Problems in Endoscopic Sphincteropapillotomy
Article information
Abstract
Since 1976, endoscopic retrograde cholangiopancreatography(ERCP) has been done in 2,185 cases at Kwangju Christian Hospital in Kwangju, Korea, Between November 1981 and September 1986, endoscopic sphincteropapillotomy(EST) was performed on 194 patients. The results are as follows:
1) Common bile duct stones were found in 171 patients, ascaris in the common bile ducts of 12 patients, ascaris and stones in the common bile duct of 1 patient, clonorchis in the bile ducts of 4 patients, fibrotic stenosis of the periampullary choledochoduodenal fistula in 1 patient, stenosis of the common bile duct in 1 patient and stones in the pancreatic ducts of 4 patients.
2) In five cases the stones were extracted under direct vision, in 61 cases the stones were passed in the stool, while in 66 cases stone elimination was confirmed by repeated ERCP or T-tube cholangiography. In 46 cases the stones were not removed, but symptoms and laboratory findings showed marked improvement.
3) Complications following EST included 5 cases of bleeding, 1 case of acute pancreatitis with a pancreatic pseudocyst, one death due to sepsis following cholangitis, 5 cases of recurrent cholangitis and 2 cases of recurrent pancreatitis.
4) The conditions under which EST became difficult or did not succeed included periampullary diverticula, fibrotic stenosis of ampulla of Vater and stones in the intrahepatic ducts or a gallbladder.
5) With improved EST technical maneuverability, we could prevent bleeding and acute pancreatitis with a pancreatic pseudocyst and perform EST successfully in cases with periampullary diverticula.
INTRODUCTION
Recent developments in gastroenterology have lead to the wide use of endoscopic procedures in the diagnosis and treatment of disorders of the entire digestive system. Endoscopic sphincteropapillotomy (EST) is a therapeutic step above endoscopic retrograde cholangiopancreatography (ERCP). EST was developed by Demling and Classen1) in West Germany, and by Kawai and his coworkers2) in Japan. It allows common bile duct stones to be removed from high-risk surgical patients without having them undergo laparotomies. At present, it is widely performed in Western Europe1,3–7), Japan8,9) and the United States10,11).
MATERIALS AND METHODS
1. Materials
Of 2,185 cases of ERCP(Table 1), biliary tract diseases were found in 813(37.2%) cases, pancreatic diseases in 742(34.0%) cases, obstruction of the ampulla of Vater in 101(4.6%) cases, and normal findings in 475(21.7%) cases. Of 194 patients on whom EST was performed, common bile duct stones were found in 171 patients, ascaris in the common bile ducts of 12 patients, ascaris and stones in the common bile duct of 1 patient, clonorchis in the bile ducts of 4 patients, fibrotic stenosis of the periampullary choledochoduodenal fistula in 1 patient, stenosis of the common bile duct in 1 patient, and stones in the pancreatic ducts of 4 patients.
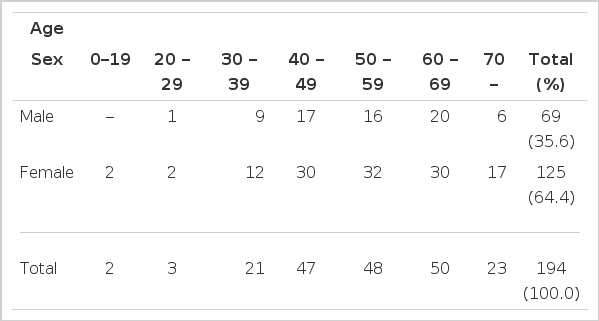
1) Age and Sex (Table 2)
The majority of patients (145 patients; 74.7%) were in the fifth to seventh decades of life. There were 69 male patients (35.6%) and 125 female patients (64.4%).
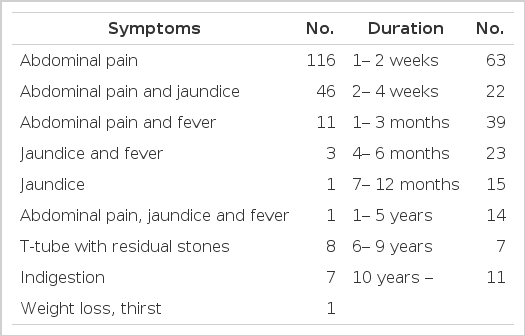
2) Clinical Symptoms (Table 3)
Abdominal pain was the presenting symptom in 174 (89.7%) patients, jaundice in 51 (26.3%) patients, and fever in 15 (7.7%) patients. Eight patients displayed residual stones on T-tube cholangiography. The duration of the chief complaints was variable from days to decades.
