Application of Helical Tomotherapy for Two Cases of Advanced Hepatocellular Carcinoma
Article information
Abstract
The role of radiotherapy in the treatment of hepatocellular carcinoma (HCC) has been limited to date, because the liver has a low tolerance to radiation. However, reconstructing tumors and surrounding organs via a three-dimensional conformal planning system can avoid excess radiotherapy exposure to the rest of the liver and adjacent organs. Recently, the concept of "adaptive radiotherapy," such as with helical tomotherapy, has been introduced for treating HCC. Helical tomotherapy obtains an image from the computed tomography component, which allows targeted regions to be visualized prior to, during, and immediately after each treatment and delivers intensity-modulated radiation therapy. We report two patients with advanced HCC who underwent tomotherapy treatment. One was a patient afflicted with advanced HCC and a portal vein tumor thrombus, which was treated with tomotherapy combined with transarterial chemolipiodolization. The other was a patient afflicted with multiple pulmonary metastases treated with tomotherapy followed by systemic chemotherapy.
INTRODUCTION
Hepatocellular carcinoma (HCC) is one of the most difficult malignancies to treat. Several modalities, including surgery, transcatheter arterial chemoembolization (TACE), radiofrequency catheter ablation, percutaneous ethanol injection therapy, radiotherapy, and liver transplantation, have been used and attempted in treating HCC. However, most patients have a poor prognosis because of a poor hepatic functional reserve, associated with cirrhosis, as well as unresectable and aggressive characteristics, such as adjacent vessel invasion and distant metastases.
Portal vein thrombosis due to invasion of the tumor into the portal vein occurs in 20-70% of patients with HCC [1], and has a poor prognosis compared with patients without portal vein thrombosis [2]. Currently, no standard treatment regimen has been established for patients afflicted with HCC combined with portal vein thrombosis. The most frequent site experiencing extrahepatic metastasis from HCC is the lung, and resection may prolong survival in selected cases [3-5]. Nevertheless, surgery is usually limited to patients with pulmonary metastasis or those with metastases at other sites. Few treatment modalities have been suggested for patients with advanced HCC with multiple lung metastases.
Rather than whole-liver radiation therapy (RT), targeted local RT has been attempted by several investigators and has revealed that high doses of radiation can be safely delivered to a portion of the liver [6]. This suggests possible beneficial effects of radiation and chemotherapy for advanced HCC with portal vein tumor thrombosis (PVTT). The most advanced radiation therapeutic techniques are being developed for treating solid tumors. Among them, helical tomotherapy (HT) is an innovative approach for delivering intensity-modulated radiation therapy by combining the elements of helical computed tomography (CT) with megavoltage linear accelerator treatment [7].
Here, we report two cases of advanced HCC treated with HT. One patient was afflicted with PVTT and the other showed multiple lung metastases.
CASE REPORTS
Case 1
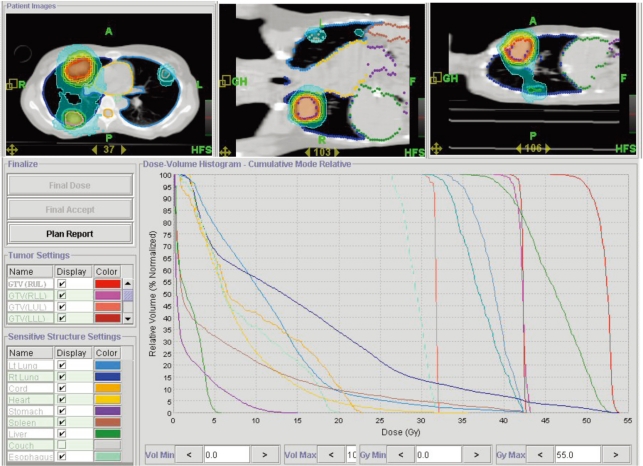
A 43-year-old male was admitted to Seoul St. Mary's Hospital in January 2006. He had been a known hepatitis B carrier for 18 years, and abdominal sonography performed at the outpatient clinic incidentally revealed a mass in the right liver lobe. He had no history of diabetes or hypertension. Pertinent laboratory findings showed the following: a leukocyte count of 8,340/µL, hemoglobin concentration of 14.6 g/dL, platelet count of 251,000/µL, prothrombin activity time of 85%, aspartate aminotransferase of 38 IU/L, alanine aminotransferase of 62 IU/L, alkaline phosphatase of 180 IU/L, total bilirubin of 0.68 mg/dL, total protein concentration of 7.3 g/dL, and an albumin concentration of 3.05 g/dL. Serological tests performed on the patient to test for the hepatitis B "s" and "e" antigens were positive. Furthermore, the serum alpha-fetoprotein (AFP) concentration was 8.04 ng/mL. CT