Early Gastric Cancer in Korea
Article information
Abstract
We reviewed the 639 cases of early gastric cancer from nation-wide 16 medical centers. The proportion of early gastric cancer among surgically resected gastric carcinoma comprised 6 to 12 percent. Male to female ratio was 1.7 to 1 with male preponderance. Mean ages of the early gastric cancer was 49.0 years and most prevalent ages was 5th decade. Macroscopically type IIc was most prevalent, reaching 59.9 percent. Depressed type lesions was more frequent than elevated type lesions by four folds. The size of lesions less than 4 cm accounted for more than 80 percent. Most frequent site of lesions were lower third by the CMA classification and lesser curvature transectionally. Lymph node metastasis was observed in 10.9 percent of all cases and it was more frequent in large tumor size more than 4 cm, elevated type, and undifferentiated carcinoma. 5-year survival rate was 91.6 percent. Gastrofiberscopic examination was superior to that of radiological examination in the diagnosis of early gastric cancer.
INTRODUCTION
By the statistics of mortality returns in Korea, gastric carcinoma ranks first among the cancer death. In spite of the decreasing trend in the incidence of gastric carcinoma in western countries, the detection frequency of the gastric carcinoma are in increasing trend because of the nation-wide execution of the medical insurance system, increasing concern about health and improved diagnostic technology. However, in a point of therapeutic view various forms of therapeutic modalities except early surgical excision are failed to show any significant increase in 5 year survival rate.
In Japan, after the tuberculosis was overcome in some degree many researchers have worked on countermeasure against cancer. Twenty-seven years have passed since the definition and classification of early gastric cancer was proposed by Tasaka at the 4th General Meeting of the Japan Society of Gastroenterological Endoscopy in 1962. Thereafter pan-national efforts to find out early gastric cancer produced a remarkable increase in the number of early gastric cancer. By the recent report in Japan early gastric cancer account for more than 50 percent of the total gastric carcinoma. 5-year survival rate also increased more than 90 percent. Thus, early gastric cancer is recognized as a potentially curable malignancy if it to be detected at early stage.
In our country, it takes an increasing interest in early gastric cancer with the spread of endoscopic examination even in a private clinic and generalized application of the upper gastrointestinal series in the diagnosis of dyspeptic patients, but the discovery rate remains very low even in the level of general hospital or university hospital and as yet we have no nation-wide report.
For the purpose of recognizing the problems with which our country is faced, we pursued a clinical investigation about the 639 cases of early gastric cancer confirmed by operation from 16 medical centers.
SUBJECTS AND METHODS
1. Subjects
The subjects of investigation were 639 cases of early gastric cancer confirmed by operation from national 16 medical centers.
2. Methods
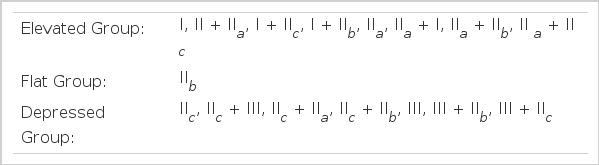
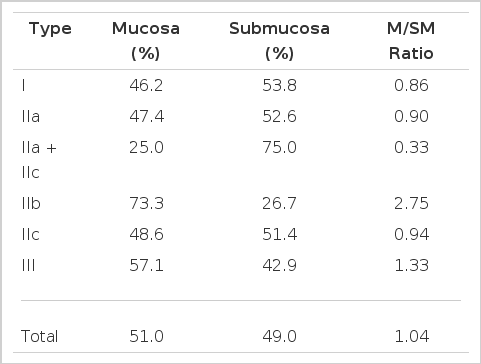
The classification of the early gastric cancer was based on the General rules issued by the Japanese Research Society for Gastric Cancer Study (JRSGC)12,13). Major types were classified into the type I, IIa, IIa + IIc, IIb, IIc, and III. These were grouped with elevated, flat and depressed groups (Fig. 1. Table 1,2).
The cancer lesions were divided according to the largest diameter into 5 groups less than 5mm, 6 to 10mm, 11 to 20mm, 21 to 40 mm and more than 40mm.
Location of the lesion was recorded by virtue of the CMA classification issued by the Japanese Research Society for Gastric Cancer Study12,13): C (upper one third), M (middle one third), and A (lower one third). Cross sectional circumference of the stomach was separated into four parts, namely the lesser curvature (LC), the anterior wall (AW), the greater curvature (GC), and the posterior wall (PW).
