Guideline on the prevention and control of seasonal influenza in healthcare setting
Article information
INTRODUCTION
Background and purpose
Influenza is an acute respiratory disease caused by influenza virus infection. In Korea, epidemic occurs mostly in winter. The characteristic symptoms of influenza consist of abrupt fever, cough, fatigue and other constitutional and respiratory symptoms. Influenza is usually a self-limiting illness without complications, but some patients at higher risk can experience severe complications or die. Influenza is a contagious disease that infects many patients in a short period, so the spread of influenza in the community can lead to public health issues or socioeconomic problems.
Influenza within a medical institution has a different epidemiology and effects compared to influenza in the community. Medical institutions have high number of visits from influenza patients and wards are crowded with high risk patients. Therefore, there is a high possibility that influenza can spread between patients in a medical institution, and influenza can cause more complications and mortality in this setting. Hence, to minimize the damage from influenza in a medical institution, the effective infection control measures are important to prevent influenza and its spread. The purpose of this guideline is to prevent and control seasonal influenza in a medical institution based on the evidences and current situation in Korea.
Scope and subjects
The subject institutions of the guideline are private clinics, general hospitals, tertiary hospitals, and long term care hospitals. The scope of the guideline is seasonal influenza, and it cannot be applied in the same manner to pandemic influenza or highly pathogenic avian influenza. The epidemiology, clinical symptoms, diagnosis, tests, and treatment of influenza are addressed as an introduction, but the recommendations suggested by the guideline are limited to prevention and control of influenza in a medical institution. Guideline on the use of antivirals other than infection control purposes is discussed in a seperate guidelline [1].
Method of development
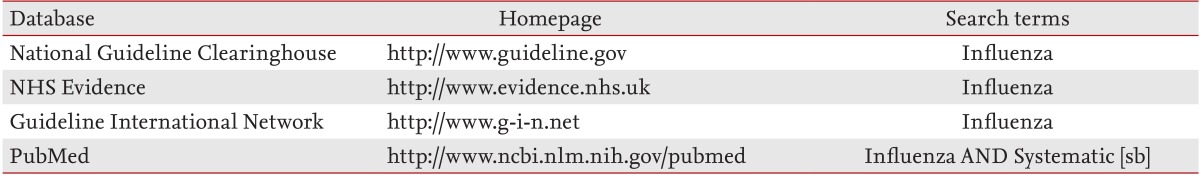
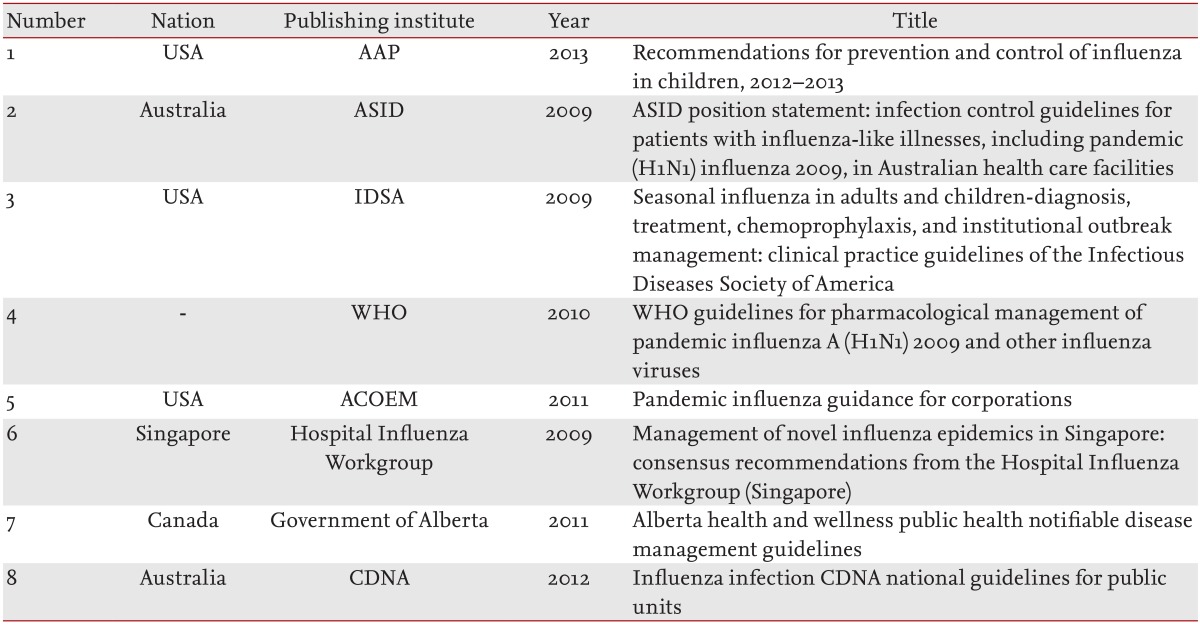
As the first step, a guideline development committee was organized consisting of six professionals including infectious disease specialists, an infectious control nurse, and a methodology specialist, so that specialists from multiple disciplines could participate in the development process. The second step was to systematically examine the related guidelines. The influenza related guidelines published from 2009 to 2013, only those in English and Korean were included. The guidelines were limited to those developed by Government or professional associations, and were searched from four databases. The databases and search words are presented in Table 1. The retrieved treatment guidelines were reviewed by two members of the development committee to select eight treatment guidelines appropriate to the scope of this guideline, and the selected guidelines are presented in Table 2. The third step was to create a table of contents for the guideline based on the published guidelines. Due to the characteristics of the guideline on the prevention and control of infection, the relevant content was described rather than listing key questions. The fourth step was to construct contents according to domestic and foreign guidelines, related literature searches, and specialist opinions. The level of the recommended items was not ranked, and the recommendations were proposed and composed through discussion by the development committee. In the fifth step, the recommendations were reviewed by three specialists and also approved by Korean Society of Infectious Diseases and Korean Society for Nosocomial Infection Control.