3) Laboratory Results and Liver Scan Findings (Table 4)
Blood hemoglobin levels were above 12 g/dl in 122 cases, 8 to 12 g/dl in 71 cases, and less than 8 g/dl in 1 case. White blood cell counts were less than 10,000/mm3 in 114 cases, 10,000 to 20,000/mm3 in 68 cases, and above 20,000/mm3 in 12 cases. Serum glutamic oxaloacetic transaminase levels were below 40 Interntional Units (IU)/ml in 72 cases (37%), 100 to 199 IU/ml in 32 cases and above 200 IU/ml in 20 cases. Serum total bilirubin levels were over 5 mg/dl in 36 cases and less than 2.5 mg/dl in 107 cases (55%). Serum alkaline phosphatase levels were below 3 Bessey-Lowry units in 35 cases (18%) and over 6 B-L units in 119 cases (61%). Liver scans showed normal findings in 61 cases, diffuse enlargement of the liver in 72 cases, and cirrhosis of the liver in 3 cases. In 52 cases (27%) a liver scan was not performed.
2. Methods
Patients were prepared in the same manner as for ERCP. All of the patients were admitted to the hospital and given routine laboratory test, including coagulation profiles, and two or three units of blood were crossmatched for each as a precaution. Using the FD-XL, MS 100 Electrosurgical Unit, the papillotome was inserted accurately into the common bile duct. The sphincter of Oddi was incised with an electric knife which was applied to the 11 to 12 o’clock sector of the ampulla of Vater. EST was completed within 30 minutes. The patient was carefully monitored for 24 hours following the procedure and was not allowed any food.
RESULTS
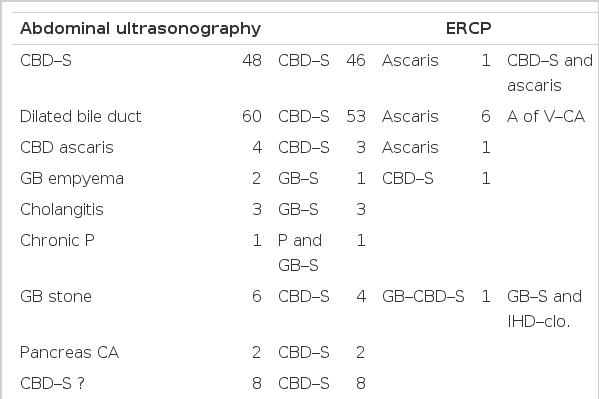
1. Comparison of Abdominal Ultrasonography with ERCP in the Diagnosis of Disease (Table 5)
Abdominal ultrasonography was performed on 171 cases. In 47 (33.1%) of 142 cases in which ERCP showed common bile duct stones, abdominal ultrasonography gave the correct diagnosis. In 151 (90.4%) of 167 cases in which ERCP revealed common bile duct diseases, abdominal ultrasonography made the correct diagnosis.
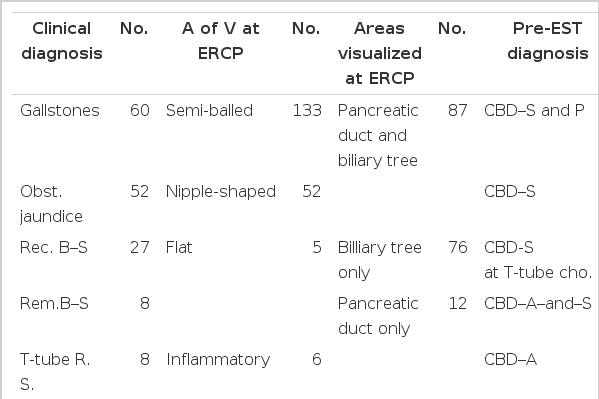
2. Clinical Diagnoses and Findings of ERCP (Table 6)
Gallstones, obstructive jaundice, recurrent biliary stones, and common bile duct stones were the clinical diagnoses in 160(82%) cases. The ampulla of Vater was shaped like a half ball in 133(69%) cases. The pancreatic duct and biliary tree were visualized by ERCP in 87 cases, only the biliary tree in 76 cases and only the pancreatic duct in 12 cases. Both T-tube cholangiography and ERCP were performed in 3 cases, and both percutaneous transhepatic cholangiography and ERCP in 7 cases. Common bile duct stones and pancreatitis were found by ERCP in 88 cases, common bile duct stones alone by ERCP in 171 cases, common bile duct stones by T-tube cholangiography in 8 cases, ascaris in the common bile ducts in 12 cases and so on.