revealed a diffuse infiltrative HCC involving the right hepatic lobe with tumor thrombosis involving the right portal vein and the proximal portion of the left portal vein (Fig. 1A and 1B). HT treatment was targeted at the site of the portal vein thrombosis. The patient was immobilized with a whole-body vacuum, low-pressure foil (Body Fix System, Medical Intelligence, Schwabmuenchen, Germany) to minimize respiratory motion of the tumor and internal organs. A daily dose of 5 Gy was administered, at five fractions per week, to deliver a total dose of 50 Gy (Fig. 2). We performed CT scans at 2 (Fig. 1C and 1D) and 6 months (Fig. 1E and 1F) after treatment, which showed markedly improved portal vein thrombosis. After HT treatment, an intra-arterial chemoport was inserted at the hepatic artery 1 month later, and the patient received four cycles of chemotherapy with a monthly regimen of cisplatin (60 mg/m2), epirubicin (50 mg/m2), and 5-fluorouracil (200 mg/m2). One year after receiving HT, a 2-cm arterial enhancing nodule was discovered on the hepatic dome of the liver. The patient subsequently received successful radiofrequency ablation (RFA) for the enhancing nodule. He is currently alive and has been in good health for 23 months with subsequent successful treatments after the HCC diagnosis.

Abdominal computed tomography (CT) scan reveals a diffuse infiltrative hepatocellular carcinoma involving the right hepatic lobe (A) with a portal vein thrombosis (B). Abdominal CT 2 months after transcatheter arterial chemoembolization and tomotherapy showed improvement in the right infiltrative mass (C) and portal vein thrombosis (D). Abdominal CT 6 months after the initial treatment showed partial resolution of the right infiltrative mass (E) and a portal vein thrombosis (F).
Case 2
A 42-year-old female patient with HCC visited Seoul St. Mary's Hospital in January 2006. She was diagnosed with HCC in 2001 and had received a right hepatectomy at another hospital. Three years after the surgery (August 2004), she visited our hospital, and a lung metastasis was discovered. She received six intermittent cycles of chemotherapy from 2004 to 2005. After the six cycles of chemotherapy, she refused to visit the hospital. The laboratory findings upon admission showed the following: a leukocyte count of 2,500/µL, hemoglobin concentration of 11.5 g/dL, platelet count of 50,000/µL, prothrombin time activity of 78%, aspartate aminotransferase of 36 IU/L, alanine aminotransferase of 31 IU/L, alkaline phosphatase of 94 IU/L, total bilirubin of 0.65 mg/dL, total protein of 6.8 g/dL, and an albumin concentration of 3.86 g/dL. Additionally, serum AFP was 926.3 ng/mL. We performed chest X-rays upon admission, which showed an increase in the size of the metastatic lung lesions compared with her previous chest X-rays from 11 months earlier (Fig. 3A). The chest CT also showed an increase in the size of multiple metastatic lung lesions, but no increase in number (Fig. 3D). A CT of the abdomen also revealed an interval increase in the size of the HCC in the hepatic dome, compared with the abdominal CT from 1 year earlier. The patient received HT for her multiple lung lesions, with a daily regimen of 3-5 Gy, at five fractions per week, for a total dose of 30-50 Gy to each metastatic lung lesion (Fig. 4). A chest X-ray was performed at 2 and 6 months after the HT and revealed a marked decrease in the size of the multiple lung nodules (Fig. 3B and 3C). A chest CT similarly showed a vast decrease in the size of the lung nodules (Fig. 3E and 3F). Serum AFP 2 months after HT was 224.1 ng/mL. The patient received systemic chemotherapy treatment on a monthly regimen. Six months after receiving HT, a brain CT showed newly developed brain metastases. She received HT again for her multiple brain lesions, according to the same treatment protocol for her metastatic lung lesions (data not shown). A brain CT was performed at 3 months after the HT and revealed a marked decrease in the size of the multiple brain masses. She was alive 16 months after the initial HT for multiple metastatic lung tumors and died 6 months after receiving brain HT due to bleeding from a newly developed metastatic brain tumor.
