Chest Computed Tomography (CT) Immediately after CT-Guided Transthoracic Needle Aspiration Biopsy as a Predictor of Overt Pneumothorax
Article information
Abstract
Background/Aims
This study examined the correlation between pneumothorax detected by immediate post-transthoracic needle aspiration-biopsy (TTNB) chest computed tomography (CT) and overt pneumothorax detected by chest PA, and investigated factors that might influence the correlation.
Methods
Adult patients who had undergone CT-guided TTNB for lung lesions from May 2003 to June 2007 at Seoul National University Bundang Hospital were included. Immediate post-TTNB CT and chest PA follow-up at 4 and 16 hours after CT-guided TTNB were performed in 934 patients.
Results
Pneumothorax detected by immediate chest CT (CT-pneumothorax) was found in 237 (25%) and overt pneumothorax was detected by chest PA follow-up in 92 (38.8%) of the 237 patients. However, overt pneumothorax was found in 18 (2.6%) of the 697 patients without CT-pneumothorax. The width and depth of CT-pneumothorax were predictive risk factors for overt pneumothorax.
Conclusions
CT-pneumothorax is very sensitive for predicting overt pneumothorax, and the width and depth on CT-pneumothorax are reliable risk factors for predicting overt pneumothorax.
INTRODUCTION
Transthoracic needle aspiration-biopsy of the lung (TTNB) is a well-established method for diagnosing lung lesions [1-4]. TTNB is usually performed by an image-guidance method such as fluoroscopy, ultrasonograpy (US), or computed tomography (CT). CT-guided TTNB (CT-TTNB) is an effective and accurate method for the evaluation of small nodules that are not clearly delineated by fluoroscopy and of lesions adjacent to mediastinal vascular structures [1,3,4].
Although TTNB is a generally safe and high-yield technique, with a diagnostic accuracy of 94% and a sensitivity of 95% for diagnosing malignant lesions, pneumothorax is a relatively common and inevitable complication that can develop into a serious condition [5].
The incidence of pneumothorax as a complication of TTNB of pulmonary lesions varies widely, from 8 to 61%. Some of these incidents (10-17%) required chest tube insertion [2,6-8]. Thus, early and accurate detection of pneumothorax after TTNB is clinically important. The occurrence of pneumothorax immediately after TTNB is readily detected with the image-guidance system used for TTNB (fluoroscopy, US, or CT). Most instances of immediate pneumothorax after TTNB are small and localized to the site of the TTNB, and fluoroscopy and US are of less use than is CT. Furthermore, a proportion of pneumothorax was not evident immediately after TTNB and only developed later. Our group previously reported that the incidences of pneumothorax and delayed pneumothorax (pneumothorax after 3 hour) after TTNB by simple chest PA were 21.8% and 3.3%, respectively [9]. In our previous study [9], most TTNBs were performed by fluoroscopic and ultrasonographic guidance. However, Byrd and Roy [10] suggested that CT taken immediately after TTNB was sufficient to predict the occurrence of pneumothorax, and regular follow-up with simple chest PA might therefore be unnecessary. Byrd also recommended that the patient should be instructed to seek medical attention only if symptoms related to pneumothorax occurred.
We agree that chest CT is much more sensitive in detecting pneumothorax than is simple chest PA. However, we think the immediate post-TTNB CT might not correctly predict the occurrence of overt pneumothorax later. Some of the pneumothorax found in the immediate post-TTNB CT resolve spontaneously, but some overt pneumothorax developed subsequently in patients with negative immediate post-TTNB CT.
Thus, we performed a large-scale retrospective study to investigate the correlation between pneumothorax detected by immediate post-TTNB chest CT (CT-pneumothorax) and overt pneumothorax detected by chest PA taken 4 or 16 hours after TTNB and confirmed by at least one pulmonologist and one radiologist. Furthermore, we investigated factors that might influence whether pneumothorax detected on a CT scan (CT pneumothorax) would still appear on a chest X-ray (overt pneumothorax) in particular by measuring the size of the CT pneumothorax.
METHODS
Study design
A retrospective review was performed of the clinical records and radiological findings of 934 patients who underwent CT-guided TTNB for lung lesions at Seoul National University Bundang Hospital between May 2003 and June 2007.
All TTNB were performed by two experienced thoracic radiologists under CT guidance (16-MDCT scanner: MX 8000IDT, Phillips Medical Systems, Best, Netherlands) [11]. Chest CT was taken immediately after TTNB. If pneumothorax was found, its depth and width were measured. Chest PA was also taken at 4 and 16 hours after TTNB to detect overt pneumothorax. Supplementary oxygen, via nasal cannula, was supplied to all patients with CT pneumothorax or overt pneumothorax.
