Efficacy of Irbesartan on Left Ventricular Mass and Arterial Stiffness in Hypertensive Patients
Article information
Abstract
Background
Increased aortic stiffness measured by pulse wave velocity (PWV) and left ventricular hypertrophy (LVH) are independent risk factors of cardiovascular events in hypertensive patients. We have conducted a prospective study to examine the effects of the angiotensin II receptor antagonist (irbesartan) on PWV and LVH in hypertensive patients.
Methods
A total of 52 untreated hypertensive patients (age:53.3±8.0 yrs) were enrolled; they had no evidence of associated cardiovascular complications. Blood pressure, heart rate, aortic PWV and left ventricular mass index (LVMI) by 2-D echocardiography were measured at baseline and after irbesartan treatment (150 mg or 300 mg/day) at 12 weeks and 24 weeks.
Results
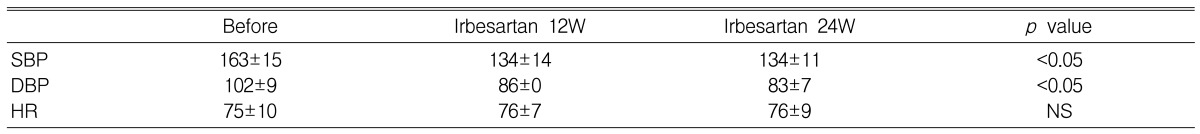
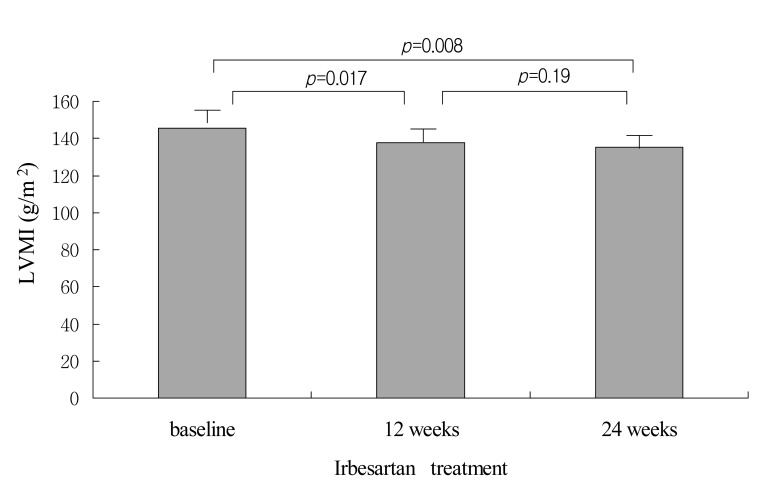
Blood pressure was significantly decreased after 12 weeks and 24 weeks of treatment compared to baseline (SBP: 134.6±13.3 mmHg, 134.0±11.0 mmHg vs 163.7±13.8 mmHg p<0.001, DBP: 86.0±10 mmHg, 83.07 mmHg vs 102.4±9.6 mmHg p<0.001, respectively) without significant change in heart rate. LVMI decreased at 12 weeks and at 24 weeks after treatment compared to baseline (from 145.5±35.1 g/m2 at baseline to 137.5±35.4 g/m2 at 12 weeks, p=0.017 and 135.3±35.4 g/m2 at 24 weeks, p=0.008). Aortic PWV was decreased after irbesartan treatment at 12 weeks (from 9.6±2.8 m/sec to 8.7±3.1 m/sec at 12 weeks, p=0.064) and at 24 weeks (from 9.6±2.9 m/sec to 7.7±2.1 m/sec at 24 weeks, p=0.007).
Conclusions
Long-term treatment with irbesartan may reduce arterial stiffness and regression of LVH in hypertensive patients. The pleiotropic effects of irbesartan, further decreasing PWV without change of BP between 12 and 24 weeks of treatment, may have favorable vascular effects on arterial stiffness and LVH.