By the depth of cancer invasion, early gastric cancer was subclassified with mucosal and submucosal cancer. Mucosal cancer was defined as the tumor confined to a mucosa and submucosal cancer invaded the submucosa.
Histological recording was made according to the WHO classification, namely papillary adenocarcinoma, tubular adenocarcinoma, poorly differentiated adenocarcinoma, signet ring cell carcinoma and the others.
The presence or absence of the metastasis was made by histological examination in a resected lymph node or neighboring organs.
We get the 5 year survival rate by the life table method in 93 patients whose follow up examination after operation was done regularly.
RESULTS
1. Age and Sex Distribution
The mean age of the patients was 49.0 years (male 49.7 yrs, female 47.9 yrs) and male to female ratio was 1.7 to 1. Patients in their 40’s were most frequently observed, reaching 31.0%, followed by those in their 50’s, 30’s and 60’s. Age versus female to male ratio was most high in their 20’s (Fig. 2). But the difference decreased as increasing ages (Fig. 3).
2. Macroscopic Features
Depressed group was more prevalent with the ratio of 4 to 1 than elevated and flat group. The most frequent type was the IIc, reaching 59.9%, and following by III, I, IIa + IIc, and IIb. The age distribution of elevated type showed a “beak” shape with the mode at the 6th decade, and that of depressed type had a “plateau” shape with the mode at 4th, 5th and 6th decades (Fig. 4, 5).
3. Size of the Lesion
Lesions measuring 1.1 to 2.0 cm were found most frequently in 29.3%. Lesions less than 4.0 cm comprised 85.3% of the total. So called “minute cancer” less than 5mm was 5.5% (Fig. 6). Size difference in relation to age or sex was not observed. There was a trend that size of the lesion was more larger in elevated group than depressed group.
4. Site of the Lesion
As depicted in Fig. 7, we classified the lesion by CMA classification and transectional location.

Location of early gastric cancer.
C : Upper 1/3 of the stomach
M : Middle 1/3 of the stomach
A : Lower 1/3 of the stomach
GC: Greater curvature
AW: Anterior wall
LC : Lesser curvature
PW: Posterior wall
The lower third (A) accounted for 69.9% and the upper third (C) accounted for only 3.2%.Transectionaliy, lesions on the lesser curvature comprised 66.2%. There was no significant difference between distribution of location in relation to macroscopic features.
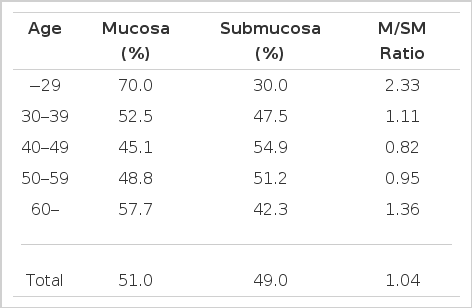
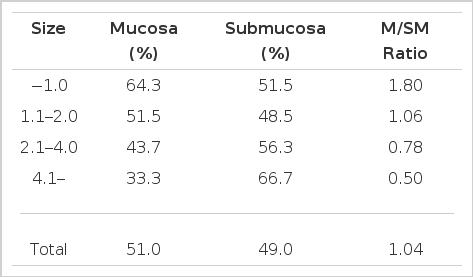
5. Invasion
Mucosal cancer comprised 51.0% and submucosal cancer in 49.0%. Mucosal cancer was more prevalent in 3rd and 7th decades, type IIb, and small sized lesions. In contrast, submucosal cancer was more prevalent in 5th and 6th decades, type IIa +IIc, and more large sized lesions.
There was close correlation between the size and invasion. That is, more larger the size, more invasive the lesion. Regarding the depth of invasion, age, macroscopic type and size of the lesion were the major influencing factors (Table 3,4,5).
6. Histological Types
We divided the histological types into papillary adenocarcinoma, tubular adenocarcinoma, poorly differentiated adenocarcinoma, signet ring cell carcinoma and others. We also divide the histological types by the degree of differentiation into undifferentiated and differentiated types.
Tubular adenocarcinoma was more frequent in elevated types. On the other hand the relative incidence of signet ring cell carcinoma was more frequently observed in depressed lesions and lower third. Undifferentiated carcinoma was more frequent in younger persons (3rd and 4th decades) and female. In contrast differentiated type showed a tendency to increase as the ages increase and size of the lesions become smaller (Fig. 8,9,10).
