Manning Criteria in Irritable Bowel Syndrome: Its Diagnostic Significance
Article information
Abstract
Background:
Irritable bowel syndrome is one of the most commonly encountered gastrointestinal disorders, for which there are no established diagnostic criteria. Thus, a diagnosis of IBS is made by exclusion of any organic diseases. Recently, important attempts for the positive diagnosis of irritable bowel syndrome by questionnaire surveys of physical symptoms have been made. We performed a questionnaire survey to evaluate the diagnostic value of the Manning criteria and to observe the major symptoms in irritable bowel syndrome.
Methods:
A symptom questionnaire which consisted of 22 items, including 6 cardinal symptoms of the Manning criteria, were answered by 172 outpatients who had gastrointestinal complaints. According to a final diagnosis based on independent clinical evaluation, all patients were categorized in three groups: irritable bowel syndrome group, nonulcer dyspepsia group and organic gastrointestinal disease group. The results of the questionnaire were analyzed for each group.
Results:
The sensitivity and specificity of the Manning criteria for the diagnosis of irritable bowel syndrome were 67% and 70% if three or more items were regarded as positive. The mean score and overall frequency of the Manning criteria were significantly higher in irritable bowel syndrome group than in nonulcer dyspepsia (p<0.01) or organic gastointestinal disease group (p<0.05) Among subgroups of the irritable bowel syndrome group, the pain-predominant subgroup showed a significantly higher score and overall frequency than the painless subgroup(p<0.05).
Conclusions:
The Manning criteria would be useful as a simple and reliable backup tool for the diagnosis of irritable bowel syndrome and seem to be more useful in pain-predominant subgroup. More detailed history-taking should prevent unnecessary extensive investigations for the diagnosis of irritable bowel syndrome.
INTRODUCTION
Irritable bowel syndrome (IBS) is a very common clinical condition characterized by abdominal pain and alteration of bowel habits, or both, as the main symptoms. But these symptoms are also common in organic gastrointestinal diseases, and there are no established pathophysiologic mechanism and diagnostic procedure in IBS. Thus, a diagnosis of IBS is generally made by exclusion of any organic gastrointestinal diseases with similar symptoms.
It is amazing to see the expensive, dangerous and extensive workups to which healthy patients are subjected by physicians searching for an organic cause in patients who obviously suffer from IBS. It is difficult to decide how extensive investigations should be before the diagnosis of IBS may be accepted with reasonable confidence. To overcome this obstacle, important attempts for positive diagnosis of IBS from physical symptoms have been made by questionnaire surveys1–6). The application of refined symptoms criteria, selected from questionnaire surveys, may permit a more positive diagnosis of IBS and may help minimized the investigative procedures to exclude organic causes. Manning et al.1) have shown that certain symptoms derived from a 15-items questionnaire differentiated patients with IBS from patients with organic diseases. Subsequently, this empirical approach has been used commonly In clinical researches2–6), yet there are few data to confirm the validity of the Manning criteria. The purpose of the present study was to evaluate the reliability and discriminatory value of the Manning criteria in the differentiation of IBS from organic diseases and nonulcer dyspepsia. We also examined the frequency of additional symptoms to determine if other symptoms would provide additional discriminatory value.
MATERIALS AND METHODS
1. Patients
We studied 172 patients who attended the ouptatient clinic of the Department of Internal Medicine, Chungang University Hospital in 1991–1992 for the management of gastrointestinal complaints. All patients who consented to participate completed a questionnaire before their diagnostic evaluations. The final diagnosis for each patient was based on an independent clinical evaluation, supplemented by the results of investigations including endoscopy and barium studies. Responses to the questionnaire were not shown to examining physicians and were not used to arrive at the final diagnosis. According to the final diagnosis, all subjects were categorized in several groups and subgroups as follows: (1) Irritable bowel syndrome group: pain-predominant subgroup (pain>6 times/year) versus painless subgroup (pain≤6 times/year), constipation - predominant subgroup (stool<3 times/week or often hard) versus diarrhea-predominant subgroup (stool≥3 times/day or often loose), male subgroup versus female subgroup. (2) Nonulcer dyspepsia group. (3) Organic gastrointestinal disease group: upper bowel subgroup, lower bowel subgroup, other disease subgroup. The results of the questinnaire were analyzed for each group and each subgroup.
2. Questionnaire
The questionnaire used for the present study was modified from that of Talley NJ7). The questionnaire contained 22 items: 6 cardinal symptoms of the Manning criteria and 14 additional gastrointestinal symptoms. The six cardinal symptoms were (1) visible abdominal distension, (2) pain relief with defecation, (3) looser stools at pain onset, (4) more frequent stools at pain onset, (5) mucus per rectum, (6) feeling of incomplete evacuation.
