Diet and Airway Obstruction: A Cross Sectional Study from the Second Korean National Health and Nutrition Examination Survey
Article information
Abstract
Background/Aims
Several dietary factors, such as antioxidant vitamins, have potential roles in the development of obstructive lung diseases. However, the results of studies on the relationships between dietary factors and obstructive lung diseases are inconsistent. The aim of this study was to determine which nutrients are related to airway obstruction (AO) in the Korean population.
Methods
We used data obtained as part of the Korean National Health and Nutrition Examination Survey (NHANES II) in 2001. Analysis was restricted to 1,005 adults who were 18 years of age and older, who had two or more acceptable spirometry curves, and who had participated in the nutrition examination survey. AO was defined as the ratio of forced expiratory volume in one second (FEV1) to forced vital capacity (FVC) of less than 0.7.
Results
Of the 1,005 study subjects, 78 (7.8%) had AO. Statistically significant factors associated with AO were 55 years of age or older (p = 0.032), central obesity (p = 0.047), hypertension (p < 0.001), smoking of 20 pack-years or more (p < 0.001), low income (p < 0.001), and low dietary protein intake expressed as a ratio of protein to recommended dietary allowance for Koreans (p = 0.037). Multiple logistic regression analyses revealed four factors that were independently associated with AO: smoking of 20 pack-years or more (odds ratio [OR], 5.801; p < 0.001), hypertension (OR, 3.905; p < 0.001), low protein intake (OR, 0.992; p = 0.004), and low income (OR, 1.962; p = 0.018).
Conclusions
In the Korean NHANES, smoking, hypertension, and low income were related to AO. Among dietary factors, only low protein intake was associated with AO.
INTRODUCTION
Dietary factors have been implicated in the cause and prevention of several diseases. Thus, nutritional factors could modify the response to environmental toxins, and a balanced diet might inhibit or reduce the harmful effects of environmental toxins [1]. Similarly, nutritional deficiencies may increase individual susceptibility to adverse environmental exposures, such as allergens, tobacco smoke, infectious agents, and air pollution [2]. Several dietary factors, such as antioxidant vitamins and fatty acids, have potential roles in the development of obstructive lung diseases [3]. However, the results of studies on the relationship between dietary factors and obstructive lung diseases are inconsistent and depend on study design and the populations investigated [4-11].
The aim of the present study was to identify the nutritional factors that are related to airway obstruction (AO). Analyses were based on a large random sample of the general population who participated in the second South Korean National Health and Nutrition Examination Survey (Korean NHANES II) [12].
METHODS
Subjects
We used data from the Korean NHANES II, which has previously been described in detail [12]. Briefly, NHANES II involved a cross-sectional, multistage probability-based sample representing the total non-institutionalized Korean civilian population. Survey subjects were selected from 12,183 households in 2001. Of the 27,859 individuals aged 18 years or older, of 4,816 underwent spirometry, only 3,981 had two or more acceptable curves, and 7,203 underwent a nutritional survey. Complete data for both diet and pulmonary function were available for 1,005.
Nutritional survey and spirometry
The Korean NHANES II consisted of a household questionnaire and a health examination administered by trained examiners. Food intake was estimated based on 24-hour dietary recalls interviews, which were conducted by trained dieticians and nutritionists. Nutrient intakes were calculated using Korean food composition tables [13] and expressed as a percentages of recommended dietary allowance (RDA) for Koreans [14].
Spirometry was performed using equipment that met the American Thoracic Society (ATS) performance criteria, and procedures for testing were based on 1994 ATS recommendations [15].
Definitions
Spirometry results were classified using the Global Initiative for Chronic Obstructive Lung Disease criteria [16]. AO was defined as the ratio of forced expiratory volume in one second (FEV1) to forced vital capacity (FVC) of less than 0.7.
Body mass index (BMI) was calculated from a measurement of weight and standing height (weight in kg / [standing height in m]2). BMI, a measure of adiposity, was categorized as follows; less than 18.5, 18.5 to 24.9, 25.0 to 29.9, and 30.0 or more. These categories corresponded to those proposed by the World Health Organization and represent underweight, normal range, overweight, and obesity, respectively [17].