7. Lymph Node Metastasis
Lymph node metastasis was identified in 10.3% of all cases. The frequency of metastasis was associated with age, macroscopic type and size of the lesion. The incidence of metastasis was most frequently observed in 5th decade (16.4%) macroscopic type I (17.6%) and tumor size larger than 4cm (24.4%) (Fig. 12, 13). Significant difference in the frequency of metastasis according to the location was not observed, but relative incidence was higher in middle third and anterior wall. As depicted in table 6, lymph node metastasis regarding to the depth of invasion revealed that more deep the depth of invasion, more frequent the metastasis.

Preoperative diagnosis of early gastric cancer.
EGC: Early gastric cancer
AGC: Advanced gastric cancer
8. Diagnostic Modality
Correct diagnosis as early gastric cancer was given in 56.8%. The others were diagnosed as benign lesions or advanced gastric cancer. Endoscopic examination with biopsy was the better method for the diagnosis of early gastric cancer than radiological examination. By the endoscopic examination 87.5% of all cases were diagnosed as malignant disease, whereas radiologic examination suspected malignancy in only 60% (Table 7, Fig. 13).
DISCUSSION
Despite the declining trend in the incidence of gastric carcinoma in western countries, it remains the most common cause of death from malignant disease world-wide1–4). In Korea the detection frequency has been increased in recent years because of nation-wide medical insurance system, increased concern about health and Improved diagnostic technology. In Japan, a quarter of a century have passed since the definition and classification of early gastric cancer by Tasaka5) in 1962. In the initial stages of the classification, it was difficult to demonstrate a definite trend in early gastric cancer because of insufficient number of cases, lack of consistency in the interpretation, and the method application of the new classification. However nation-wide screening of the gastric carcinoma by mass survey increased the number of early gastric cancer more than 20,000 reported cases and enabled the statistical analysis of the chronological clinical-pathologic findings6,26,27). The actual circumstances of our country are insufficient to statistical analysis. Even a nation-wide collected report has not yet been made.
The purpose of this study was designed to recognize the problems which we are faced. The number of cases collected from 16 medical centers were 639 cases, but there were several problems in the interpretation of the clinical recordings because of interinstitutional variation and inadequate description. For example, classification application in macroscopic types, method of measurement in the size of lesion, and the histologic findings are inconsistent with among the institutions. Therefore it was considered what we have to do now is to unify the classification, and make a rule for patient care. In the point of patient care another problem was exposed that correct and thoroughful follow up was made in only a 15% (93 cases).
Early gastric cancer comprised 6 to 12 percent of all the surgically resected gastric cancer. This level was very low as compared with that of the Japan, 30 to 50%. In Japan 70% of the early gastric cancer was suspected from the private clinic. Thus the medical doctor in private clinic play a major role in the detection of early gastric cancer. In our country most of the cases have been detected in general hospital level, but it is promising that regular use of UGI series and more frequent endoscopic examination in dyspeptic patients being performed even in private clinic.
The mean ages of the early gastric cancer was 49 years. This result was younger than that of Japan by 6 years15,16,19). It was considered that average national life span may be the major point of difference.
Hirota et al20) who reported a chronological trend of the gastric carcinoma in Japan described that the number of elderly patients increased with time, especially those above the age of 70 years because of changes in age composition of the population due to increased average life span and changes in environmental factors. The male to female ratio was 1.7 to 1 with male preponderance. But as for the young patients below 30 years there showed a female predominance. This results was similar to that of Mori et al16).
Type IIc early gastric cancer was seen most frequently followed by those of III, I and IIa + IIc. Depressed types of early gastric cancer was more frequently found than elevated types. These results are similar to that of Japan. Hirota et al20) subdivide the IIc into shallow and deep IIc lesion and reported that the increasing trend in IIc lesion was attributable to the increase In shallow IIc lesion. The fact that this kind of shallow and smaller cancer has become readily detected may be influenced by histological diagnosis of the gastric biopsy specimen and improved diagnostic technique such as chromoscopy or strip biopsy7–11).
The fact that this kind of shallow and smaller cancer has become readily detected may be influenced by histological diagnosis of the gastric biopsy specimen and improved diagnostic technique such as chromoscopy or strip biopsy7–11).
There was close relation between tumor size and the depth of invasion. Intramucosal cancer was more frequently observed in minute gastric cancer those largest diameter is less than 5mm18), younger person less than 30 years and IIb lesion. In contrast submucosal cancer was more prevalent in larger tumor size, older ages and IIa + IIc lesion. These results was similar to that of Japan.
