Tissue Doppler-derived E/e' ratio as a parameter for assessing diastolic heart failure and as a predictor of mortality in patients with chronic kidney disease
Article information
Abstract
Background/Aims
Diastolic dysfunction occurs frequently in patients with chronic kidney disease (CKD) and is associated with heart failure (HF) or mortality. We investigated whether the ratio of early diastolic mitral inflow velocity to early diastolic mitral annulus velocity (E/e' ratio), estimated using tissue Doppler imaging, has prognostic value for cardiovascular morbidity and all-cause mortality in patients with CKD.
Methods
For 186 patients with CKD of stages III to V, we obtained echocardiograms with tissue Doppler imaging. A 5-year follow-up of 136 patients was performed based on hospital records and telephone interviews. The enrolled patients (79 males and 57 females) were categorized into the following CKD subgroups: stage III (n = 25); stage IV (n = 22); and stage V (n = 89).
Results
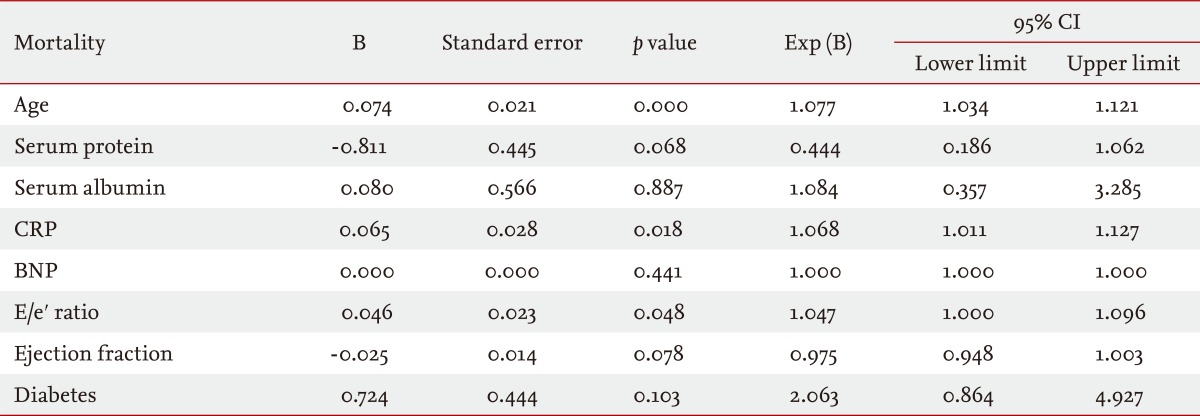
The average follow-up period was 30.45 months and the mean age of the patients was 61.13 years. The mortality rate after 5 years was 60.0%. The causes of death were: sepsis, 21.9%; HF, 16.2%; and sudden death, 15.2%. Age (p = 0.000), increased C-reactive protein level (p = 0.018), and increased E/e' ratio (p = 0.048) were found to correlate with mortality. Age (p = 0.000), decreased ejection fraction (p = 0.003), and increased E/e' ratio (p = 0.045) correlated with cardiovascular event.
Conclusions
The E/e' ratio can predict mortality and cardiovascular events in patients with CKD who have diastolic dysfunction.
INTRODUCTION
Patients with chronic kidney disease (CKD) associated with cardiovascular disease (CVD) have a higher risk of death than the general population [1]. Heart failure (HF) associated with CKD increases the risk of death, and these patients have a poor prognosis [1,2]. Therefore, in patients with CKD, HF needs to be diagnosed and treated early [3,4]. In general, the level of B-type natriuretic peptide (BNP), which reflects an increase in the volume of the left ventricle, is elevated in patients with CKD or end-stage renal disease (ESRD), often in the presence of normal cardiac function [1]. This means that BNP cannot be used as an accurate marker for the diagnosis of HF in patients in whom the left ventricular (LV) ejection fraction (EF) is preserved. Presently, the ratio of early diastolic mitral inflow velocity to early diastolic mitral annulus velocity (E/e' ratio) is used for the evaluation of LV filling pressure, and it has been used as a marker to diagnose diastolic HF [5,6]. In hypertensive patients with elevated E/e' ratio the annual mortality rate is 10% and the ratio is considered to be a prognostic factor for the development of CVD [3]. However, with respect to the different degrees of CKD associated with HF, studies on the usefulness of the tissue Doppler E/e' ratio as a predictive factor for the development of CVD and mortality have not been conducted. In the present study, we investigated whether the E/e' ratio, which is a marker for the diagnosis of diastolic HF in CKD patients, could predict the incidence of CVD and mortality.