3. Statistical Analysis
Kruskall-Wallis test was used to compare the overall frequency of the Manning criteria among the groups. Wilcoxon’s rank-sum test was used for the comparisons of this frequency among subgroups of the IBS group. Anova t-test and Chi-square test were used to compare the Manning criteria score (Number of criteria present) and the frequency of individual symptoms among the groups. Correlations between the Manning criteria score and several factors (sex, age, presence of abdominal pain) were evaluated by multiple regression analysis. Internal consistency of our questionnaire, using Cronbach’s α, was 0.78.
RESUTS
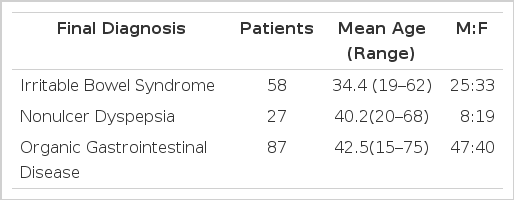
The characteristics of patients are summarized in Table 1. There were 58 patients with IBS, 27 patients with nonulcer dyspepsia and 87 patients with organic gastrointestinal diseases. The mean age of IBS group was younger than that of organic gastrointestinal disease group (34.4 years vs. 42.5 years). In IBS group, patient’s mean age was 36.2 years in male and 33.0 years in female, and there was a slight female preponderance.
The Manning criteria scores in each group and subgroups are shown in Table 2. The mean score of IBS group was higher than in nonulcer dyspepsia group and organic disease group (3.10±1.39 vs. 1,14±1.16, p<0.01; 1.82±1.55, p<0.05). Among IBS subgroups, the pain-predominant subgroup showed a higher score than the painless subgroup (3.38±1.39 vs. 2.63±1.29, p<0.05). The diagnostic sensitivity and specificity of the Manning criteria were 67% and 70% if three or more symptoms were regarded as positive, and 84% and 55% if two or more symptoms were regarded as positive.
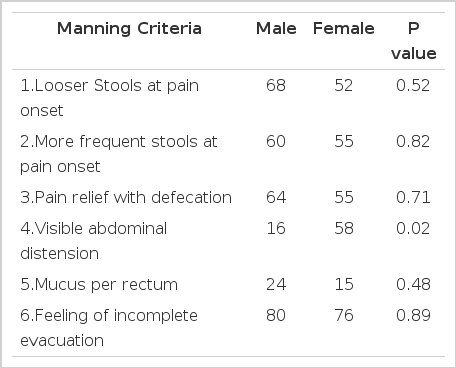
In IBS group, the overall frequency of six cardinal symptoms of the Manning criteria was significantly higher than in nonulcer dyspepsia group (p<0.01) and organic gastrointestinal disease group (p<0.02). Among the six symptoms of the Manning criteria, two symptoms, ‘more frequent stools at pain onset’ (p=0.01) and ‘pain relief with defecation’ (p=0.04), were significantly more frequent in IBS group than in organic disease group (Table 3). Among the IBS subgroups, the overall frequency in the pain-predominant subgroup was higher than the painless subgroup (p=0.02), but no significant difference was found between the male subgroup and the female subgroup (p=0.34) and between the constipation-predominant subgroup and the diarrhea-predominant subgroup (p=0.42). Only one symptom was significantly associated with female gender, ‘visible abdominal distension’(p=0.02) (Table 4).
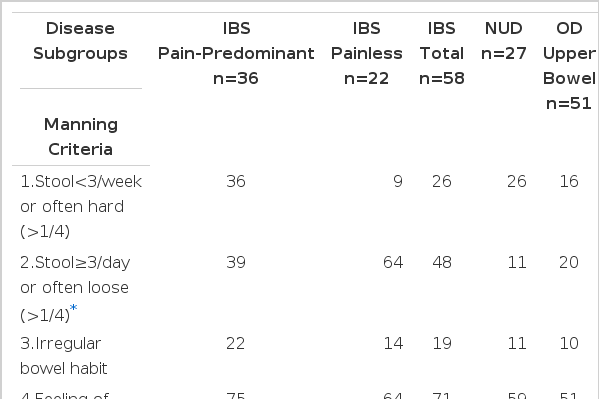
Frequency of the additional symptoms is summarized in Table 5. IBS group complained more frequently of abdominal distension, flatus, belch or indigestion, longer duration of symptom, and stress or nervous character than organic gastrointestinal disease group. But only ‘stool≥3/day or often loose (>1/4)’ was significantly more frequent in IBS group (Table 5).