DEFINITIONS
Influenza-like illness
Generally, influenza-like illness (ILI) is defined as acute respiratory symptoms accompanying fever, and influenza can be suspected when it occurs during influenza season. The case definition used in the influenza surveillance system of the Korea Centers for Disease Control and Prevention is a case with sudden-onset fever of 38℃ or more accompanied by cough or sore throat [2].
High risk groups
The definition of high risk groups is slightly different between various clinical guidelines, but the following persons are commonly included [3-6].
Persons at high risk for severe or complicated influenza
Children aged less than 2 years and adults aged 65 years or older
Persons with chronic pulmonary diseases, cardiovascular disorders (except controlled hypertension), chronic renal diseases, chronic hepatic diseases, chronic metabolic disorders, hemoglobinopathies, neurologic disorders (including neuromuscular diseases, epilepsy, cerebral infarction, cerebral palsy, etc.), and malignancies
Persons with immunosuppression, including that caused by immunosuppressants or human immunodeficiency virus (HIV) infection
Women who are pregnant or postpartum (within 2 weeks after delivery)
Children receiving chronic aspirin therapy
Persons with obesity
Residents of long-term care facilities
Healthcare workers
'Healthcare workers' used in this guideline is defined as any person who can be exposed to the patients' surrounding environment or have contact with patients, by visiting regularly or residing in a medical institution. This includes staff employed by the medical institution or a related institution to work at the medical institution, students in practical training, trainees, and volunteers.
Example: doctors, nurses, assistant nurses, medical technicians, pharmacists, administrative staff, clerical staff, students, trainees, facility managers, cooks, central supply department workers, laundry workers, cleaners, security staff, volunteers, etc.
In the domestic medical environment, there are many cases where caregivers or guardians of patients reside in the medical institution. Considering this situation, applying the recommendation of this guideline to caregivers and guardians is helpful to manage influenza effectively in a medical institution though they are not employed by the medical institution or related institutions.
INFLUENZA OVERVIEW
Influenza is an acute febrile illness caused by infection of influenza A or B virus. It is a contagious infectious disease characteristically having an outbreak with an incidence rate of 10% to 40% during an influenza season of 5 to 6 weeks [7].
Epidemiology
In Korea, an influenza epidemic usually occurs from October to April of the following year, and the peak of the epidemic is usually in December and January. Influenza occurs most frequently in children and adolescents between 5 and 14 years of age. Hospitalization from influenza occurs mostly in children aged less than 5 years and the elderly aged 65 years or older, and mortality is highest among the elderly aged 65 years or older. There are no domestic epidemiologic data on influenza, but it is estimated that excess death from influenza and pneumonia is 1.36 to 1.53 per 100,000 population and it is accounts for approximately 1% of the total death [8].