METHODS
Subjects
The 186 patients admitted for dyspnea to the Department of Nephrology, Yonsei University Wonju College of Medicine between March 2003 and February 2006 underwent basic blood and urine tests, BNP, chest X-ray, electrocardiography, and echocardiography. Fifty patients with normal LV EF in the electrocardiograph and dyspnea due to other causes were excluded, and 136 patients underwent follow-up for 5 years. Correlations of the results of the clinical tests and echocardiography during the follow-up period to the incidence of CVD and mortality were examined.
Methods
Echocardiography
Two-dimensional echocardiography was performed according to the recommendations of the American Society of Echocardiography. EF was measured using the two-dimensional M-mode method, and the left arterial volume was measured using the cylinder method with two orthogonal apical views. A patient with EF > 50% was assigned to the 'normal' group, while a patient with EF < 50% was assigned to the 'reduced' group. To record the trans-mitral blood flow at the apical four-chamber view, pulsed-wave Doppler was used. The rate of the E, the rate of the late diastolic blood flow (mitral peak velocity of late filling, A), the ratio of E/A, and the deceleration time (DT) of the E wave were measured. In the septum and the lateral annulus, e' was measured by tissue Doppler, and the E/e' ratio was calculated.
Definition of clinical courses
CVD includes acute myocardial infarction, coronary artery disease, angina pectoris, and congestive HF. The glomerular filtration rate (GFR) was calculated using the Modification of Diet in Renal Disease equations. Renal dysfunction that was more extensive than the moderate level was defined when the creatinine clearance rate was < 60 mL/min, and the severity of renal dysfunction was classified according to the level of renal failure. Patients who had creatinine clearance rates in the range of 30 to 60 mL/min were defined as stage 3, those with 15 to 30 mL/min were stage 4, and those with rates lower < 15 mL/min were defined as stage 5 ESRD [7].
Systolic HF was defined according to the Framingham criteria according to disease history; echocardiography findings; radiologic findings; clinical biochemical test findings; EF < 50% in echocardiography; and left ventricle size during the late diastolic phase of > 5.5 cm. Diastolic HF was defined when at least three categories of the clinical conditions used in the perindopril in elderly people with chronic HF (PEP-CHF) trial were satisfied (i.e., exertional dyspnea, orthopnea, pretibial pitting edema, clinical pulmonary congestion, improvement of dyspnea after the administration of diuretics, accentuation of jugular vein waves, cardiomegaly, past history of myocardial infarction, and radiologic pulmonary congestion). The objective test standards were those cases with two findings in echocardiography from the following list: EF > 50%; dysfunction of the left ventricle in the diastolic phase (i.e., enlargement of the left ventricle); Doppler finding of abnormal LV inflow; and E/e' ratio > 10 [7].