Subjects' waists were measured using a soft tape midway between the lowest rib and the iliac crest. Hip circumferences were measured at the widest part of the gluteal region, and waist-to-hip ratios were then calculated. Central obesity was defined as a waist-to-hip ratio of > 0.9 for women and > 1.0 for men.
Statistical analysis
Statistical analyses were performed using SPSS version 11.0 (SPSS Inc., Chicago, IL, USA). Descriptive data are expressed as mean ± SD, and frequencies are expressed as numbers (%). Differences between the two groups were tested using the Student's t test or the χ2 test. We conducted univariate logistic regression analyses to examine the association between each variable and AO. Then, multiple logistic regression analyses using the forward stepwise method were performed to identify independent factors associated with AO. Statistical significance was accepted at p values < 0.05.
RESULTS
An analysis of the NHANES II data revealed that 78 (7.8%) of the 1,005 subjects had AO and 927 did not.
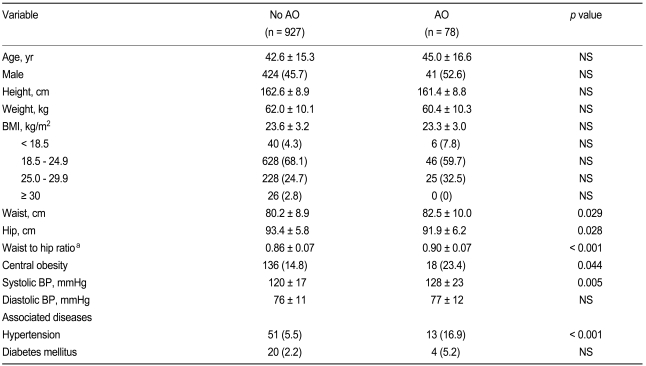
Compared to subjects without AO, those with AO showed significantly higher waist (p = 0.029) and lower hip measurements (p = 0.028) and higher waist-to-hip ratios (p < 0.001). Central obesity was more common in the AO group than in the non-AO group (p = 0.044), but no BMI difference was apparent. Mean systolic blood pressure was significantly higher in subjects with AO than in those without AO (p = 0.005), and hypertension was more common in the AO group (p < 0.001) (Table 1).
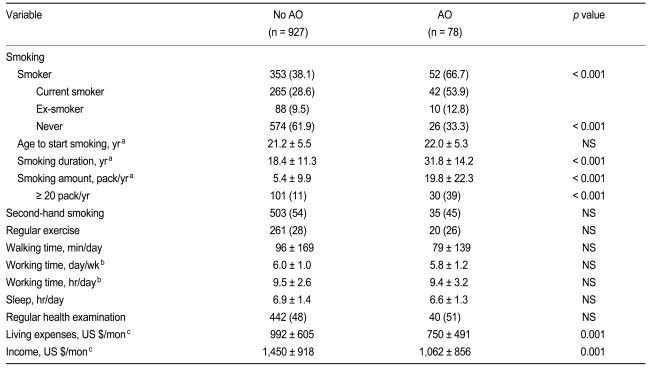
The proportion of smokers was higher in the AO group (p < 0.001), and mean smoking duration was also longer in this group (p < 0.001). Moreover, the AO group had a significantly greater number of pack-years (p < 0.001) and contained more subjects with a smoking history of 20 pack-years or more (p < 0.001). Additionally, mean living expenses (p = 0.001) and income were lower in the AO group (p = 0.001) (Table 2).
The AO group had a significantly lower protein level in their diet than the non-AO group, in terms of both the absolute amount of protein (p = 0.01) and the ratio of protein to recommended daily allowance (RDA) (p = 0.004). Furthermore, the AO group consumed less dietary vitamin B1 (p = 0.022) and B2 than the non-AO group in proportion to the RDA (p = 0.015) (Table 3).
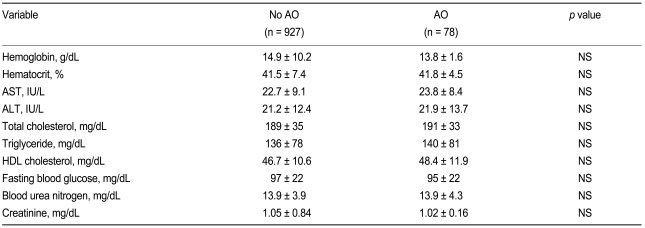
Laboratory results showed no differences between the AO and non-AO groups (Table 4).