INTRODUCTION
Left ventricle hypertrophy increases the risk of cardiovascular disease in hypertensive patients1, 2), and aortic stiffness is also known as a major risk factor for the development of cardiovascular disease3, 4). Aortic stiffness can be measured by a variety of methods; pulse wave velocity (PWV) has been shown to have a significant positive correlation with aortic stiffness. Increased aortic stiffness, measured by PWV, has been reported to be a significant marker for predicting death in patients with cardiovascular disease such as arteriosclerosis and hypertension5). Moreover, aortic PWV is a useful marker for predicting risk of death due to atherosclerosis and hypertension; decreasing PWV has been shown to be more significant than decreasing blood pressure in patients with end stage renal failure6). Although it is well known that hypertensive agents can reduce cardiovascular complications in hypertensive patients, whether a hypertensive agent has an effect on decreasing aortic PWV, in addition to decreasing blood pressure, is a clinically important issue that remains to be addressed. According to recent studies, there are many types of anti hypertensive agents; the vascular effects of each medication are not always the same in hypertensive patients. Angiotensin converting enzyme inhibitors (ACEI), calcium channel blockers and alpha-blocking agents decrease aortic stiffness; however, thiazide-family diuretics have no effect on decreasing aortic stiffness7-10). The use of an angiotensin receptor blockers (ARB), as a hypertensive agents, has been increasing; ARBs have the additional benefit of are reducing aortic stiffness in hypertensive patients10). Irbesartan is a long-acting AT1 receptor antagonist; it has not been studied for its effect on aortic stiffness. Moreover, results from previous studies on the effect of irbesartan on LVH have been controversial; even though other ARBs are known to facilitate regression of LVH. In this study, we evaluated the effects of irbesartan on aortic pulse wave velocity and left ventricular mass in hypertensive patients.
MATERIAL AND METHODS
The study was conducted in the cardiology department at the Korea University Guro Hospital (Seoul, Korea) between March 2001 and July 2002. All patients provided written informed consent. The local ethics committee approved the study.
Study population
A total of 52 patients (age:53.3±8.0 yrs) with untreated essential arterial hypertension (sitting systolic BP of 140~180 mmHg or diastolic BP of 90~115 mmHg) were enrolled; they had no evidence of associated cardiovascular disease. Patients with a low left ventricular ejection fraction, myocardial infarction, angina pectoris, renal failure, atrial fibrillation, diabetic or other cardiovascular disease were excluded.
Treatment protocol
All subjects received: once daily 150 mg/day irbesartan as an initial dose, or once daily 300 mg/day irbesartan or 150 mg/day irbesartan with 12.5 mg/day chlorothiazide in cases of SBP>140 mmHg or DBP>90 mmHg after two weeks of treatment. If the blood pressure was not controlled to below SBP 140 mmHg or DBP 90 mmHg, a dose of once daily 300 mg/day irbesartan with 12.5 mg/day chlorothiazide was administered. Chlorothiazide has been shown to have little effect on pulse wave velocity.
Measurements
Pulse wave velocity (PWV) and the left ventricular mass index (LVMI) were measured using an echocardiogram (HP model 5000). The measurements were repeated three times for each patient: before irbesartan treatment, at 12 weeks, and at 24 weeks after treatment. Echocardiographic data were evaluated by two observers who were blinded to patient information. Smoking was not allowed 24 hours prior to the examination, and height, weight, blood pressure and pulse rate were measured more than three times. The left ventricular ejection fraction was measured with an echocardiogram, and the left ventricular mass was calculated by the formula below after measuring left ventricular internal diastolic diameter (LVIDD), interventricular septal thickness (IVST) and LV posterior wall thickness (PWT) in M-mode.
Left ventricular mass (g)=0.8{1.04[(LVEDD+IVST+PWT)3-LVEDD3]}+0.60
To correct for the influence of body size, LVMI was calculated by dividing body surface area by LVM.
Left ventricular hypertrophy was defined as a LVMI > 134 g/m2 in men and >110 g/m2 in women. From the transmitral flow tracing, early diastolic peak velocity (mitral E waves), late filling with atrial contraction (mitral E waves), and the deceleration time (DT) of the E waves were recorded for the evaluation of LV diastolic function.
PWV was measured using the foot-to-foot method. The measurement of a proximal site was performed at the supra-sternal notch (just distal of left subclavian artery of descending aorta), and a measurement of a distal site was performed at the right femoral artery with a 3.5MHz cardiac probe in the supine position; a sample volume with pulse wave Doppler was obtained from both sites. T1 and T2 represent the time interval for the appearance of a Doppler wave at the proximal site; for the distal site a QRS wave from the ECG was measured by cardiac ultrasonography (Figure 1). The time delay (T: T2 and T1) was measured between the feet for both Doppler waveforms, and the distance (D) was adjusted to the distance measured between the two recording sites. The PWV was calculated as shown below.