Statistical analyses
Through application of the Student's t test and chi-square test, blood tests, and echocardiography indexes were compared and the cut-off values of the E/e' ratio were divided into groups, and the survival rate was analyzed by the Kaplan-Meier method. Cox regression was used to assess the association of mortality with the E/e' ratio, as well as the association of cardiovascular events with the E/e' ratio. For the determinations of optimal sensitivity and specificity, the results were analyzed using receiver operating characteristic (ROC) curves. The SPSS version 17.0 software (SPSS Inc., Chicago, IL, USA) was used, and statistical significance was adjudged for a p value < 0.05.
RESULTS
Demographics and laboratory results of the study group
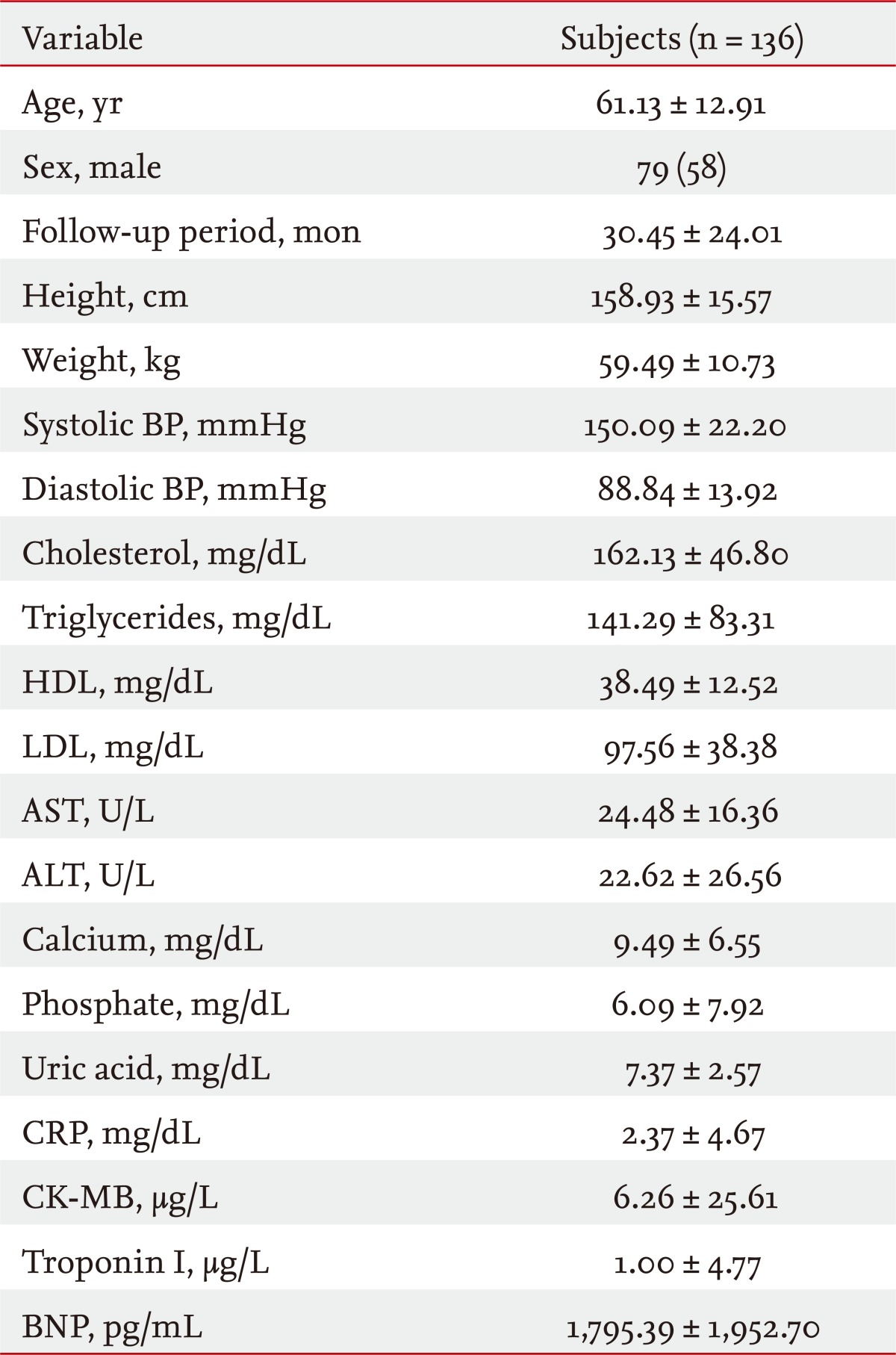
The mean age of the 136 subjects was 61.13 ± 12.91 years, there were 79 male patients (58.0%), and 53 of the patients (38.9%) had systolic HF. With regard to the stage of chronic renal failure, 25 patients were stage 3, 22 patients were stage 4, and 89 patients were stage 5. In the renal failure stage 5 group, 22 patients underwent renal replacement therapy, 19 patients underwent peritoneal dialysis, and 48 patients received hemodialysis. For the patients in the study, the follow-up observation period was 30.45 ± 24.01 months, systolic blood pressure was 150.09 ± 22.20 mmHg, and diastolic blood pressure was 88.84 ± 13.92 mmHg. For the laboratory results, with respect to those categories that showed abnormality, the hemoglobin level was 9.95 ± 1.75 g/dL (normal range, 13.5 to 17.0), the total protein level was 6.39 ± 0.91 g/dL (6.4 to 8.3), the albumin level was 3.43 ± 0.63 g/dL (3.3 to 6.1), and reduced results were shown. The mean C-reactive protein (CRP) level was 2.37 ± 4.67 mg/dL (normal value, < 0.5), the level of phosphate was 6.09 ± 7.92 mg/dL (normal range, 2.3 to 4.5), and increased results were shown. Concerning the results of tests pertinent to the cardiovascular system, the creatine kinase-myocardial band fraction level was 6.26 ± 25.61 µg/L (normal value, < 5.0), the troponin I level was 1.00 ± 4.77 µg/L (normal value, < 0.78), the BNP level was 1,795.39 ± 1,952.70 pg/mL (normal value, < 100), and increased results were shown. The mean glomerular infiltration rate was 13.16 ± 12.26 mL/min (Table 1).
Echocardiographic results for the study group
In echocardiography, the LV mass was 294.14 ± 84.90, the end-systolic LV diameter was 3.92 ± 0.97 cm (normal range, 2.3 to 3.5), the end-diastolic LV diameter was 5.60 ± 0.77 cm (normal range, 3.8 to 5.5), the end-diastolic interventricular septum thickness was 1.14 ± 0.25 cm (normal range, 0.6 to 1.1), and the end-diastolic posterior wall thickness was 1.13 ± 0.24 cm (normal range, 0.6 to 1.1). The left atrium size was 4.84 ± 0.64 cm (normal range, 3.0 to 4.5), the E was 0.88 ± 0.33 m/sec, the e' was 0.06 ± 0.03 m/sec, and the E/e' ratio was 14.66 ± 6.91. The A was 0.97 ± 0.30 m/sec, the E/A ratio was 1.00 ± 0.66, and the DT was 196.75 ± 62.41 msec (Table 2).