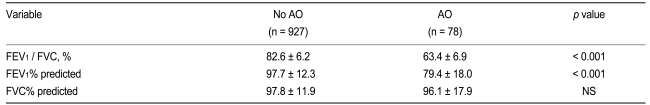
Mean FEV1% FVC (p < 0.001) and FEV1% of the AO group were lower than those of the non-AO group (p < 0.001), whereas FVC% was similar in the two groups (Table 5).
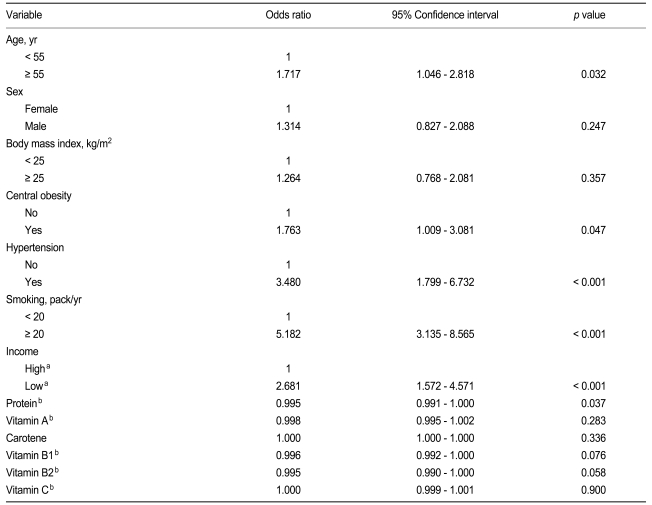
Statistically significant factors associated with AO were aged 55 years or older (odds ratio [OR], 1.717; p = 0.032), central obesity (OR, 1.763; p = 0.047), the presence of hypertension (OR, 3.480; p < 0.001), smoking of 20 pack-years or more (OR, 5.182; p < 0.001), low income (OR, 2.681; p < 0.001), and low dietary protein intake expressed as a ratio of protein to the RDA for Koreans (OR, 0.995; p = 0.037) (Table 6).
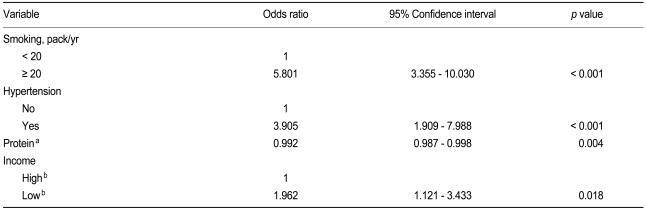
Multiple logistic regression analyses revealed four independent factors associated with AO, including smoking of 20 pack-years or more (OR, 5.801; p < 0.001), hypertension (OR, 3.905; p < 0.001), low protein intake (OR, 0.992; p = 0.004), and low income (OR, 1.962; p = 0.018) (Table 7).
DISCUSSION
This study demonstrated that the presence of hypertension, a lower-protein diet, lower income, and smoking of 20 pack-years or more were associated with an increased risk of AO in adults 18 years or older.
Although the mean dietary intake of each nutrient, except fiber and alcohol, was less in the AO group than in the non-AO group, only dietary protein intake was identified as significantly associated with AO. Multiple logistic regression analyses confirmed the significant association between protein intake and AO, and this relationship was as strong as that between smoking and AO, whereas age and central obesity, which were both significant by univariate analyses, lost significance in the multivariate analysis. Interestingly, protein is not currently the focus of attention as a nutrient related to lung function or diseases, in contrast to antioxidants. However, several animal experiments have shown the importance of dietary protein intake during lung development [18-21]. Studies on rats that were severely calorie restricted for several weeks showed that changes in pulmonary mechanics and lung structure were "emphysema-like" [18]. Moreover, the lungs of protein-deficient rats appeared to be less compliant than those of normal rats [19], and a protein-deficient diet from the neonatal period in a rat model revealed increased surface forces, decreased tissue elastic forces, and augmented resistance of the lung to rupture [20]. Moreover, protein deprivation in isocalorically fed animals had a specific effect on lung scleroprotein content [21], and some observational human studies have demonstrated malnutrition-related emphysema [22,23]. A study conducted in the Warsaw ghetto during World War II revealed that a surprisingly high percentage of people who died of starvation had emphysema (autopsy findings, 50/370 [13.5%]) and that 34 of these 50 were less than 40 years old [22]. Recently, Coxson et al. [23] showed that computerized tomography measurements of emphysema were greater in an anorexic group than in historical controls. Thus, the above data strongly suggest that emphysema-like changes occur in the lungs of subjects who are chronically malnourished.
