performed following donor-specific blood transfusions (DST). Within all CsA treated recipients, the acturial graft survival rates of DST (n = 12) and non-DST (n = 41) groups at six months and one year were 100% and 60%, and 93%, 87%, respectively. None of the differences in graft survival rates between DST and non-DST groups were statistically significant (p = .38). Within all non-specific transfusions, the actuarial graft survival rates for the group that received one to four pints and group that received more than five pints, were 85% and 77% respectively. There was no significant difference in survival rates between both groups (p = .36) (Fig. 7,8).

(J) Renal allograft functional survival rates in patients according to donor specific transfusion (N=12) and non-donor specific transfusion (N=41) in CsA treated recipients.
6. Results According to HLA and Immunosuppressive Regimen
Analysis of the actuarial graft survival rates at one year for CsA- and Aza-treated recipients revealed no benefit of HLA typing either in aggregate for HLA-A, B, and DR, and specifically for HLA-DR. In the Aza-treated group, the actuarial graft survival rate tended to be higher in the HLA identical LRD group (100%) than in either the haplo-identical (73%) or mismatched LRD group (80%), which was shown by a statistical difference between the HLA identical and haplo-identical LRD group. The CsA-treated group again showed the actuarial graft survival rate higher in the HLA identical LRD group (100%) than in either the haplo-identical (87%) or mismatched LRD group (100%), although the HLA identical group and mismatched LRD group could not be compared properly due to the small number of entries (Fig. 9, 10) (Table 8).

(L) (M) Graft survival following renal transplantation according to HCA matching grade and immunosuppressive therapy.
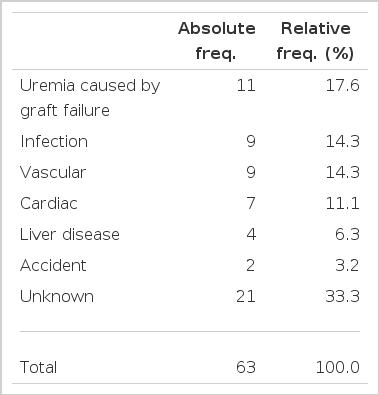
7. Causes of Death in Renal Transplant Recipients
Total number of deaths among the 200 cases represent 31.5% with 63 deaths. The most frequent cause of mortality was a result of uremia per se subsequent to graft rejection representing 17.5% (11 cases). It was followed by infections (14.3%), vascular (14.3%), cardiac diseases (11.1%) and others. Unknown causes of death accounted for one third of a total (21 cases) (Table 9).
8. Posttransplant Complications
There are numerous types of reported complications in transplant recipients. The authors listed some of the important complications we encountered in this study in Table 10. Posttransplant pneumonia was encountered 30 cases (15.0%), septicemia in 10 (5.0%), urinary tract infections in 28 (14.0%), and herpes simplex and herpes zoster infections in 11 and 13, respectively. Additionally, posttransplant diabetes mellitus was observed in 17 cases, and erythrocytosis in 36 cases. Although there were 14 cases of posttransplant aseptic necrosis, most of which were due to use of massive steroid along with the immunosuppressive regimen of Aza + PDN in initial stages of the renal transplantation, it was not observed after the switch was made to the CsA + PDN regimen. Furthermore, there were two cases of posttransplant autoimmune hemolytic anemia after the use of CsA + PDN. The complications due to technical errors were seen only during the initial stages of the renal transplantation and are seldom seen today (Table 10).
DISCUSSION
This report presents essential findings on all patients treated in the CMC nonrandomized trial of Aza vs CsA for immunosuppression.
The demographic features of the recipients included two diabetics and eight retransplants. 23 recipients in this study received grafts from HLA-mismatched NRD, and 9 recipients received grafts from CAD. The actuarial patient survival rates in the entire study group at two and four years were 75% and 68%, respectively. The corresponding graft survival rates for the group at two and four years were 68% and 57%. One and two year graft survival rates in all recipients in the CMC trial were 87% and 80% in CsA; and 74% and 65% in Aza-treated recipients (p<.05;NS). In the just CsA-treated group, however, the graft survival rate at one and two years were 91% and 91% which was significantly higher than those of Aza-treated group (p = .011, .0056).
In contrast, in the Minnesota trial, the one year cadaveric graft survival rates were 82% in CsA and 79% in Aza-treated recipients (p = .357)10); in the European multicenter trial, one year cadaveric graft survival rates were 72% in CsA and 52% in Aza-treated recipients (p = .001)11); in the Canadian multicenter trial the corresponding rates were 84 % and 67%12); and in the Michigan Medical Center trial, one year cadaveric graft survival rates were 77% in CsA and 62% in Aza-treated recipients (p = NS)13).
In the results according to donor sources, the actuarial graft survival rates at two-year posttransplant in all LRD, NRD, and CAD were 73%, 42%, and 56%, respectively. Among the all recipients group, the graft survival rate of the LRD group showed an excellent outcome. Within all LRD group, the graft for CsA-treated recipients had a 16% higher survival rate at two years than that Aza-treated recipients but it was not significantly different (p = .29). In the CsA-treated group, the graft for LRD indicated 14% higher survival rate at two years than that for NRD statistically insignificant difference (p = .56). In the Aza-treated recipients, however, the graft for LRD showed 28% higher survival rate at two years than that for NRD which is a statistically significant difference (p = .016).
