Sonographic evaluation of esophageal achalasia
Article information
A 32-year-old man was referred to the gastroenterology department for dysphagia with both solids and liquids. The symptoms were progressive with considerable weight loss over an 8-year period. High resolution manometry was performed, which revealed type 1 achalasia, diagnosed according to the Chicago classification. A barium-swallow study showed a dilated esophagus with tapering distally. Abdominal ultrasound also demonstrated a dilatation of the distal esophagus with regular thickening of the esophagogastric junction (EGJ) with a "bird's beak appearance" (Fig. 1A). Normally, an elongated pseudokidney pattern without dilatation is noted in healthy subjects (Fig. 1B). Given the sonographic findings, a diagnosis of esophageal achalasia was suspected. The patient underwent a peroral endoscopic myotomy, and at the 18-month follow-up the dysphagia had completely resolved.
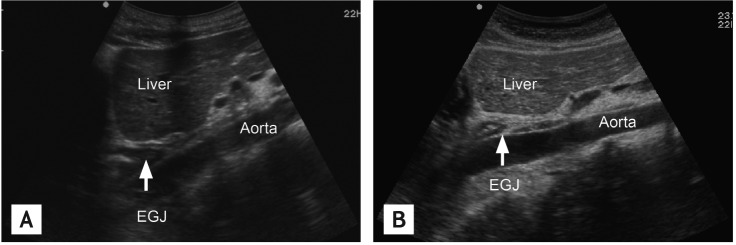
(A) A dilatation of the distal esophagus with regular thickening of the esophagogastric junction (EGJ) with a "bird's beak appearance" in a patient with achalasia. (B) An elongated pseudokidney pattern without dilatation in a healthy subject.
Esophageal manometry is the gold standard for dysphagia assessment, but it is generally not part of the initial work-up. Pseudoachalasia resembles achalasia, and is characterized by lesions that cause narrowing of the EGJ and esophageal dilatation. A barium swallow does not rule out pseudoachalasia. Endoscopic ultrasonography (EUS) is useful for evaluating patients with suspected pseudoachalasia due to tumor infiltration. However, it is expensive and requires an experienced endosonographer. The present report shows that abdominal ultrasound is a useful tool for evaluating the EGJ, and is helpful to diagnose achalasia while excluding pseudoachalasia. However, pathologic changes cannot be identified in fasting patients, and examinations should be performed following water ingestion. Further studies are required to determine whether abdominal ultrasound can replace EUS for the evaluation of achalasia.
Notes
No potential conflict of interest relevant to this article was reported.