The occurrence of influenza within the medical institution increases during influenza season because many influenza patients are hospitalized from community and healthcare workers or visitors also get influenza. Influenza among hospitalized patients is known to occur at a mean ratio of 0.3 to 0.8 cases per 100 hospitalized patients [9-11]. In a medical institution where an outbreak of influenza occurs, the attack rate increases to 0.7% to 20%, and it can increase to more than 30% in the ward where the outbreak occurred [11-16]. When an influenza outbreak occurs in a long-term care facility with many elderly patients, the attack rate can increase up to 70% [17]. In healthcare workers taking care of influenza patients, the attack rate is diverse from 11% to 59% [13,14]. When aggressive infection control measures were implemented on healthcare workers such as vaccination, reporting and monitoring of respiratory symptoms, and exclusion from work when developing symptoms, the attack rate in healthcare workers was reported to be maintained at less than 2% [18].
The mortality of influenza occurring in medical institution is diverse according to the characteristics of the patients. The mortality is not high in infants without severe cardiovascular diseases, but the mortality of patients in general hospitals or long-term care hospitals was 16%, and especially, the mortality of intensive care unit patients, hematopoietic stem cell transplantation patients, or acquired immune deficiency syndrome patients is reported up to 33% to 71% [15,16,18-20]. Therefore, infection control to reduce influenza and its outbreak within a medical institution is very important.
Transmission
The influenza virus is spread through 1) direct contact with a patient, 2) contact with the surrounding environment of a contaminated patient, and 3) inhalation of a droplet that includes the virus. The influenza virus can survive for 5 minutes on a contaminated hand, 8 to 12 hours on contaminated clothing or tissue, and 24 to 48 hours on contaminated metal or plastic. The virus can move onto a hand after staying up to 15 minutes on contaminated clothing or tissue, and up to 2 to 8 hours on contaminated metal or plastic [21]. In animal models, influenza has been transmitted in close, separated spaces without direct contact with infected animal or its surroundings and outbreak of influenza in confined spaces such as aircrafts have been reported, which suggest the possibility of airborne transmission in certain circumstances.
When the influenza virus is transmitted, influenza symptoms develop in approximately 50% of patients, and even asymptomatic persons can shed influenza virus. Young adults and middle aged adults are infectious 1 day before the onset of symptoms, and infectivity rapidly decreases at 3 to 5 days after symptoms onset, and 20% to 30% of cases can shed the virus up to 5 to 10 days after the initial day of symptoms [22]. Young children can spread the virus up to 3 weeks [23]. Use of antiviral agents can decrease the period of viral shedding. In severe influenza patients requiring hospitalization, the ratio of detecting virus RNA 1 week after developing symptoms was 57.1% when antiviral agents were not used, while it was 14.3% when antiviral agents were used within 48 hours of symptom onset [24]. Immunocompromised patients are known to shed the virus for a longer period than healthy people. In elderly patients or patients with underlying conditions, around 30% were confirmed to shed the virus for 1 week or more after developing symptoms. In the 2009 influenza outbreak, prolonged viral shedding for 2 weeks or more was reported in severely immunocompromised patients even when antiviral agents were used.
Clinical course
After transmission of the influenza virus, symptoms occur after approximately 1 to 4 days of a latent period. Around 50% are asymptomatic infections, but there is a higher rate of developing symptoms in children.
Typical influenza show sudden-onset fever accompanied by cough or sore throat, and there could be systemic symptoms such as lethargy, headache, myalgia, and joint pain, or respiratory symptoms such as cough, sore throat, rhinorrhea, and dyspnea. Gastrointestinal symptoms like diarrhea or vomiting, or ocular symptoms like ocular pain or photosensitivity can also accompany the infection.
In uncomplicated influenza, the symptoms usually improve after 3 to 7 days even without treatment, but cough and lethargy can continue for more than 2 weeks. In high risk groups, severe complications can accompany the infection or underlying diseases can worsen (high risk groups; refer to "Definitions" section). The most common complication is pneumonia, and other complications such as otitis media, sinusitis and the aggravation of underlying cardiovascular diseases, chronic liver diseases, or chronic renal diseases can be occurred.