Mortality rate and cause of death in the study group
During the follow-up observation period, 63 patients (46.3%) died and 42 patients (30.8%) were confirmed to be alive. The most common cause of death was sepsis (n = 23, 16.91%), followed by congestive HF (n = 17, 12.5%) and sudden death (n = 16, 11.7%) (Fig. 1).
Linear regression analysis of the E/e' ratio with the GFR, LV EF, and BNP of the study group
As the E/e' ratio increased, the LV EF (p = 0.327) and GFR (p = 0.106) decreased, and the BNP showed a tendency to increase (p = 0.051). However, statistical significance was not demonstrated.
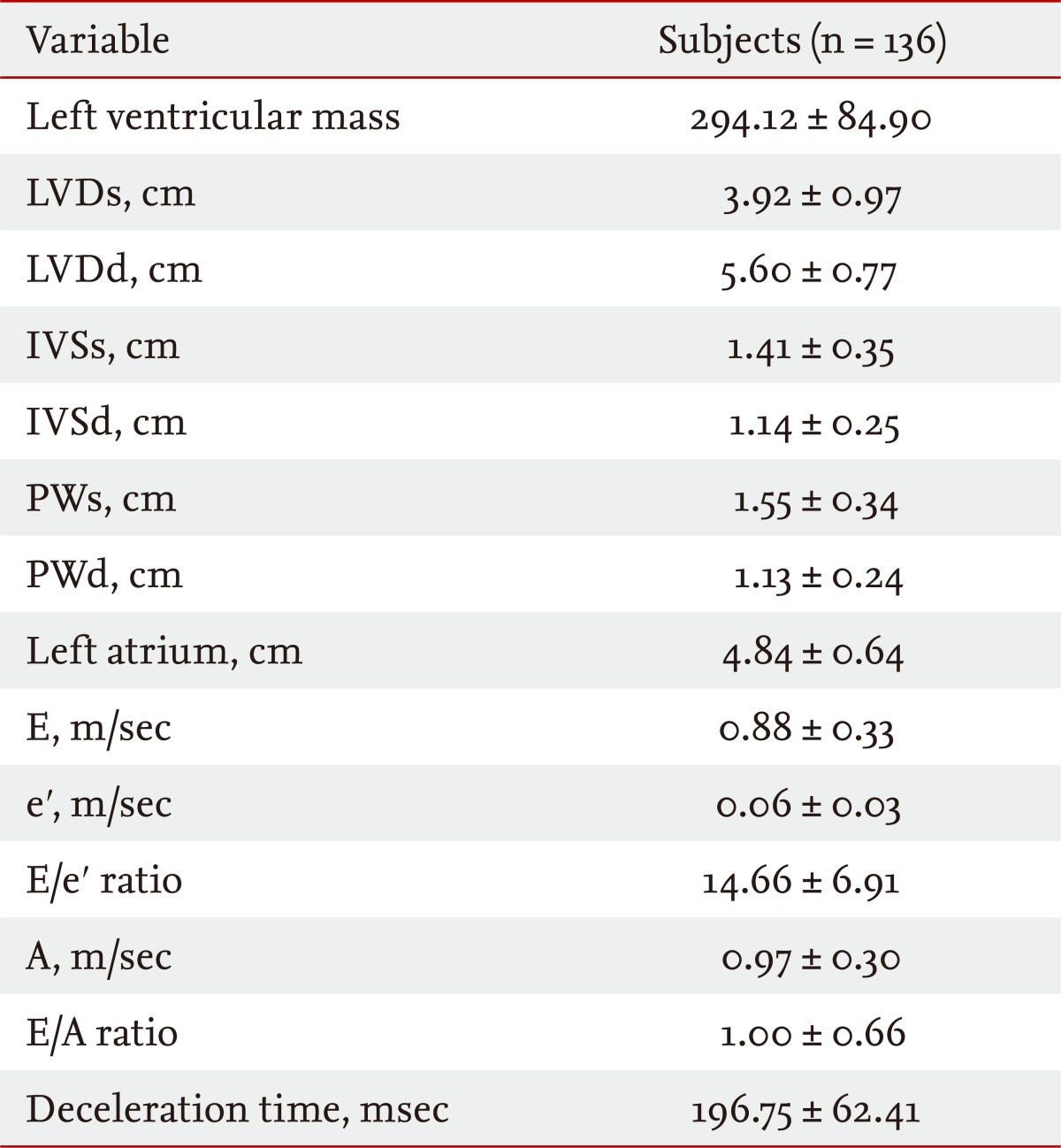
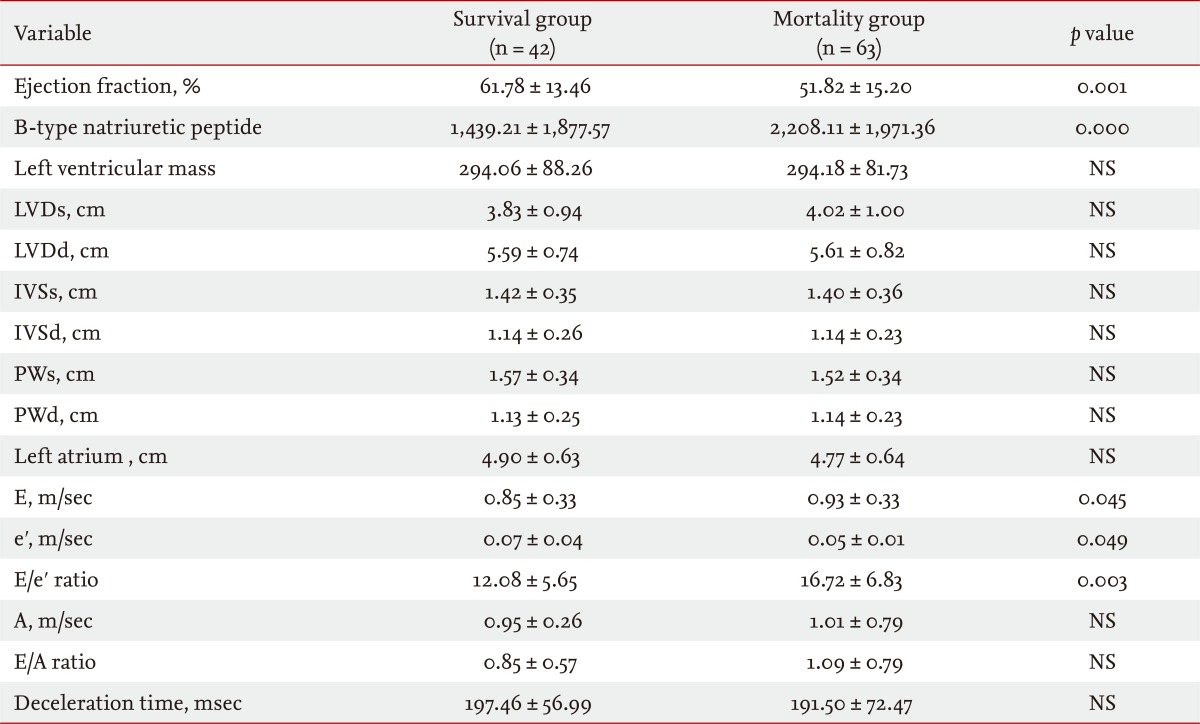
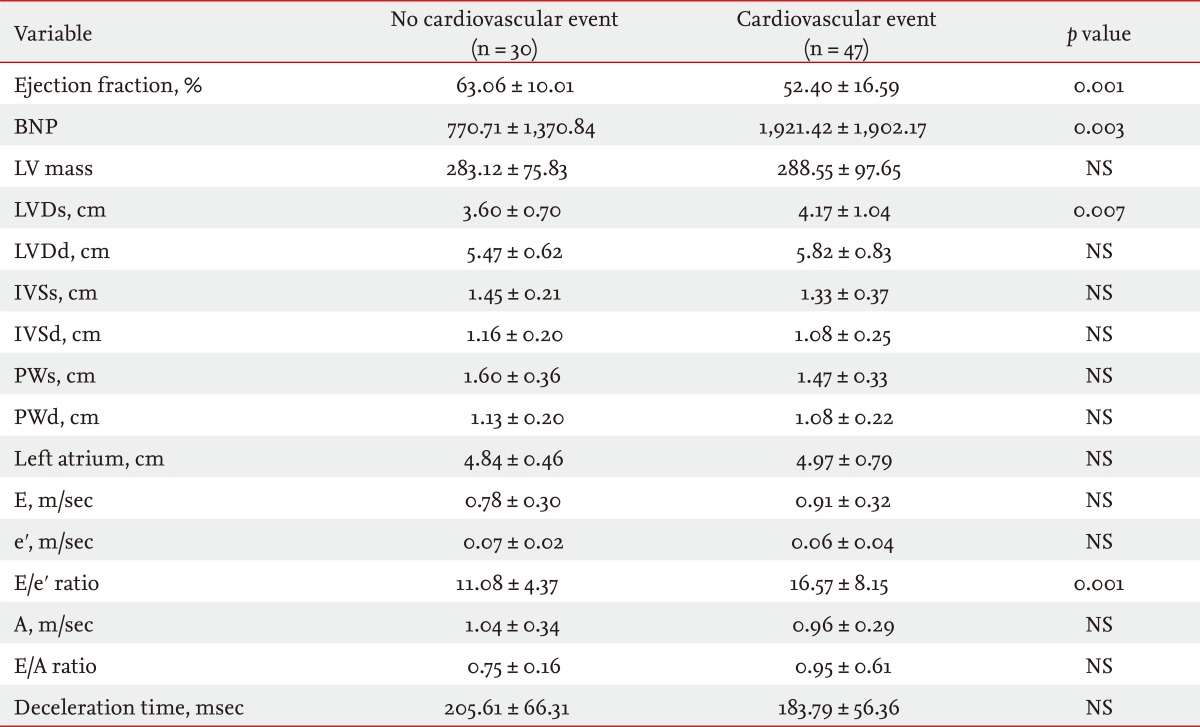
Comparison of the index pertinent to the heart between the survivors and deceased, and between the CVD group and the normal group
In comparison with the survival group, the deceased group showed decreased LV EF (p = 0.001), increased BNP (p = 0.000), and increased E/e' ratio (p = 0.003) (Table 3). In comparison with the group that did not develop CVD, the group that developed CVD showed reduced LV EF (p = 0.001), and increases in BNP (p = 0.003), LVD (p = 0.007), and E/e' ratio (p = 0.001) (Table 4).