3. The Results of EST (Table 7)
In 116 patients EST was performed once, in 49 patients twice, in 19 patients three times, and in 6 patients four times. In the 4 patients whose biliary trees were not visualized by ERCP, EST was performed for diagnostic purposes. The papillotome was inserted accurately into the common bile duct, common bile duct stones were visualized by ERCP, and then EST allowed the removal of the stones. Stones were extracted under direct visualization from 5 patients (2.5%), and were found in the stools of 61 patients (31.4%). Stone elimination was confirmed by repeated ERCP or T-tube cholangiography in 66 patients (33.5%). Not all stones were removed from 46 patients (23.7%), and improvement was noted only in symptoms and laboratory findings. EST failed in 15 cases (7.7%), and 1 patient (0.5%) died following the procedure. Hence, stone elimination was confirmed in 132 cases (68.0%). Including the 46 cases in which improvement was noted only in symptoms and laboratory findings, EST is thought to have been performed successfully in 178 patients (91.8%).
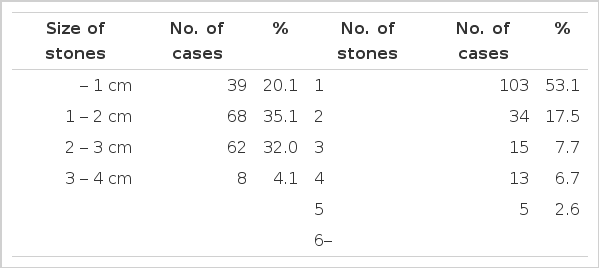
4. The Size and Number of Stones Extracted (Table 8)
The size of the stones was less than 1 cm in 39 cases(20.1%), and ranged from 1 to 3 cm in 130 cases(67.0%). In 103 cases(53.1%) only 1 stone was found, while in 7 cases, 6 or more stones were found.
5. Post-EST Surgery
A number of cases required surgery following the EST procedure. The associated problems included hemorrhaging (4 cases), periampullary diverticula (1 case), fibrotic stenosis of the ampulla of Vater (6 cases), symptomatic improvement only (1 case), pancreatic cancer (1 case), peritonitis (1 case), residual stones (3 cases), and nonexistent ascarides (1 case). In the remaining 176 cases no surgery was necessary after EST.
6. Complications after EST
Four patients required surgery to correct bleeding problems following EST. Another patient also hemorrhaged after EST, but the bleeding stopped spontaneously, and repeated ERCP showed no stones in the common bile duct. Acute pancreatitis with a pancreatic pseudocyst developed after EST in a patient with an impacted stone, however this problem was resolved with medical treatment. Six patients with a fibrotic stenosis of the ampulla of Vater required surgery after EST failure. A patient with a periampullary diverticula underwent surgery after EST failure. A patient died of cholangitis culminating in septicemia following a second EST procedure. A patient was surgerized because of pentonitis after EST. The serum amylase level increased in 20 patients after EST, but this finding may develop after ERCP.
7. Follow-up after EST
The patients who were admitted to our hospital within two months to two years and two months after EST showed the following features: (1) chronic pancreatits found at repeated ERCP (two months later), (2) passage of stones after the fourth EST (three months later), (3) passage of stones after the third EST (four months later), (4) acute gastroenteritis (five months later), (5) cholangitis with no common bile duct stones at repeated ERCP (six months later), (6) passage of stones after the second EST (eight months later), (7) cholangitis progressing to a moribund condition (one year later), (8) chronic pancreatitis (one year and one month later), (9) cholangitis with no common bile duct stones at repeated ERCP (one year and three months later), (10) chronic pancreatitis (one year and three months later), and (11) multiple common bile duct stones found on repeated ERCP and eliminated after repeated EST (two years and two months later).