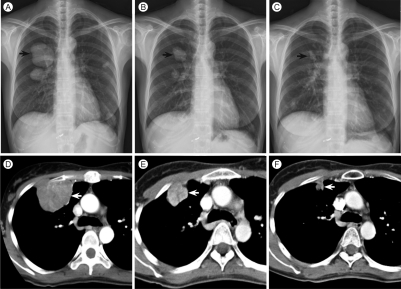
Chest X-rays show multiple metastatic lung lesions (A). Chest X-ray 2 months (B) and 6 months (C) after tomotherapy showed a marked decrease in the size of the multiple lung nodules. Chest computed tomography (CT) on admission showed multiple metastatic lung lesions with the largest lesion measuring 5.5 cm in diameter (D). Chest CT 2 months later shows a marked decrease in the size of the lung nodules, from 5.5 to 1.3 cm (E). Chest CT 6 months later shows a further decrease in the size of the lung nodules (F).
DISCUSSION
Until recently, the role of radiotherapy in advanced HCC had been limited due to the poor tolerance of the entire liver to radiation [8]. Recently, local RT has been investigated for treating HCC. In particular, recent advances in three-dimensional conformal radiotherapy have allowed us to minimize unwanted irradiation to normal liver tissue, and, therefore, facilitate maximal escalation of the radiation dose to the critical organs without a significant increase in toxicity [6]. HT uses intensity-modulated radiation fan beams to deliver a highly conformal dose distribution to the patient [7].
Portal vein thrombosis and lung metastases are common in patients with advanced HCC [4]. Both complications are associated with a poor prognosis; however, no standard treatment regimen has been established. Although TACE shows statistically significant survival benefits in patients with unresectable HCC [9], controversy remains over the benefit for patients with portal vein thrombosis. TACE has generally been contraindicated for these patients because of potential ischemic liver damage [10]. However, several studies have been conducted in which TACE was successfully performed in patients with good hepatic reserve or collateral circulation around the main portal vein [6].
The lungs are the most common site of extrahepatic spread of HCC [3], and pulmonary resection for metastasis prolongs survival in selected cases [3,4]. Furthermore, some authors have reported using curative resection to prolong survival, even in patients with multiple lung metastases [5]. However, in clinical practice, surgery is usually restricted to patients with a good pulmonary reserve and a solitary metastasis. Thus, few patients are suitable for this surgery.
Here, we describe two cases of advanced HCC treated with HT and combined chemotherapy. One patient had a portal vein thrombosis, which resolved after HT and additional hepatic artery infusion chemotherapy, whereas the other patient exhibited a vast decrease in the size of multiple lung nodules treated with HT and systemic chemotherapy. One year after receiving HT, the first patient developed a new arterial enhancing mass in the hepatic dome and received RFA for the hepatic mass. Six months after the RFA, the patient currently shows no sign of tumor recurrence. No significant adverse effect of HT occurred during the 23-month follow-up period. The second patient died 16 months after receiving HT. Imaging studies performed 6 months after HT revealed brain metastases. The patient survived 16 months after receiving lung HT, and no significant adverse effect developed. HT combined with chemotherapy achieved a good response and longer survival in these two cases of advanced HCC with a portal vein tumor thrombosis and a lung metastasis.
Recently, many precise radiation techniques have been developed to treat solid tumors [11]. Our cases suggest that PVTT and pulmonary metastasis are amenable to highly targeted irradiation associated with minimal irradiation to surrounding normal tissue. The results demonstrate that appropriate combinations of radiation techniques with intra-arterial and systemic chemotherapy may significantly improve a patient's quality of life by improving the treatment response and minimizing the potential for late radiation effects in surrounding structures.
Neither patient showed signs of recurrence or adverse effects during a 16 month follow-up period. In conclusion, HT may be beneficial for select patients with advanced HCC.
Notes
No potential conflict of interest relevant to this article was reported.