Strangulated Small Bowel Obstruction Following Endoscopic Retrograde Cholangiopancreatography
Article information
To the Editor,
The most common cause of mechanical small bowel obstruction is adhesions related to prior abdominal surgery. Cases of mechanical small bowel obstruction following endoscopy have been rarely reported and most of these cases were related to prior colonoscopy [1]. The following is the first report of intestinal obstruction following endoscopic retrograde cholangiopancreatography (ERCP).
An 81-year-old female was admitted for evaluation following an abnormal liver function test and abdominal ultrasound findings of a dilated common bile duct 12 mm in diameter. The patient had been healthy with a prior history of a total hysterectomy for a large uterine myoma 20 years ago. Her vital signs were stable upon admission with blood pressure (BP), 110/67 mmHg; pulse rate, 90 beats/min (bpm); respiratory rate, 18/min; and body temperature, 36.5℃. A physical examination revealed normoactive bowel sounds and no abdominal tenderness or palpable mass. Chest and abdominal X-rays were normal. Laboratory tests indicated increased alkaline phosphate (175 IU/L) and gamma-glutamyl transferase (237 IU/L). On the second day of admission, an ERCP was performed. Cholangiography revealed no specific lesions, apart from a dilated extrahepatic duct. The day after the procedure, on the third day of admission, serum amylase and serum lipase were elevated to 3,491 U/L and 5,887 U/L, respectively, and the patient was managed by restricting oral intake and intravenous hydration. Three days after the procedure, a physical examination and simple abdominal X-ray revealed no abnormalities and serum amylase and lipase levels returned to normal (36 U/L and 20 U/L, respectively). The patient was then started on a liquid oral diet. Two hours after eating, approximately 72 hours after the procedure, the patient complained of sudden-onset, severe, non-radiating abdominal pain. Physical examination revealed abdominal distension and periumbilical tenderness with decreased bowel sounds and paralytic ileus was suspected. Four days after the procedure, the patient's vital signs deteriorated with BP, 81/57 mmHg; pulse rate, 102 bpm; respiratory rate, 26/min; and body temperature, 36.8℃. An abdominal examination revealed board-like rigidity and abdominal X-rays indicated small bowel dilation with a dilated loop (Fig. 1). Emergent abdominal computed tomography (CT) showed diffuse distension of the small bowel loops with gas and fluid, reduced enhancement in the long segment of the ileum (Fig. 2), and swelling of the pancreas. Strangulated mechanical small bowel obstruction was considered to be a likely diagnosis. The patient went to the operating room for an emergency laparotomy. Upon opening the abdomen, a peritoneal fibrotic band was observed between the right pelvic wall and rectosigmoid colon, creating a 2 cm diameter opening with a loop of small bowel confined into the space. Approximately 1.2 m of the ileum was necrotic and nonviable; therefore, the involved tissue was resected, followed by primary anastomosis. Hemorrhagic necrosis of the ileum was noted on the pathology report (Fig. 3). The patient recovered uneventfully and was discharged 10 days postoperatively.

Plain abdominal X-ray 4 days after the endoscopic retrograde cholangiopancreatography procedure revealed small bowel dilation with a dilated loop.

Abdominal computer tomography 4 days after the endoscopic retrograde cholangiopancreatography procedure shows pneumatosis intestinalis and decreased enhancement of the ileum wall.
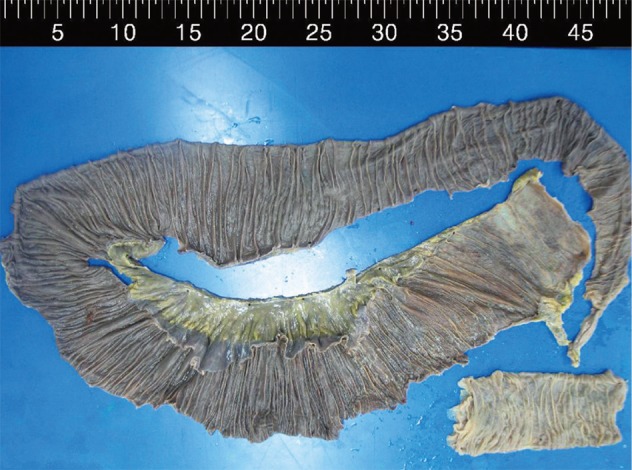
Surgical specimen of the small bowel with hemorrhagic necrosis observed through the entire resected region.
The median interval between an initial obstetric operation and small-bowel obstruction is 5.3 years [2]. Therefore, the risk of spontaneous adhesive small bowel obstruction was low in this case since the patient had not developed a small bowel obstruction 20 years after hysterectomy. Reports of small bowel obstructions following colonoscopy note that each of the cases occurred in patients who had previously had surgery, thus suggesting that adhesive small bowel obstruction was initiated by colonoscopy [3]. Additionally, the interval between initial endoscopy and mechanical small bowel obstruction following endoscopy was between 1 to 3 days [1]. In this case, we propose that ERCP initiated a mechanical intestinal obstruction 72 hours after the procedure.
A review of the literature failed to identify any reports of strangulated small bowel obstruction after ERCP. Only a small number of case reports have described mechanical small bowel obstruction following colonoscopy and only one case of small bowel pseudo-obstruction after esophagogastroscopy has been reported [1,4]. Several mechanisms have been proposed as contributing factors to intestinal obstruction following endoscopy, including increased sympathetic tone due to high pressure in the bowel. This is caused by inf lation of the intestine and encapsulation of the small bowel by adhesion with air insufflations through an incompetent ileocecal valve [1]. We suggest two additional mechanisms. First, we hypothesize that the small bowel was forcefully encapsulated into the opening by high pressure during the ERCP procedure. Second, we hypothesize that decreased motility of the small bowel was related to mild acute pancreatitis [5] that aggravated bowel strangulation. This is supported by results from the emergent CT showing swelling of the pancreas on the fourth day after ERCP with normal amylase and lipase levels.
Mechanical small bowel obstruction following endoscopy is rare, but can be a significant complication. Physicians should consider it as a possible diagnosis when a patient has a history of previous abdominal surgery, small bowel obstruction, or acute abdominal pain following endoscopic procedures.
Notes
No potential conflict of interest relevant to this article is reported.