8. Problems in EST
Hemorrhaging developed in 5 patients immediately following EST. Four of them developed bleeding during the initial EST studies, while the 5th case of hemorrhage occurred in the second half of the studies. Therefore, it seems that bleeding was due to poor technique and that the frequency of bleeding decreased with improved technical maneuverability and skill.
EST was not successful in the patient with the periampullary diverticula. However, as EST techniques improve, periampullary diverticula likely will not be a major cause of EST failure.
EST was not successful in the 6 patients with fibrotic stenosis of the ampulla of Vater. Even with improved EST techniques, fibrotic stenosis of the ampulla of Vater seems to be one of the major causes of failure.
Acute pancreatitis with a pancreatic pseudocyst developed in a patient with an impacted stone in the distal common bile duct. This case was noted in our early EST studies. In the later studies, we incised the ampulla of Vater more deeply with a papillotome and the aforementioned complications did not develop.
However, another patient had an impacted stone in the distal common bile duct, EST was failed, and the stone was not removed.
A patient developed septicemia following cholangitis after undergoing a second EST procedure.
Recurrent cholangitis and recurrent pancreatitis developed in 5 and 2 patients, respectively, following hospital discharge. Therefore, if fever or abdominal pain develops after EST, the patient should be examined by a physician.
One patient developed bleeding from the ampulla of Vater after it was cut by the papillotome and the EST was failed.
We cannot remove stones impacted in the intrahepatic ducts or in the gallbladder with the EST procedure.
DISCUSSION
Generally, the indications of EST3,12–15) include (1) recurrent or residual stone(s) following cholecystectomy, (2) choledocholithiasis in high-risk surgical patients16), (3) benign papillary stenosis, (4) malignant tumors of the papilla17), (5) gallstone pancreatitis18), and (6) diagnostic purposes(any ductal abnormalities suggesting tumor or inflammation).
The contraindications for EST3,12) include blood coagulation disorders, a long stricture of the distal common bile duct, abnormalities of the proximal bile ducts, large stones (>2.5 cm), acute pancreatitis and so on. Significant coagulation defects can be determined with a standardized hematological profile which includes prothrombin time, partial thromboplastin time, and bleeding time. In the cases with blood coagulation disorders, EST can be safely performed after medical treatment with fresh frozen plasma or specific coagulation factors19).
If there is a long stricture of the distal common bile duct, an operative procedure is required. When the anatomic structure of the ampulla of Vater is not clear, EST should not be done.
There is a report20) that even giant stones may pass spontaneously. In our study, stones of 2 to 3 cm in diameter passed in the stools in 62 cases and stones of 3 to 4 cm in diameter in 8 cases. But it is difficult to remove common bile duct stones larger than 2.5 cm in diameter with the use of EST procedures. There have been reports21–23) that for the removal of the large stones electrohydraulic lithotripsy and an ultrasonic drill are used to break up common bile duct stones.
When there is acute pancreatitis, EST is contraindicated. But, in the case of gallstone pancreatitis,24) EST is encouraged.
In our study, stones were extracted under direct vision from 5 patients(2.5%), they were found in the stools of 61 patients(31.4%) and stone elimination was confirmed by repeated ERCP or T-tube cholangiography in 66 patients(33.5%). In 46 patients(23.7%), not all of the stones were removed and improvement was noted only in the symptoms and laboratory findings. Of more than 3,000 cases of EST performed in Europe and the United States25), stones were eliminated with a Dormia basket in 31 to 32% of the cases and they were found in the stool in 54 to 63% of the cases. EST was considered successful if all stones were removed from the common bile duct or if a patient with papillary stenosis was relieved of pain and/or cholestasis12). In our study, the success rate of EST was 91.8% and it was comparable to 89%12), 93.8%26) etc. reported in large series.
The complications following EST include bleeding, cholangitis, pancreatitis, and retroperitoneal perforation. Bleeding post EST develops more frequently than the other complications. It usually develops immediately following EST, but there is a report27) of bleeding occurring 7 days after EST. In our experience, an accurate incision in the 11 to 12 o’clock sector of the ampulla of Vater would be safe from bleeding. In our study, bleeding developed in 5 patients. Four of them had bleeding problems during the initial period in which EST had been performed. Only one of them developed bleeding in the latter half of that period. Therefore, it seems that the frequency of bleeding decreases with acquired skill in EST.