Diagnosis
When ILI develops during influenza season, it can be clinically diagnosed as influenza. When ILI is defined as sudden fever accompanied by cough or sore throat, the positive predictive value is reported to be in the 79% to 88% range in adults in community [25]. Therefore, influenza should be suspected in medical institutions during influenza season when any hospitalized patient has new-onset fever or respiratory symptoms, underlying respiratory symptoms worsen in elderly patients, there are no symptoms other than fever in infant and patients in serious condition with fever or hypothermia.
Laboratory methods to diagnose influenza include rapid antigen test (RAT), reverse transcriptase-polymerase chain reaction (RT-PCR), serology, and virus culture. RAT and RT-PCR are used in clinical situations where results need to be confirmed quickly. The optimal clinical specimen for children or adults is nasopharyngeal aspirate or swab, and for infants, nasal aspirate or swab [26-28]. Time-wise, detection rate is higher when it is collected closer to the illness onset (within 72 hours). Endotracheal suction and the broncho-alveolar lavage have a high detection rate when a lower respiratory tract infection is accompanied.
RAT can be used easily in all medical institutions because it is point-of-care testing using the diagnostic kit without any other laboratory equipment and provides results in less than 15 minutes. It has high specificity of more than 90%, but its sensitivity is lower than that of RT-PCR (children 70%-90%, adult < 40%-60%), so it cannot be used as confirmation of a diagnosis [6,29-31]. RT-PCR has high sensitivity and specificity, so it can be used as a confirmation test. The results can be obtained within 4 to 6 hours when tested in the laboratory of a medical institution, but it may be difficult to obtain prompt results when samples are sent to an external laboratory [5].
Treatment
Guideline for antiviral treatment and chemoprophylaxis of seasonal influenza and guideline for treatment of severe influenza have been developed separately [1].
PREVENTION AND CONTROL OF INFLUENZA IN A MEDICAL INSTITUTION
A multi-faceted effort is required to prevent the occurrence and transmission of influenza within a medical institution. Influenza virus in health care settings can spread through healthcare workers and visitors as well as between patients, so infection prevention and control have to include all people at a medical institution. The basic elements for influenza prevention and control are as follows:
Influenza vaccination
Adherence to precautions
Influenza surveillance
Infection control according to the environment and facilities of the institution
Use of prophylactic and therapeutic antiviral agents
Education of patients, guardians, and medical staff
Recommendations for each of the above basic elements are presented below.
Vaccination
Vaccination is the most effective way to prevent influenza. Vaccination on healthcare workers and hospitalized patients is a basic element for preventing influenza outbreak in a medical institution.
Vaccination against seasonal influenza should be undertaken every year before upcoming influenza season. Subjects for vaccination in a medical institution are all hospitalized patients older than 6 months and healthcare workers without contraindications. Especially, for high risk patients such as those mentioned below, who are at higher risk of developing severe or complicated influenza, vaccination should be carried out meticulously. And vaccination should be delivered to healthcare workers to minimize the possibility of exposure of influenza to high risk patients.
Priority subjects for vaccination
-
Persons at high risk for severe or complicated influenza
- Children aged less than 2 years and adults aged 65 years or older
- Persons with chronic pulmonary diseases, cardiovascular disorders (except controlled hypertension), chronic renal diseases, chronic hepatic diseases, chronic metabolic disorders, hemoglobinopathies, neurologic disorders (including neuromuscular diseases, epilepsy, cerebral infarction, cerebral palsy, etc.), and malignancies
- Persons with immunosuppression, including that caused by immunosuppressants or HIV infection
- Women who are pregnant or postpartum (within 2 weeks after delivery)
- Children receiving chronic aspirin therapy
- Persons with obesity
- Residents of long-term care facilities
Healthcare workers
Currently, inactivated influenza vaccine (IIV3), vaccine trivalent containing immunologic adjuvant and live-attenuated influenza vaccine (LAIV) are available in Korea. Several types of vaccine are not currently available in Korea: intradermal vaccine, and inactivated influenza vaccine quadrivalent (IIV4).
Both inactivated influenza vaccine and LAIV can be used for vaccination at medical institutions, but only inactivated influenza vaccine is recommended for severe immunocompromised patients and for healthcare workers who have close contact with these patients. Inactivated influenza vaccine is recommended for patients taking prophylactic antiviral agents for the effect of the live-attenuated influenza vaccination is reduced in these patients.