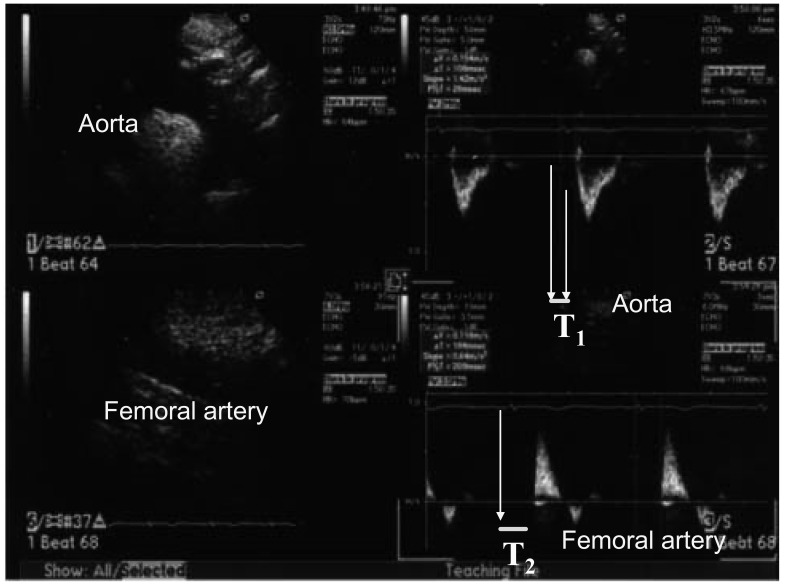
Measurement of pulse wave velocity by the foot-to-foot method. T1 and T2 are the time intervals of the appearance of a Doppler wave just distal to the left subclavian artery of the descending aorta, and at the right femoral artery from the QRS wave of the ECG measured by cardiac ultrasonography.
PWV=D (meters) / T (seconds).
Data were expressed as mean±SD and were analyzed using SPSS (version 10.0). Hemodynamic data, LVMI and PWV were analyzed using a paired sample t-test. The relationships among blood pressure, pulse rate, age, LVMI and PWV were analyzed using a correlation analysis. Statistical significance was accepted as a p value less than 0.05.
RESULTS
A total of 52 patients were examined. [the average age: 53.3±8.0 years, 32 males (57%)] The baseline mean systolic and the diastolic blood pressures were 163±15 mmHg and 102±9 mmHg, respectively. The mean heart rate was 75±10 per minute. After 12 weeks from the index irbesartan treatment, the mean systolic and the diastolic blood pressures decreased to 134±14 mmHg and 86±10 mmHg, respectively (p<0.001); there was no difference in the mean heart rate (76±7/min). A similar trend was also observed after 24 weeks: the SBP (134±11 mmHg), the DBP (83±7 mmHg) and the pulse rate (74±9/min) (Table 1). The Irbesartan treatment dose of subjects were: 150 mg/day irbesartan in 30 cases, 300 mg/day irbesartan in six cases, 150 mg/day irbesartan plus 12.5 mg/day hydrochlorothiazide in seven cases and irbesartan 300 mg plus 12.5 mg/day hydrochlorothiazide in nine cases.
The LVMI was 145.5±35.1 g/m at baseline and 137.5±35.4 g/m2 at 12 weeks (p=0.017), and 135.3±35.4 g/m2 at 24 weeks after the index treatment (p=0.008). LVMI further decreased at 24 weeks compared to 12 weeks of treatment, however this was not significant (Figure 2). The E/A ratio showed an increasing tendency, and DT demonstrated a decreasing tendency after treatment (Table 2); however, these findings were not significant.
Although the aortic pulse wave velocity showed a difference, before and 12 weeks after the treatment it was not significant (9.6±2.8 m/sec before irbesartan treatment and 8.7±3.1 m/sec after 12 weeks, p=0.064); the aortic PWV showed a significant difference in comparisons between baseline and at 24 weeks after onset of treatment (9.6±2.8 m/sec before irbesartan treatment and 7.7±2.1 m/sec after 24 weeks, p=0.007); there was no significant difference in the aortic PWV between 12 and 24 weeks (Figure 3). In addition, age, gender, left ventricular mass and blood pressure did not show significant correlation with aortic pulse wave velocity.
DISCUSSION
We selected only previously untreated hypertensive patients to avoid potential interactions with other antihypertensive agents. There were significant changes after 12 and 24 weeks of irbesartan treatment in both LVMI and PWV.
Thrmann PA et al.11) reported that LVMI estimated by echocardiogram after eight months of treatment significantly decreased from 127±23 to 106±25 g/m2 with valsartan treatment, another angiotensin receptor blocker. The study included only the responders (diastolic BP ≤90 mmHg) to an initial four week treatment with the randomized drug followed by the same randomized treatment for another five months. Our current study showed significant LVH regression with irbesartan treatment after inclusion of all subjects. Left ventricular hypertrophy is associated with a risk for cardiovascular disease; the hypertrophy can be reduced with anti hypertensive agents in hypertensive patients. Angiotensin II receptor blockers have been shown to reduce left ventricular hypertrophy in hypertensive patients. Some participants, in our study, failed to reach optimal blood pressure levels after irbesartan treatment; we did not administer any other medications that could affect LVM and PWV except for chlorothiazide. This study is unique in that the effect of irbesartan could be assessed in a relatively homogeneous group of hypertensive subjects without other factors influencing the results.