Cholangitis may develop due to a prolonged EST procedure, recurrent instrumentation, or inadequate biliary drainage. In the last condition, biliary drainage utilizing a nasobiliary catheter can decrease the risk of cholangitis28). We administered antibiotics before and after EST to prevent the cholangitis. In our study, 1 case of acute cholangitis developed after the second EST procedure, and recurrent cholangitis developed in 5 patients following discharge from our hospital. Therefore, if fever or abdominal pain develops post EST, the patient should be examined by a physician.
Pancreatitis frequently develops when the pancreatic duct is cut or when the ampulla of Vater is excessively coagulated with no relation to the pancreatic duct, but rarely when there is a gallstone impacted in the common duct29). Pancreatitis usually improves with antibiotics and conservative treatment. In our study, acute pancreatitis and a pancreatic pseudocyst developed after EST in a patient with an impacted stone in the distal common bile duct. This case was noted during the first half of our EST experience. In the second half of that period, we incised the ampulla of Vater more deeply with a papillotome and no complications developed. Recurrent pancreatitis developed in 2 patients after they were discharged from our hospital. Transient hyperamylasemia is common after EST (indeed, even after diagnostic ERCP), and it is therefore difficult to define the true incidence of pancreatitis30). In our study, 20 cases showed an increased serum amylase level after EST, and all recovered after medical treatment.
Perforation of the bile duct or duodenal wall is a rare complication12,30). Retroperitoneal perforation is usually treated with antibiotics and nasogastric suction. In our study, no retroperitoneal perforation developed.
Other conditions that make EST difficult or easily fail include periampullary diverticula, fibrotic stenosis of ampulla of Vater, stones in the intrahepatic bile ducts or in a gallbladder, or Billroth II gastrectomy. Also, EST is technically difficult. In our study EST failed in 1 patient with periampullary diverticula. With improved EST techniques, periampullary diverticula do not seem to be one of the major causes of EST failure. However, it sometimes becomes difficult to insert a sphincterotome into the common bile duct and great care should be taken to direct the sphincterotome accurately. In these conditions fluoroscopy and radiographic confirmation of catheter placement allow safe EST31).
During our entire study, EST did not succeed in only 6 patients with a fibrotic stenosis of the ampulla of Vater. With the cannula inserted into the common bile duct by 0.5 cm, ERCP becomes possible. In contrast, in the EST procedure, the papillotome should be inserted into the common duct to a depth of 3 to 4 cm. Therefore, fibrotic stenosis of ampulla of Vater makes EST impossible.
Stones cannot be removed from the intrahepatic ducts or from a gallbladder with the EST procedure.
EST is also difficult after a Billroth II partial gastrectomy, since the papilla must be approached through the afferent loop. These anatomic situations provide difficult technical problems which sometimes cannot be overcome by EST, thus justifying the lower reported success rate (50 to 80%)32–34).
EST is a procedure requiring a high degree of skill. The endoscopist must have extensive experience with ERCP. He should be able to cannulate the bile duct quickly and easily in 50 to 70% of patients and be able to obtain cholangiograms in 80 to 90% of cases. To reach this level of expertise, 200 to 300 ERCP examinations are required12).
To estimate the efficacy of EST, it is necessary to know its long-term results. Restenosis of the ampulla of Vater is one of the long-term problems following EST35). Geenen and his coworkers20) reported no stenosis or obstruction of the common bile duct during a follow-up period of 6 to 12 months in 13 of the patients. Nakajima and his coworkers36) reported no stenosis in 14 patients during a follow-up period of 16 months. Safrany and his coworkers37) observed stenosis of the ampulla of Vater in 2 of the 50 patients followed up. In 1979, the stenosis of the common bile duct post EST was reported as 1% in Japan38). In our study during the follow-up period of up to 2 years and 3 months, no restenosis of the ampulla of Vater was observed. Cholangitis was found in 3 patients, chronic pancreatitis in 3 patients, and acute gastroenteritis in 1 patient.
In our study 1 patient (0.5%) died following EST. In Europe and the United States the rate of death following EST was reported as 1.2 to 1.4%12,39,40). This rate is lower than the mortality rate of 2.1%41) following a reoperation of the common bile duct. Therefore, EST is considered to be a relatively safe procedure in high-risk surgical patients with common bile duct stones.