The Manning criteria score was closely correlated to the presence of abdominal pain (r=0.672, p<0,001), but not to age (r=0.034, p=0.16) or sex (r=0.010, p=0.93).
DISCUSSION
Irritable bowel syndrome (IBS) has been reported to account for 20–50% of referrals to the gastroenterology clinic8) and 14–22% of selected, apparently health adults in qustionnaire surveys9). One recent epidemiologic data showed that IBS was the most common diagnosis accounting for 10.4% of all digestive disease diagnoses in the United States10). Also Sandler’s prevalence data indicated a prevalance rate of 2.9%, so nearly 5 million people have had IBS. There are between 2.5 and 3.5 million physician visits yearly, and more than 2 million prescriptions are written11).
At present, pathophysiologic mechanism, cause of chronic symptom complex of IBS, is largely unknown, but thought to be primarily altered gastrointestinal motility. Patients with IBS have been shown to exhibit exaggerated sigmoid motor response12–14), delayed gastrocolic response to meal15,16), predominant frequency of 3 cycles/minute in colonic myoelectric activity16,17), lowered visceral sensory threshold to pain caused by balloon distension18,19), abnormal rectal sensitivity and pressure response to balloon dilation20), altered visceral afferent mechanism21), modified small bowel motility22), delayed colonic transit of diets23,25) and associations with neurohormonal effect or gastrointestinal hormones. Also, evidence of significant psychological disturbance may be seen in some patients with IBS26,28), but reported higher prevalence of psychopathology among the patient population with IBS may be due to behavioral influences that lead to health care seeking29).
In spite of many previous studies, a diagnosis of IBS may still be made by exclusion of any organic gastrointestinal diseases with similar symptoms. Clinicians who are afraid of overlooking organic disease, including malignancy, tend to make the diagnosis of IBS with reluctance and to pursue extensive, often unnecessary investigations. To overcome these problems, questionnaire survey methods have been introduced. Several investigators have attempted to identify more specific symptoms and physical findings that would enable them to distinguish IBS from organic gastrointestinal disease. Manning et al.1) have shown that six cardinal symptoms derived from a 15-items questionnaire differentiated patients with IBS from other patients at a 84% of sensitivity. Talley et al.7) have applied this criteria to 361 patients by questionnaire survey. Its diagnostic sensitivity and specificty for IBS were 56% and 77%. Kruis et al.5) have reported a weighted scoring system for the diagnosis of IBS incorporating the case history, physical findings, and some basic investigations with a 83% of sensitivity and a 97% of specificity. Similarly, Talley’s scoring system with high reliability was introduced4,30). However, there was some dispute about the limitation of questionnaire surveys in the differentiation of IBS from organic lower bowel disease31).
Our results were similar to those of previous studies. Diagnostic sensitivity and specificity of the Manning criteria were 67% and 70%. The Manning criteria score and overall frequency were significantly higher in patients with IBS than in patients with nonulcer dyspepsia or organic gastrointestinal disease. Among subgroups of the IBS groups, the pain-predominant subgroup showed higher score and frequency than the painless subgroup. Also, regression analysis showed close correlation between the Manning criteria score and presence of abdominal pain. With the above results, we expect that the Manning criteria is useful as a backup tool for the diagnosis of IBS and more specific in pain-predominant IBS subgroup. Among the individual symptoms, ‘more frequent stools at pain onset’ and ‘pain relief with defecation’ were significantly more frequent in IBS group compared with organic gastrointestinal disease group. These two symptoms were in concordance with ‘irritable bowel factors’32), which were relief of pain with defecation, looser stools with pain onset, more frequent stools with pain, and gastrointestinal reactions to eating. Additional symptoms with significant difference were not found, which coincides with the results of Talley et al7). Smith et al.33) reported that the Manning criteria is significantly associated with the female gender33) but, in our study, gender difference was not found. Only one criterion, ‘visible abdominal distension’, was more frequent in female than in male.
There are some limitations for the results of a questionnaire to be applied to the general population due to unavoidable impairment of scientific accuracy, large variability of subjectively complained symptoms and their tolerance, and different sociocultural or psychological situation for health care seeking behavior34,35). Despite these problems, our study indicates that the Manning criteria is reasonably specific and of diagnostic value. Development of better diagnostic criteria, with improved accuracy by some modification based on further studies, should prevent unnecessary, extensive investigations for the diagnosis of IBS.