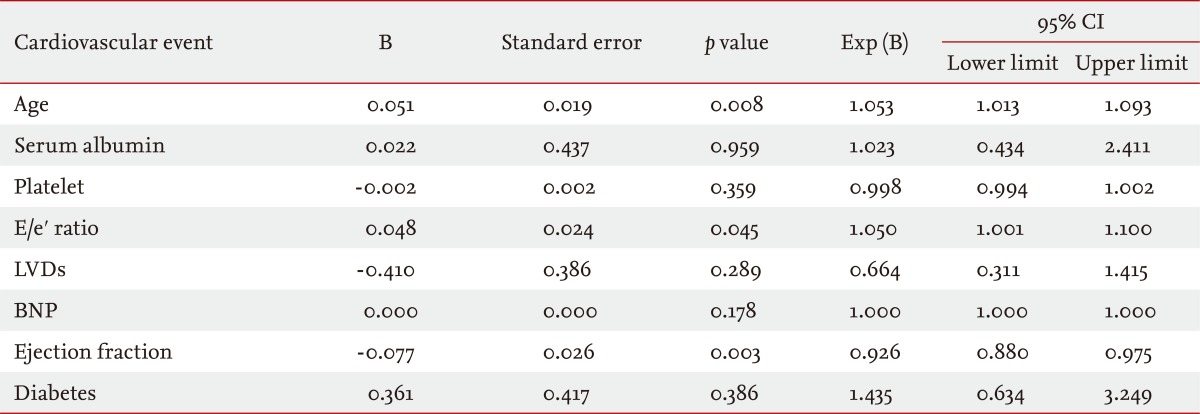
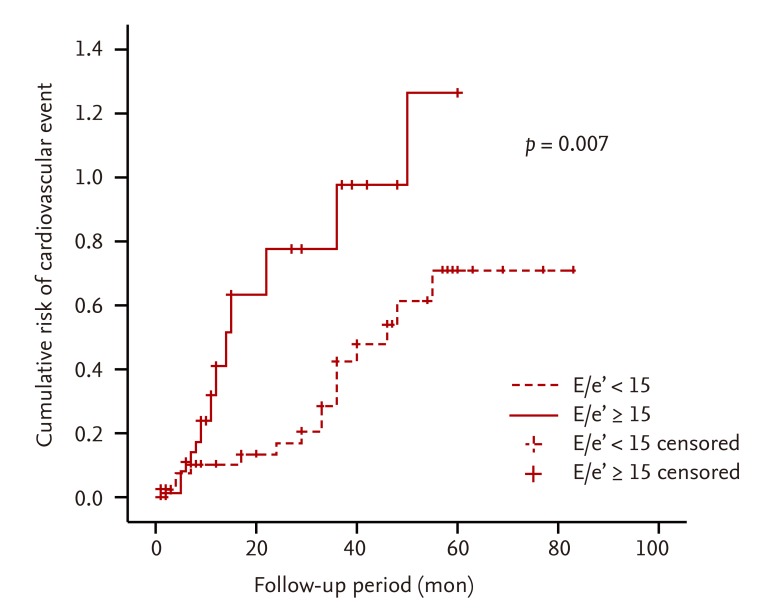
Kaplan-Meier survival curve according to the E/e' ratio
In the Kaplan-Meier analysis, when the E/e' ratio was > 15, the survival rate of patients (p = 0.037) (Fig. 2), CVD (p = 0.007) (Fig. 3), and death due to CVDs (p = 0.005) (Fig. 4).

Kaplan-Meier curves for patient survival. In the Kaplan-Meier analysis, the survival rate for patients in the E/e' ratio group > 15 is lower than that for patients in the E/e' ratio group < 15 (p = 0.037). E, early diastolic mitral inflow velocity; e', early diastolic mitral annulus velocity.