For people who have contraindications or precautions to vaccination (severe allergic reaction such as anaphylaxis to eggs or vaccine components, prior experience of severe fever after vaccination, history of Guillain-Barre syndrome within 6 weeks of a previous influenza vaccination), chemoprophylaxis can be considered instead of vaccination. Cell-culture based influenza vaccine is planned to be released later. Cell-culture based vaccine is egg-free unlike the existing egg-based influenza vaccines. Therefore cell-culture based influenza vaccine can be used in patients who have severe allergic reaction to eggs. For the children aged 6 months to 8 years who get influenza vaccine for the first time in their lives, the second dose should be given one month after the first dose to obtain the appropriate immunity.
Vaccination for hospitalized patients
Vaccination against seasonal influenza is universally recommended to all people older than 6 months. This vaccination strategy is also applied to hospitalized patients in a medical institution.
For patients who are suffering from moderate to severe acute febrile illness accompanied by a fever of 38℃ or higher, the vaccination might be delayed until the symptoms improve. For patients with moderate to severe acute illnesses without fever, influenza vaccination should be considered cautiously. Vaccination should be undertaken without delay in patients under long term care for chronic illnesses and not acute illnesses.
Patients admitted during an influenza season should be asked whether they have received an influenza vaccination. Then vaccination should be performed for unvaccinated patients.
Vaccination for healthcare workers
Influenza vaccination to healthcare workers prevents influenza in vaccinee and decreases the subsequent absences. Secondly it reduces the transmission of influenza virus in healthcare settings [32,33].
Many patients admitted at medical institutions are at higher risk of developing severe or complicated influenza, therefore vaccination of healthcare workers is strongly recommended since it can reduce influenza mortality in medical institutions [34,35]. Administrative policies are required to deliver vaccination to all healthcare workers without contraindications to vaccination.
Although data regarding vaccination rate of healthcare workers in Korea is limited, reported vaccination rate in university hospitals was 23.0% to 78.0% [36,37]. Considering that the vaccination rate is relatively lower in long-term care hospitals and clinics, the overall vaccination rate of healthcare workers is expected to be lower than reported data. Because vaccination is the key strategy to prevent influenza in healthcare settings, influenza vaccination to all healthcare workers should be encouraged at all medical institutions.
Adherence to precautions
Influenza is usually transmitted through droplet of large particles generated by cough or sneezing of an influenza patient. In some cases, it can spread through smaller aerosols. Droplet can travel less than 1 m, and therefore it is spread by close contact. Indirect contact can also transmit influenza virus from contaminated surfaces to eyes or mouth through hands. Thus, standard and droplet precautions should be implemented. During procedures which generate aerosols, airborne precautions should be followed [38].
Adherence to standard precautions
To prevent the spread of influenza, all healthcare workers should adhere to standard precautions. Standard precautions are applied to patients potentially infected or colonized with an organism that could be transmitted, and this includes patients with respiratory infections, inclusive of influenza.
Healthcare workers should perform hand hygiene before and after contact with patient, contact with potential source of infection and wearing personal protective equipment such as gloves. Hand hygiene can be performed using water and soap, or using alcohol hand rub without water. When hand is visibly soiled, they should wash their hands with water and soap. Medical institutions should supply materials for hand hygiene.
Healthcare workers should wear gloves when they contact potential source of infection, and wash their hands after taking off gloves. Gloves should be changed for each patient, and should not be washed with the purpose of reuse.
When healthcare workers are expected to contact with blood, body fluids and secretions or excretions from respiratory tract or other system, they should wear gown before contact with patients. They should take off their gowns before leaving the patient's surroundings, and then wash their hands. The gown should be changed for each patient.
Adherence to droplet precautions
For previously healthy adult patients they should be isolated for 5 days after symptom onset. When fever continues for more than 5 days, isolation should be maintained until the patient is afebrile for 24 hours or more without any antipyretics. However, in children or severely immunocompromised patients, the viral shedding may be prolonged and isolation period may be extended.
Patients with suspected or confirmed influenza should be isolated in a single patient room. When single room is not available, the patient should be assigned to the cohort room. Healthcare workers should wear masks when they enter rooms with patients suspected or confirmed influenza. They should take off the mask when leaving the room, dispose it in a medical waste box, and hand hygiene should be followed.