In contrast to other studies [4-6,8,10,24], we observed no association between the dietary intake of antioxidants and AO. Neither vitamin A and C nor carotene were associated with AO, and no correlation was found between these and FEV1. The main reason for such discrepancies may be differences in study population. Although a Western-style diet is becoming more popular in Korea, the typical Korean diet remains quite different; it contains more fiber and markedly more vegetables. This is why the dietary intake of vitamin C was high in the present study, with a mean ratio of vitamin C to RDA of almost 200% and a median value of 156%. Furthermore, vitamin C deficiency, defined as less than 75% of the RDA, was observed in only 45 of 7,203 subjects participating in our nutrition survey. In our subjects, the dietary intake of vitamin A and carotene was less than that of vitamin C. Some available epidemiologic data suggests that higher intakes of vitamin A and C may prevent smoking-induced AO [24]. However, in the present study, smokers showed no association between the consumption of these vitamins and AO (data not shown). Vitamin E and omega-3 and omega-6 fatty acids were not evaluated in the present study, so we cannot comment on their effects.
In our subjects, the presence of hypertension was identified as an independent factor associated with AO. These associations could derive from shared risk factors, most notably cigarette smoking. In our subjects, a smoking history of 20 pack-years or more was significantly associated with the presence of hypertension (OR, 1.640; p < 0.001). Moreover, smokers with hypertension had a much higher risk for AO than never-smokers without hypertension (OR, 7.578; p < 0.001). Epidemiologic studies evaluating the risk of heart disease have consistently shown an increased risk among patients with chronic obstructive pulmonary disease (COPD) [24,25]. This is true even when the data are "corrected" for smoking. It has long been recognized that reduced lung function is a major risk factor for cardiac death [26]. It has also become clear that cardiac events are the major cause of death in patients with COPD [27,28].
Many studies have reported that low socioeconomic level, as measured by education, income, or some other social class index, is a risk factor for COPD [29,30], and our results support this finding. Socioeconomic variables such as income obviously cannot cause disease directly, but their effect must be mediated through biological mechanisms. These may include smoking, occupational exposures, childhood respiratory illnesses, and others. Socioeconomic status also affects general attitudes toward disease prevention and early care seeking, both of which are difficult to measure in studies such as the present one. Although no positive correlation or significant association was found between income and dietary protein intake, the coexistence of an income below the median value and protein intake in the lower three quartiles significantly increased the risk for AO compared to those with a high income and a protein intake in the highest quartile (OR, 2.681; p < 0.001).
Obesity is a known risk factor for AO [31-33]. The present study also showed a significantly inverse correlation between BMI and FEV1 / FVC or FVC, and waist circumference and waist-to-hip ratio were both inversely correlated with FEV1 / FVC, FEV1, and FVC (data not shown). Moreover, the univariate analysis showed that central obesity, defined by the waist-to-hip ratio, was significantly associated with AO, but that BMI was not. However, the multivariate analysis failed to identify central obesity as an independent predictor of AO.
This study was cross sectional in nature, so we could not establish a temporal relationship between diet and AO. It is unknown whether the onset of AO followed a lower protein intake or whether a higher protein intake prevented the occurrence of AO. Thus, prospective data are needed to establish whether such associations are causal or whether a window of opportunity for being at a major risk for developing AO exists.
In the Korean NHANES, smoking, hypertension, and a low income were risk factors for AO. Among dietary factors, a lower protein intake was associated with AO; thus, a higher protein diet may reduce the prevalence of AO in Koreans.
Acknowledgements
This work was funded by the Korean Academy of Tuberculosis and Respiratory Diseases (KATRD).
The authors thank Heui Sug Jo, M.D. of Kangwon National University for help with the statistical analysis.
Notes
No potential conflict of interest relevant to this article was reported.