Kaplan-Meier curves for cumulative cardiovascular events. In the Kaplan-Meier analysis, the cumulative risk of cardiovascular events is higher in the group with E/e' ratio > 15 than in the group with E/e' ratio < 15 (p = 0.007). E, early diastolic mitral inflow velocity; E', early diastolic mitral annulus velocity.

Kaplan-Meier curves for cardiovascular mortality. In the analysis performed by the Kaplan-Meier method, the death due to cardiovascular diseases the E/e' ratio group higher than 15 occurred more than lower group (p = 0.005). E, early diastolic mitral inflow velocity; e', early diastolic mitral annulus velocity.
Factors affecting mortality and the incidence of CVD
In the Cox regression analysis performed, mortality increased with increases in age (p = 0.000), CRP level (p = 0.018), and E/e' ratio (p = 0.048) (Table 5). The incidence of CVD increased as the age (p = 0.008) and E/e' ratio increased (p = 0.045) and as the LV EF (p = 0.003) decreased (Table 6).
ROC curve of mortality in relation to E/e' ratio and cardiovascular events
In the ROC curve, regarding mortality, when the E/e' ratio was 14.4, the sensitivity was 62.9% and the specificity was 72.2% (Fig. 5A). Concerning the incidence of CVD, when the E/e' ratio was 13.08, the sensitivity was 63.2% and the specificity was 68.2% (Fig. 5B).
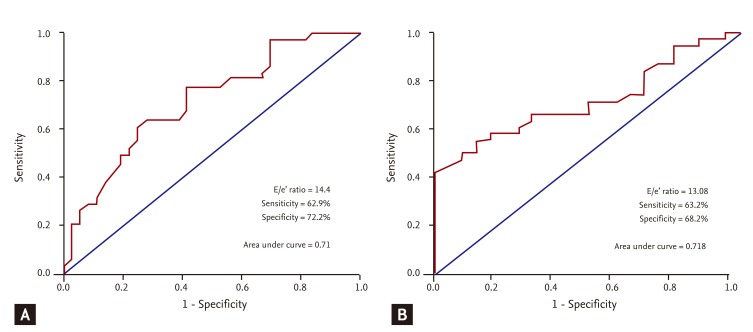
Receiver operating characteristic (ROC) curves of E/e' ratios for (A) mortality rates and (B) cardiovascular events. In the ROC curve for mortality, when the E/e' ratio is 14.4, the sensitivity is 62.9% and the specificity is 72.2% (A). Concerning the incidence of cardiovascular disease, when the E/e' ratio is 13.08, the sensitivity is 63.2% and the specificity is 68.2% (B). E, early diastolic mitral inflow velocity; e', early diastolic mitral annulus velocity.
DISCUSSION
CVDs are major causes of death in CKD and ESRD patients [1]. Among the CVDs, HF increases mortality associated with the cardiovascular system in patients with CKD and ESRD, which means that the prognosis of patients with HF is poor [1,2].
HF can be subdivided into systolic HF and diastolic HF. Diastolic HF is defined as cases satisfying more than three of the nine clinical conditions used in the PEP-CHF trial [7]. The objective test standard was defined as cases that showed two of the following findings in echocardiography: EF > 50%, dysfunction of the left ventricle during the diastolic phase (i.e., enlargement of the left ventricle), abnormal Doppler results for the LV inflow; and E/e' ratio > 10 [7].
Although the prognosis for diastolic HF is better than for systolic HF, the annual mortality rate is approximately 10%. In addition, this rate is on the increase as the incidences of diabetes and hypertension increase [3]. Patients with diastolic HF are mostly elderly (age range, 74 to 76 years), and females make up of the majority (62% to 66%) of these cases. Diastolic HF frequently develops in association with several other diseases, such as hypertension (55% to 77%), coronary artery disease (36% to 53%), atrial fibrillation (32% to 41%), diabetes (32% to 45%), CKD (23% to 26%), cerebrovascular diseases (15%), obesity, and anemia [3]. Diseases associated with diastolic HF are risk factors for CKD and, thus, in patients with CKD, similarly, the incidences of diastolic HF and CVD are increased [5]. In the present study of 186 patients with CKD who visited our hospital complaining of dyspnea, systolic HF was discovered in 50 patients (36.7%) and diastolic HF was diagnosed in 136 patients (73.1%). Among these, 83 (44.6%) patients had diastolic HF only, and it was found that diastolic HF strongly influenced the etiology of dyspnea.