When a patient on droplet precaution moves outside the room, the patient should use a mask and follow respiratory and cough etiquette, and hand hygiene. Transferring department should be informed about the patient with suspected or confirmed influenza.
Precautions when performing aerosol-generating procedures
Procedures that can generate aerosols such as bronchoscope, sputum induction, tracheal intubation or extubation, autopsy, and cardiopulmonary resuscitation have a risk of exposure to influenza through aerosols, so airborne precaution should be implemented. Only the essential members should be attended, and the procedure should be undertaken by vaccinated personnel.
Procedures should be performed in negative-pressure rooms, where air ventilation is possible through HEPA filters allowing a minimum of 6 to 12 air changes per hour. The door should be closed all the time. Negative pressure room should be checked to ensure the proper operation of negative pressure.
The practitioner performing the procedure should wear gloves, a gown, facial mask or goggles to cover the entire face, and a N95 mask or other respiratory protective equipment with equivalent function with N95 mask. The surface of immediate surroundings should be disinfected following procedure.
Influenza surveillance
For early detection and response to occurrence of influenza within a medical institution, infection control activities are required during the influenza season to monitor the occurrence of ILI and to facilitate laboratory tests when ILI occurs. When an ILI occurs in a medical institution, laboratory tests should be actively performed for patient management and prevention of transmission.
A RAT is performed on patients who have an ILI. When the RAT results are positive in patients who have an ILI during influenza season, additional laboratory testing is not needed. However when the results are negative, RT-PCR can be considered due to the possibility of false negative results of RAT. Because the laboratory test for patients who have ILI during influenza season is to manage influenza patients and prevent transmission within a medical institution, the use of therapeutic antiviral agents for treatment of individual patients can be considered whether influenza tests are taken or not. However, a diagnostic method for surveillance can be chosen according to the situation of each institution.
Surveillance during influenza season
Continual surveillance on the occurrence of ILI in hospitalized patients is necessary during influenza season. Even when hospitalized patients are not showing an ILI during influenza season, influenza should be suspected, and laboratory tests should be performed when there are new symptoms of fever and respiratory symptoms; underlying respiratory illness is aggravated in elderly patients regardless of fever; symptoms do not exist other than fever in child patients, and when patients are in serious condition with fever and hypothermia.
Surveillance in patients with contact to influenza
Active surveillance should be performed to monitor the occurrence of ILI or fever in patients who have come into contact with patients suspected or confirmed to have influenza, and laboratory tests should be performed for patients who show symptoms. The risk of influenza is highest in patients who have been within 1 m of an influenza patient, and surveillance is needed if influenza symptoms occur in patients who use the same hospital room or ward.
Surveillance during an outbreak in a medical institution
An influenza outbreak in a medical institution can be suspected when two or more patients develop acute febrile illness symptoms within 72 hours in a single medical institution, and one of them has laboratory confirmed influenza. The decision of whether it is an outbreak is to be made according to the epidemiologic relationship between the patients.
Surveillance should be actively performed for the occurrence of ILI or fever in all areas of the medical institution including the areas where the influenza patients have not been, and laboratory testing should be performed for symptomatic patients. Active surveillance should be continued until the end of the outbreak, and active surveillance is to be maintained until 1 week after the occurrence of the last influenza patient.
Infection control according to the environment and facilities of the institution
The entrance of a medical institution
It is important to prevent the spread of influenza within a medical institution through early detection of ILI patients. Information posters should be posted in conspicuous positions such as at the entrance and reception desk during influenza season, and employees should be positioned to instruct cough etiquette and to provide masks to patients with ILI (Figure 1). Patients with ILI should be guided to moving routes which other patients do not use. The moving route should be decided beforehand to prevent confusion.
Outpatient clinic
When installation of a quarantine waiting room is possible
Information posters should be posted in conspicuous places around the reception desk during influenza season (Figure 2). Reception employees are to instruct cough etiquette to patients with ILI, and lead them to the quarantine waiting room after providing them with masks to wear. In the quarantine waiting room, the patients are to sit more than 1 m away from each other. In addition, movement outside the quarantine area should be minimized to reduce the opportunity of contact with other patients.