The placement of a chest tube was reserved for patients with signs of respiratory distress or shortness of breath. Cases of second CT-TTNBs for patients with inadequate initial biopsies were excluded.
This study was approved by the Institutional Regulatory Board committee of Seoul National University Bundang Hospital (B-0806/058-104). Informed consent from individual patients was not required because of the retrospective nature of the study.
Data analysis
The proportions of CT pneumothorax and overt pneumothorax were determined. In particular, the correlation between CT- and overt pneumothorax was investigated.
Variables analyzed in relationship to the occurrence of CT pneumothorax and overt pneumothorax included patient age, gender, the size and location of the lesion, presence of an emphysematous change and, in particular, the width and depth of CT-pneumothorax (Fig. 1). Pneumothorax depth was measured in its largest dimension from the pleural surface of lung parenchyma, and its width was measured in the largest dimension of axial tomographic sections.

Measurement of depth and width of post-transthoracic needle aspiration-biopsy computed tomography pneumothorax. The length of pneumothorax was defined as the linear distance of both ends of pneumothorax, and the width of pneumothorax was defined as the maximal perpendicular depth of pneumothorax from chest wall. In the figure, the width is 8.9 cm and the depth is 0.8 cm.
Statistical analysis
The variables found significant by univariable analysis were further analyzed by multivariate analysis using logistic regression with forward selection. The sensitivity, specificity, and accuracy of CT prediction for overt pneumothorax were calculated for all patients with CT pneumothorax based on the clinical and radiologic follow-up, along with review of medical records. The relationship between pneumothorax and quantitative variables was analyzed separately for each variable using Student's t-test. The relationship was also analyzed for multiple dependent variables to investigate possible interactions between variables by means of logistic regression analysis using SAS for Windows (SAS Institute, Cary, NC, USA). The significance of the depth and width of pneumothorax at CT in predicting the rate of overt pneumothorax was further analyzed using the χ2 contingency test. Values of p<0.05 were deemed to be statistically significant.
RESULTS
Incidence of pneumothorax
CT-TTNB was complicated by pneumothorax in 237 cases (25.4%) immediately after TTNB, detected by CT, among the 934 patients. Among the 237 patients with CT pneumothorax, overt pneumothorax was found in 90 patients (38%) on a chest radiograph 4 hour after the procedure. In another chest PA taken 16 hours after CT-TTNB, nine (10%) of the 90 patients with overt pneumothorax at 4 hour and positive CT-pneumothorax showed disappearance of the pneumothorax, but two (1.4%) among the 147 with CT-pneumothorax and no overt pneumothorax at 4 hour showed the appearance of pneumothorax. Of the 237 patients with CT-pneumothorax, 92 (38.8%) showed overt pneumothorax during follow-up.
Of the 697 patients without CT-pneumothorax, 17 (2.4%) showed overt pneumothorax at 4 hour after TTNB, and one more patient among the 680 patient with no CT pneumothorax and no overt pneumothorax at 4 hour exhibited overt pneumothorax at 16 hours after TTNB. A total of 18 patients (2.5%) from the 697 patients without CT-pneumothorax subsequently developed overt pneumothorax.
Of the 92 patients with CT-pneumothorax and overt pneumothorax, 17 (18.4%) required chest tube insertion, and four (22.2%) of the 18 with negative CT-pneumothorax and positive overt pneumothorax required chest tube insertion (Fig. 2).
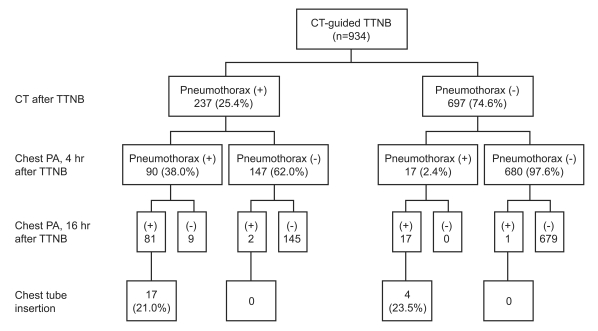
Occurrence of CT-pneumothorax and overt pneumothorax in patients receiving CT-guided transthoracic needle aspiration-biopsy (TTNB). Ninety patients at 4 hr and 2 patients at 16 hr after TTNB, respectively, showed overt pneumothorax during follow-up out of 237 with CT-pneumothorax; however, a total of 18 patients (2.5%) from 697 patients without CT-pneumothorax subsequently developed overt pneumothorax.