International or intranational variation was observed in the location of the lesion. In our result most frequent location was lower 1/3 (A), where as Park et al37) reported the incisura angularis as the most prevalent site. These variation was similar in Japan, by the report of Hirota et al20) there was increasing trend in A, where as Tagaki et al15) reported M has increased in 1970’s.
Unfortunately the symptoms of the gastric carcinoma is so nonspecific that most cases of gastric carcinoma are advanced when first diagnosed and beyond the scope of definitive therapy. In order to improve the survival rate we should make early diagnosis, namely diagnosis at an earlier pathological stages. 5 year survival rate for early gastric carcinoma in Japan would seem to be in excess of 90%, but the European reports25) are lower than Japanese reports. The difference in survival rate over sequential decades and that between Japan and other western countries may not be attributable to biological difference in malignancy itself but to the clinical stages of patients treatment.
The depth of invasion and lymph node metastasis are regarded as a most important prognostic parameter. In our results lymph node metastasis was closely related to the depth of invasion and size of the lesion. Lymph node metastasi was more frequent in submucosal cancer, tumor size more than 4cm and type IIa + IIc.
Basically, early gastric cancer was classified into three subtypes, protruded type, flat type, and depressed type. These were designed to aid in the identification of the lesions of radiology and endoscopy and does not necessarily reflect the growth characteristics of the carcinoma. These were several classifications in relation to the growth characteristics.
In the report of Lauren21) and Stemmermann et al22) diffuse type cancer may be expected to extend widely, whereas intestinal type appears to extend a few millimeters from the main tumor and shows a favorable prognosis. Ming23) classified the gastric cancer into expanding types and infiltrative types, and he described that infiltrative type showed poor prognosis. Recently Kodama et al30) have reclassified the early gastric cancer to take account of growth patterns, potentiality for recurrence and the prognosis.
In this scheme the growing histological features of the cancer and overall diameter are stressed. Cancers greater than 4cm in diameter and confined to mucosa are termed super M subtype or super SM subtype if the submucosa is reached. A lesion with a diameter of less than 4cm which invades the mucosa in a wide pattern is termed PEN A subtype if the cancer expands solidly through the muscularis mucosa or PEN B subtype if the penetration is irregular and fenestering. Small mucosal cancers are those which are less than 4cm and barely penetrate the submucosa. Super PEN B, and small mucosal cancers are characterized by a tendency to depressed lesions having a low incidence of lymph node metastasis and vessel invasion. In contrast PEN A subtypes are usually elevated lesions and have a propensity for lymph node involvement and vessel invasion. Recurrent cancer in the gastric remnant is more likely with the superficial spreading types. We did not reclassified the early gastric cancer by Lauren’s, Ming’s and Kodama’s classification. However as a means of subsidiary aids predicting the prognosis, these classification may be a useful parameter.
Controversy about the relative diagnostic accuracy of endoscopy compared with the double contrast barium meal study persists27–29,32–33). Most of the recent literature suggest that X-ray is less accurate and misses more lesions than endoscopy. There also appear to be different aspects from which the two diagnostic methods are to be compared, for example simple diagnostic efficiency, cost, frequency of complication and patient acceptibility27–29,32–33,36). In our results endoscopic examination with biopsy has better diagnostic accuracy than the radiologic examination. It is difficult to compare the treatment results between different institutions and countries. For this purpose the comparison should be performed on the common basis for description and definition of the extent of disease and treatment modalities. TMN classification or general rules issued by the Japanese Research Society for Gastric Cancer Study were established for the purpose of staging and to set the treatment plan for gastric carcinoma13,24). In our results overall 5-year survival rate was 91.6%. This results was similar to those of Japan and better than that of European results30,31). The difference in the treatment results of gastric carcinoma among countries may not be attributable to the malignancy itself but to the stage of the gastric cancer when the treatment has began. The only thing which remains to improve the treatment results of early gastric cancer is to find out the cancer more early state. In Japan, since the early sixties screening of the gastric carcinoma by mass survey using gastrocamera and fluoroscopic examination was performed. Nowadays annual detection rate of gastric carcinoma is about 0.1 % and the half of them are early gastric cancer. Nowadays overall survival rate of the gastric cancer reached at the level of 50%, which is extremely high than that of other countries14).
Acknowledgements
We thank the nation-wide 16 medical centers for the active cooperation.
Catholic University, Chonbuk National University, Chosun University, Chung-Ang University, Chungnam National University, Hanyang University, Korea University, Kwangju Christian Hospital, Kyung Hee University, Kyung Pook National University, Pusan National University, Seoul National University, Soon Chun Hyang University, Won Kwang University, Yonsei University