Tissues should be provided in the quarantine room for patient use when coughing, and trashcans with lids that can be opened without using hands should be provided to dispose of the contaminated tissues. Facilities for hand hygiene and disposable towels should be provided. When there is not enough space for quarantine, a barrier can be used to divide the space. Appropriate ventilation should be provided in the quarantine waiting room and consulting room.
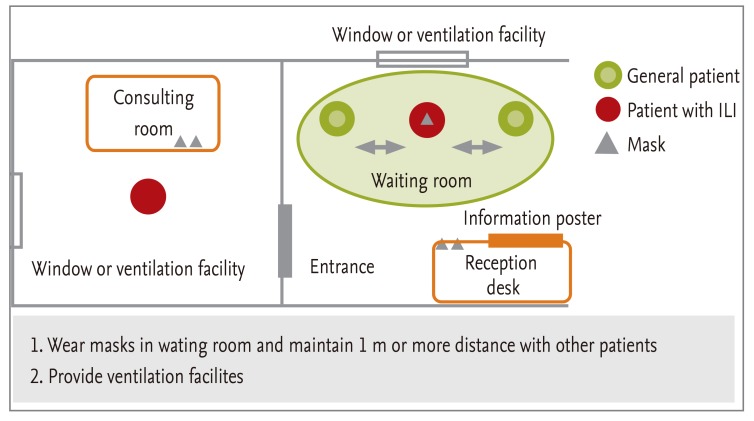
When installation of a quarantine waiting room is difficult
Information posters should be posted in conspicuous places around the reception desk during influenza season to promptly identify patients with ILI (Figure 3). These patients should be instructed of cough etiquette, and lead to waiting room after providing them with masks to wear. Patients are to sit more than 1 m away from each other. Movement should be minimized to reduce the opportunity of contact with other patients. Tissues should be provided in the waiting room for patient use when coughing, and trashcans with lids that can be opened without using hands should be provided to dispose of the contaminated tissues. Facilities for hand hygiene and disposable towels should be provided. Appropriate ventilation should be provided in the waiting room and consulting room.
Emergency room
It is important to prevent spread of influenza within an institution through early detection of influenza patients. Information posters should be posted in conspicuous places around the emergency room entrance and reception desk during influenza season (Figure 4). A triage area should be installed to question all patients regarding fever and respiratory symptoms.
Masks should be provided to patients with fever or respiratory symptoms, and a separate quarantine space should be prepared for waiting and treatment. Patients are to sit more than 1 m away from each other. Movement should be minimized to reduce the opportunity of contact with other patients.
Tissues should be provided in the quarantine waiting room for patient use when coughing, and trashcans with lids that can be opened without using hands should be provided to dispose of contaminated tissues. When there is not enough space for quarantine, a barrier can be used to divide the space. Appropriate ventilation should be provided in the quarantine waiting room and consulting room.
When hospitalization is decided, the patient should be promptly moved to a ward. Patients with ILI are to wear masks during transfer, and are to wash their hands before moving. Patients suspected of influenza are to be guided to moving routes which other patients do not use. The moving route should be decided beforehand to prevent confusion. Medical staff moving the patient should wear appropriate personal protective equipment.
Ward
To prevent the spread of influenza during influenza season, patients with ILI should be separated in their placement. In principle, they should be hospitalized in single isolation rooms. However, when there are too many patients and individual isolation is difficult, cohort isolation rooms should be used (Figure 5). When there are no cohort rooms or they cannot be used, a barrier can be used to separate part of a room. However, precautions should be taken so they are not placed in the same room with high risk patients. The spacing between beds in a cohort isolation room is to be maintained at 1 m or more. The doors to the isolation rooms should be closed, and there should be sufficient external ventilation.
Masks should be placed at the room entrance, and thorough education is necessary for the proper wearing of masks and washing of hands before entering an isolation ward. Patients suspected or confirmed of influenza should always wear masks, and opportunity for contact with other general patients in the ward should be limited. When movement to the outside the ward is inevitable, the patient should be moved after wearing a mask and washing their hands.
There is need to educate and restrict visitors. Surveillance is needed to check for fever and respiratory symptoms in visitors, and hospital visits should be restricted. Visitors should be limited to members who are needed for the care and emotional support of the patient.
Infection control according to different situations
Sporadic cases of influenza in hospitalized patients
Laboratory diagnosis when patients suspected of influenza occur
Diagnosis of influenza in local community during influenza season consists of mainly clinical symptoms, but laboratory tests should be actively performed for patients suspected of influenza in a medical institution (refer to "Surveillance during influenza season" section).