Risk factors for CT-pneumothorax and overt pneumothorax
We analyzed the patients showing pneumothorax detected by CT after TTNB (n=237) because CT-pneumothorax had spontaneously regressed at 4 hour after TTNB in a significant proportion of these patients (62.0%). We divided the group into positive overt pneumothorax and negative overt pneumothorax at 4 and 16 hours after TTNB.
Age, gender, lesion size, presence of emphysema, size of CT-pneumothorax (width and depth), pathologic findings, and location of the lung lesion were analyzed. Overt pneumothorax developed in 92 (90 at 4 hour and 2 at 16 hours; 38.8%) of 237 CT-pneumothorax patients, and overt pneumothorax was not detected in 145 (61.2%).
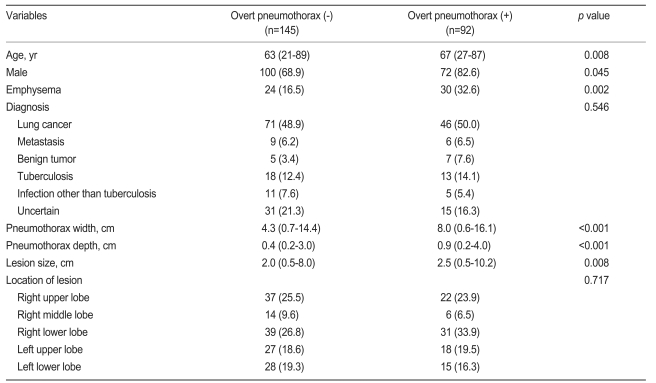
Table 1 shows results of the univariate analysis using Student's t-test. Older age, male gender, underlying emphysema, lesion size, and large CT-pneumothorax (width and depth) were risk factors for overt pneumothorax (Table 1).
However, multivariate analysis revealed that the only pneumothorax width (p=0.001) and depth (p=0.014) were significant risk factors for overt pneumothorax (Table 2). The width of CT-pneumothorax ranged from 0.6 to 16.1 cm (median 8.0 cm in patients with overt pneumothorax and 4.3 cm in patients without overt pneumothorax). The depth of pneumothorax on CT ranged from 0.2 to 4.0 cm (median 0.9 cm in patients with overt pneumothorax, and 0.4 cm in patients without overt pneumothorax).
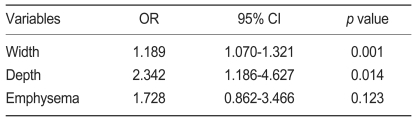
Multivariable analysis of risk factors of overt pneumothorax from post-TTNB pneumothrax detected on a CT scan performed immediately after TTNB
An attempt was made to define cut-off values of width and depth of CT-pneumothorax to predict the occurrence of overt pneumothorax. The sensitivity and specificity for predicting overt pneumothorax were 76.7% and 60.0%, respectively, at a width cut-off value of 5.0 cm in CT-pneumothorax. When the cut-off value was reduced to 3.0 cm, the sensitivity and specificity were 92.2% and 34.0%, respectively. The sensitivity and specificity were 74.5% and 61.2%, respectively, at a depth cut-off value of 0.5 cm. With a depth cut-off value of 0.3 cm, the sensitivity increased to 88.3% and specificity declined to 32.6%. For predicting overt pneumothorax as a complication, sensitivity is much more important (Fig. 3). Other variables, such as patient's age, gender, lesion size, presence of emphysema, pathologic finding, and locations of lung lesion were not associated with an increased risk of overt pneumothorax.

Sensitivity and specificity of width and depth of computed tomography (CT) pneumothorax as risk factors for overt pneumothorax from post-transthoracic needle aspiration-biopsy pneumothrax detected on a CT scan performed immediately after transthoracic needle aspiration-biopsy. Receiver operating characteristic (ROC) curves of width and depth show sensitivities and specificities according to different width and depth cut-off values.
We also analyzed the clinical characteristics of the 18 patients exhibiting overt pneumothorax among the 697 patients without CT-pneumothorax, but no significant difference was found (data not shown).
DISCUSSION
Pneumothorax and hemorrhage after TTNB are widely reported to be inevitable complications [1,3,5,12,13]. The occurrence of pneumothorax is not easy to predict, in contrast to hemorrhage, which usually occurs just after TTNB. Many reports have examined the risk factors and incidence of pneumothorax after TTNB. The most common risk factors for pneumothorax are the number of biopsies, needle size, angle of needle trajectory, lesion depth, lesion size, and underlying emphysema [7,12-16].