Also, within all primary grafts, graft survival rate at two years in CsA-treated recipients tended to be higher than that of Aza-treated recipients (p = .13). Although the graft survival rate at one year in CsA-treated group was higher than that of Aza-treated group within all secondary grafts (p = .22), the entry numbers were so small that the analysis of result was not convincing.
Since the DST protocols introduction by Salvaterra (1978)14–16) at the University of California, the graft survival following DST pretreatment has been shown to be markedly better than in the non-DST treated haplo-identical groups, also, nonspecific pretransplant blood transfusion appears to confer an additional beneficial increment of approximately 10%, although this has not been identified in all studies. In this CMC trial, although 12 CsA-treated transplants have been performed following DST, none of the differences in graft survival rates between DST and non-DST groups were statistically significant (p = .38), because of a short time-period and a small of cases.
Within all HLA typed recipients, there was no benefit of HLA typing, either in aggregate for HLA-A,B and DR, or specifically for HLA-DR, on graft survival rates at a one year follow-up. However, base on the results according to HLA matching grade and immunosuppressive regimens, in either the Aza- or the CsA-treated group, the graft survival rates were higher in HLA identical LRD group than in either haplo-identical or mismatched LRD group. Although there has been a considerable amount of controversy over many years about the role of matching for HLA-A and -B antigens, there is now a consensus that a kidney that is well matched for the A and B antigens (that is: 0 or 1 mismatch) has about a 10 to 15% better chance of survival at 1 year than a graft that is badly matched (3 or 4 mismatches)17–22).
A total number of deaths among the studied 200 cases represent 31.5% of a total, which constitute 63 cases of death. The most frequent cause of mortality was a result of uremia per se subsequent to graft rejection representing 17.5% of a total (11 cases). During the initial stage of renal transplants in korea and prior to introduction of Korean National Medical Insurance in 1978, the recipient with graft rejection had passed away because there was no available replacement therapy for the graft failure or poor economic conditions at the time.
There are numerous types of reported complications in transplant recipients. Despite dramatic improvements in patients and renal allograft survivals, infections continue to be an important cause of posttransplantation morbidity and mortality. In the CMC trial, posttransplant pneumonia was seen in 30 cases (15.0%). Although infections occurred significantly less frequently in CsA-treated than in Aza-treated patients, Yoon et al. (1986) reported 6 cases of severe pneumonia in the CsA-treated transplant patients23). Evaluation of infected renal transplant patients should be guided by four major considerations as follows; 1) recognition of opportunistic microorganisms, 2) timing of fever after kidney transplantation, 3) epidemiologic factor, i.e., geographic, nosocomial factors, 4) evidence of specific organ system involvement24–25).
Erythrocytosis after renal transplantation had been noted as an uncommon complication. However, the incidence of erythrocytosis tended to be more frequent in CsA-treated group than in Aza-treated group. To date in this study group, 36 cases (18%) of postrenal transplantations erythrocytosis have occurred. Lee et al. (1986) reported 25 patients with erythrocytosis after renal transplantation26).
A group of 17(8.5%) recipients manifested posttransplant diabetes in the CMC trial, which is higher incidence of diabetes as compared to the Korean general population (3.5%). Yoon et al. (1985) reported 12 cases with posttransplant diabetes who survived over 60 months after the renal transpantation27).
Because of the relatively selective action on T-lymphocytes, CsA therapy causes fewer immunosuppressive complications in the form of infection or malignancy, as compared to previous Aza regimens, which were relatively nonspecific in their spectrum of action on lymphoid vs nonlymphoid cells. CsA-induced complications involve primarily the neuroectodermal, or the mesenchymal hepatic and renal system. In initial studies, Yoon et al noted a higher incidence of hypertrichosis (81%), hypertension (62%), tremor (57%), nephrotoxicity (43%), infection (43%), hyperkalemia (33%), hyperuricemia (33%), and hepatotoxicity (14%) in their study group. Despite numorous complications of CsA therapy, the major advantages of CsA therapy related to the improved graft survival rate, the lower incidence of rejection episodes, the lower infection rate, and the decreased hospitalization time. CsA mitigates risk factors heretofore presenting substantial obstacles to kidney transplantation: HLA matching, pretransplant splenectomy, extensive numbers of conditioning blood transfusions, and old age21–22,28–31).
In the future, in this authors’ view, chronic uremic patients should be free of disease. Kidney transplantation should be utilized more widely, and a few problems remaining for a future research are follows;
Cadaver donor should be available more frequently. In the European multicenter reports or U.S. reports show that a cadaver donor constitutes about 80% of a total. Furthermore, considering the fact that over 95% of the kidney transplantation in China is being performed with cadaver donor, one should look into political and ethical aspects of our present Korean polices on kidney transplantation.
In using CsA, there are many problems regarding such issues: the dose to achieve the best possible immunosuppressive effect and the least amount of side effects, successful conversion from CsA to Aza, differentiation of CsA nephrotoxicity, acute rejection and acute tubular necrosis, all of which can be caused by CsA.
Proper methods to manage grafts rejection, of which large dose methylprednisolone. ALG or CsA are curently used, but not without problems.
There are many known complications including infection. There should be more on-going research to prevent and/or treat the complications.
Methods for immunological monitoring for the graft rejection after kidney transplantation should be reevaluated.
There are other problems which the authors believe will be corrected sooner of later, in which case, chronic uremic patents will be blessed with love of God.