Although this study had a small number of patients, we found irbesartan treatment reduced LVMI in the relatively short period of 12 weeks and additional reduction of LVMI was achieved with longer treatment.
Collagen fibers and calcium accumulate in arteries with increasing age; intima thickening and denaturation of the media contribute to arterial stiffness. In addition, arterial stiffness increases in various types of hypertensive patients. The known risk factors of aortic stiffness are: age, blood pressure12), hyperlipidemia13), diabetes14), tarchycardia15) and smoking16). The methods for measuring aortic stiffness include applanation tonometry, MRI and cross-sectional echocardiography. Most studies on the effect of angiotensin II receptor blocker, on arterial stiffness, have been performed using brachial-ankle PWV (baPWV)17, 18). However, baPWV cannot precisely measure the central aortic PWV. In this study, aorto-femoral pulse wave velocity was measured by Doppler ultrasound, which more accurately reflects the PWV of the central artery than baPWV.
In general, aortic stiffness passively decreases when the average blood pressure decreases according to the aortic pressure-volume curve. Atsuhiro et al.19) reported that a decrease in PWV was not observed with a blood pressure less than 140/90 mmHg while a decrease in PWV was noted with a blood pressure less than 135/85 mmHg in hypertensive patients. Azra et al.20) reported that reducing aortic stiffness could be achieved only when losartan was injected; although the same effect with lowering of the blood pressure was obtained from a cross-treatment of losartan with hydrochlorothiazide in hypertensive patients. Therefore, the effect of losartan, in reducing aortic stiffness, does not appear to correlate with the effect of lowering the blood pressure.
These studies illustrate functional factors that influence aortic stiffness as well as a passive decrease in PWV by lowering of the blood pressure. In this study, it was not clear whether the reduced effect on the PWV was due to the secondary effect of the lowered blood pressure or due to the specific effect of irbesartan on aortic stiffness. Even though the changes in blood pressure between 12 weeks and 24 weeks were only minimal, PWV substantially decreased after 12 weeks of treatment. Therefore, Irbesartan has the potential to decrease aortic stiffness in addition to lowering blood pressure.
The mechanisms have not been clearly defined for either angiotensin II receptor blocker function in decreasing aortic stiffness or the lowering of blood pressure. However, the function of the endothelial cell, the change in secretion of NO, and the prevention of collagen synthesis in vessels may contribute to the alteration in aortic stiffness. Animal studies have shown that angiotensin II increased collagen synthesis in arterial smooth muscle cells; blocking type 1 angiotensin II receptor can prevent this collagen synthesis20, 21). Another angiotensin II receptor antagonist, candesartan has been shown to increase secretion of nitric oxide (NO) in hypertensive patients, suppresses contraction against endothelin-1, and improves endothelial dysfunction in patients with coronary artery disease22).
Limitations
This study showed that long-term treatment with irbesartan reduced arterial stiffness and induced regression of LVH in patients with hypertension. It is also true however, that reduction of BP alone reduces LVMI and probably PWV as well. It is not easy to determine how much of the change was due to BP reduction and how much was due to effects that were independent of BP reduction. This study could not rule out an effect of adding thiazide on LVMI reduction, even though thiazide medications are known to have little effect on aortic stiffness. We had the additional limitation of the absence of a control group for comparison. However, it is well known that angiotensin II causes cardiovascular damage resulting in increased morbidity and mortality. Therefore, it was not surprising to find that blocking angiotensin II with irbesartan treatment had beneficial effects in reducing LVMI and PWV.
PWV is a strong independent risk factor for cardiovascular diseases. Improving PWV may be very important for preventing cardiovascular disease in hypertensive patients. In addition to lowering blood pressure, PWV was successfully decreased in patients treated with irbesartan for 24 weeks. In conclusion, these data suggest that long-term treatment with irbesartan may reduce arterial stiffness and regression of LVH in hypertensive patients. The pleiotropic effects of irbesartan further reduce PWV without change of BP between 12 and 24 weeks; this may provide additional favorable vascular effects on arterial stiffness and LVH. Further investigations to identify the mechanism involved in decreasing PWV with irbesartan treatment are warranted.
ACKNOWLEDGMENTS
This work partially supported by a grant of the Seoul R LBD program, Republic of Korea (10528) and Sanofi Aventis, Korea.