Early detection of pneumothorax after TTNB is clinically important. Simple chest X-ray is the usual method to detect pneumothorax. Chest PA taken immediately after TTNB is not suitable for detecting pneumothorax because the development of pneumothorax takes some time to be detected by this method [9,17]. Furthermore, it is not unusual to detect pneumothorax later in patients without overt pneumothorax on initial chest PA taken after 3 hour (delayed pneumothorax) [9,17-19]. Recently, TTNB has come to be performed by means of CT guidance, and it has become a routine clinical procedure to take CT immediately after TTNB to detect pneumothorax. Immediate chest CT is a reasonable practice, because CT is the most accurate method and requires no additional clinical cost or time [18]. Furthermore, large pneumothorax after TTNB can be treated with needle aspiration.
However, several questions remain, including whether all pneumothorax detected by post-TTNB CT develops into pneumothorax detectable by chest PA (overt pneumothorax). How many patients without pneumothorax at immediate post-TTNB chest CT are likely to develop pneumothorax? Are there any factors to predict the occurrence of overt pneumothorax from the condition of CT-pneumothorax?
To answer these questions, we conducted this study, which included a large number of patients (n=934), to improve the clinical and statistical relevance of the results. Even though the review and analysis of data were performed retrospectively, our hospital has a policy of performing CT-TTNB for inpatients only and of taking immediate CT after CT-TTNB and chest PA at 4 and 16 hours (the morning of the following day) after TTNB.
A similar study was reported in 1999 by Bungay et al. [18]. They compared the detection rate of pneumothorax by immediate post-TTNB CT and chest PA at 1 and 4 hour in 88 patients. In total, 37 patients (42%) developed pneumothorax; 35 (39.7%) of these were detected by chest CT and 22 (25%) by chest PA. Pneumothorax by chest PA was found in 20 (57.1%) of 35 patients with pneumothorax by CT and in 2 (3.8%) of 53 without pneumothorax by CT. Byrd's group [19] also reported that pneumothorax was detected by immediate post-TTNB CT in 38 of 158 patients (24.0%), and four (3.3%) of 120 patients with a negative result on immediate post-TTNB CT exhibited overt pneumothorax (delayed pneumothorax).
This study reports that pneumothorax by immediate post-TTNB CT was found in 237 (25.4%) of 934 patients. Overt pneumothorax by chest PA at 4 hour was found in 90 (38%) of 237 with CT-pneumothorax. Chest PA at 16 hours revealed that overt pneumothorax had disappeared at 4 hour in nine (10%) of 90 cases, and two (1.3%) cases of overt pneumothorax were detected at 4 hour among 147 subjects without pneumothorax. In total, 92 patients (38.8%) of 237 with CT-pneumothorax subsequently developed overt pneumothorax, and 145 (61.2%) cases of CT-pneumothorax had spontaneously disappeared.
In contrast, overt pneumothorax at 4 hour chest PA was found in 17 (2.4%) of 697 patients without pneumothorax at post-TTNB CT, and another case of overt pneumothorax was found at 16 hours chest PA. Overt pneumothorax was found in 18 (2.6%) of 697 patients without pneumothorax at post-TTNB CT. Although the incidence of overt pneumothorax among patients without pneumothorax on immediate post-TTNB CT was quite low, it should be recalled that four of the 18 cases (22.2%) subsequently required chest tube insertion.
Immediate post-TTNB CT has become a routine procedure after CT-TTNB, and only some (38.8%; 92/237 in this study) of the CT-pneumothorax then developed overt pneumothorax. Many papers have previously reported risk factors of pneumothorax after TTNB [4,7,9,12,15,20]. We did not investigate the risk factors of CT-pneumothorax, but we did investigate the risk factors for overt pneumothorax from CT-pneumothorax. Male gender, underlying emphysema, lesion size, and the size of the pneumothorax were risk factors, as shown by the univariate analysis. Multivariate analysis revealed that the width and depth of CT-pneumothorax were the only significant risk factors. A width over 3.0 cm and depth over 0.3 cm were optimal cut-off values for predicting overt pneumothorax.
In conclusion, CT-pneumothorax is very sensitive for predicting overt pneumothorax, and 38.8% of CT-pneumothorax developed overt pneumothorax. The width and depth of the CT-pneumothorax were reliable risk factors for overt pneumothorax. The occurrence of overt pneumothorax in negative CT-pneumothorax is infrequent, but not negligible.
Acknowledgements
This work was supported by a second stage Brain Korea 21 project.