As reported previously, BNP is a protein that is secreted from heart muscles during hemodynamic overload and, as it has been reported to reflect LV end-diastolic wall stress [8], it is a widely used marker for the evaluation of diastolic HF and assessment of prognosis. Nonetheless, in patients with CKD with deteriorated kidney function and in patients with ESRD, the levels of BNP are basically increased, which limits its usefulness [8]. In particular, for patients in whom EF is preserved (in other words, those with diastolic HF) it should be diagnosed carefully. For a more accurate evaluation of heart function, pulmonary capillary wedge pressure (PCWP) was used to evaluate the LV filling pressure. As this involves an invasive procedure, its use is limited. It has been reported that in echocardiography, the E/e' ratio derived from tissue Doppler images correlates significantly with the PCWP measured by invasive methods [8]. As a result, the E/e' ratio has been used widely to evaluate diastolic HF in patients with HF.
Diastolic HF is diagnosed on the bases of clinical symptoms and echocardiographic assessments of the retained systolic function of the left ventricle and the state of deterioration of diastolic function [3]. The E/e' ratio is an index that can be used to evaluate the LV filling pressure. It is applied to diagnose diastolic HF [2,4,6]. The E/e' ratio is an index that reflects accurately the LV filling pressure [6], and it is a predictive factor for the development of CVDs in patients with hypertension [3,6]. In patients with myocardial infarction, the E/e' ratio is considered to be a strong predictive factor for survival [4]. HF is seen in more than 50% of patients with renal failure [9]. Thus, for patients with CKD and ESRD, it is more important to diagnose HF early and to initiate its treatment [9].
The E value reflects the status of the mitral valve, as determined by the LV relaxation and the left arterial pressure [8-10], and the state of the relaxation of the myocardium can be evaluated by assessing the value of e'. If relaxation of the myocardium is abnormal, not only the magnitude of e' is decreased but also the time of opening of the mitral valve is delayed [8-10]. An E/e' ratio < 8 is considered to be normal, and a ratio > 15 is considered to reflect an increase in the LV filling pressure [11-13]. In patients with normal EF, tissue Doppler echocardiography has been used to evaluate LV filling pressure and LV stiffness [11]. The results of the present study show that, in patients with an E/e' ratio > 15, the incidences of mortality and CVD are statistically significant, whereas the LV EF, GFR, and BNP are not significant. Therefore, in CKD patients, an increase in the E/e' ratio may increase mortality, as well as the development of CVD without any association with factors that increase systolic HF and BNP (Figs. 2 and 3). In addition, in patients with CKD associated with diastolic HF, age, CRP, and the E/e' ratio were found to be factors that predict mortality. Age, EF, and the E/e' ratio were found to be factors that predict the incidence of CVD. In particular, the E/e' ratio was found to be predictive of both mortality and the incidence of CVD (Tables 5 and 6).
In patients with CKD, hypertension frequently induces diastolic failure and induces ventricular hypertrophy, myocardial dysfunction, fibrosis due to the deposition of collagen in connective tissues, and myocardial ischemia [14]. CKD is associated with hypertension in many cases due to several factors and, regardless of the stage of CKD, deterioration of diastolic function may be an associated phenomenon. Therefore, regardless of the level of deterioration of renal function, screening by echocardiography is required. Considering that the E/e' ratio and the level of renal failure were not correlated in a statistically significant manner, echocardiography should be performed for patients with CKD, and the association with diastolic failure should be assessed. For patients with major risk factors for the induction of CKD, such as diabetes and hypertension, evaluation of the E/e' ratio by echocardiography is crucial [15,16]. In patients with CKD, for the diagnosis of asymptomatic diastolic failure, an E/e' ratio > 11 (assessed by tissue Doppler echocardiography) is considered to correspond to PCWP > 15 mmHg [8,12,13]. Application of the E/e' ratio would facilitate the early diagnosis of these patients, as well as the early diagnosis of diastolic HF and early initiation of treatment, and would ameliorate the deterioration of renal failure and the deterioration of HF caused by cardio-renal syndrome [17-19]. In the present study, E/e' ratios of 14.40 and 13.08 in the ROC curve were predictive of mortality (62.9% sensitivity, 72.3% specificity) and the incidence of CVD (63% sensitivity, 68.2% specificity). In patients with CKD or ESRD, it may be useful to apply lower E/e' ratios than the currently used value of 15 (Fig. 5).
In conclusion, diastolic HF is an important factor that increases mortality related to the cardiovascular system in patients with CKD whose extent of kidney function deterioration differs [20]. As a non-invasive method to allow early assessment, the E/e' ratio could be applied usefully. For the diagnosis of HF in patients with CKD and the evaluation of responses to treatments, further studies using more accurate, non-invasive, simple, and highly reproducible measurement methods are required.
KEY MESSAGE
1. Diastolic heart failure is an important factor increasing the mortality pertinent to the cardio-vascular system in chronic kidney disease (CKD) patients.
2. The E/e' ratio estimated by tissue Doppler imaging can predict mortality and cardiovascular events in CKD patients with diastolic dysfunction.
Notes
No potential conflict of interest relevant to this article is reported.