Patient management
When a patient suspected of or confirmed with having influenza occurs,
1) Adherence to precautions
The standard precautions and droplet precaution guidelines should be implemented.
2) Restriction of movement
Patients with suspected of confirmed influenza should be restricted from common activities, and they are to stay in individual rooms or cohort isolation rooms.
3) Administration of antiviral agents for treatment
Administration of antiviral agents not only has the effect of treating the influenza patient, but can also reduce the amount of viral shedding and decrease the period of viral shedding. Therefore, antiviral agents should be used actively to treat influenza occurring within medical institutions. For details regarding the administration of antiviral agents for treatment, refer to the guideline for using antiviral agents for seasonal influenza [1].
The possibility of drug resistant influenza should be considered when influenza occurs in patients administered with antiviral agents for more than 72 hours for preventive purposes and when symptoms do not improve and the virus is continually detected in RT-PCR despite administration of antiviral agents for treatment. When drug resistant influenza is suspected or confirmed, the appropriate drug should be selected in consultation with an infectious disease specialist. Patients with suspected or confirmed drug resistant influenza are to be more actively isolated than other influenza patients.
4) Surveillance and early treatment for influenza in patients exposed to influenza
Surveillance should be conducted for patients who have been exposed to patients with suspected or confirmed influenza (refer to "Surveillance in patients with contact to influenza" section). Prophylactic use of antiviral agent is classified as pre-exposure prophylaxis and postexposure prophylaxis. Pre-exposure prophylaxis can be considered restrictively in persons at high risk of severe complications (e.g, patients at organ transplantation unit or neonatal unit, severely immunocompromised patients) for whom influenza vaccine is contraindicated or expected to have low effectiveness.
Preventive use of antiviral agents for patients exposed to influenza should be limited to patients at high risk. As an alternative to the preventive use of antiviral agents, prompt administration of antiviral agents for treatment can be started when influenza symptoms occur. For details, refer to the guideline for using antiviral agents for seasonal influenza [1].
5) Duration of isolation
Duration of isolation precautions, such as implementing standard precautions and limiting activity area for patients with suspected or confirmed influenza is determined by the anticipated period of viral shedding and infectivity.
In general, isolation is maintained for 5 days after the onset of symptoms. When fever continues for more than 5 days, isolation can be discontinued only after there has been no fever for 24 hours without the use of antipyretics.
Children can shed the virus for a longer period than adults, so the isolation period for children can be extended compared to the general isolation period. Patients with severe immunosuppression can also discharge the virus for several weeks or more even when administered with antiviral agents. There is insufficient research regarding the period of infectivity in such cases. Laboratory tests such as RT-PCR cannot confirm whether infectivity is maintained. However, when viral shedding is continually confirmed in laboratory tests despite administration of antiviral agents, there is a possibility of a drug resistant virus, so the appropriate precautions should be taken before removing quarantine.
Management of high risk patients exposed to influenza
Definition of exposure
Exposure is defined as when there was contact within 1 m with patients with suspected or confirmed influenza showing symptoms. There is insufficient research regarding what length of exposure time allows propagation.
Definition of high risk group
Persons at high risk for severe or complicated influenza
Children aged less than 2 years and elderly aged 65 years or older
Patients with chronic respiratory disease, cardiovascular disorders (excluding isolated hypertension), chronic renal disease, chronic liver disease, metabolic disorders, hemoglobinopathy, neurologic disorders (neuromuscular diseases, epilepsy, cerebral infarction, cerebral palsy, etc.), and malignancy
Patients taking immunosuppressants or who are at immunodeficiency conditions such as HIV infection
Pregnant women and mothers who gave birth within 2 weeks
Children with long-term aspirin therapy, obesity, residents of long-term care facilities
Prophylactic use of antiviral agents for high risk patients with influenza exposure
Postexposure prophylaxis refers to the administration of antiviral agents to subjects who have been exposed to patients with influenza during the season. It was observed that there was a 79% to 81% preventive effect when zanamivir was used in subjects exposed to influenza, and 68% to 89% when oseltamivir was used. Prophylactic use of antiviral agents in high risk groups can be considered according to the evidence. However, there are issues regarding the cost-benefit, developing strains with resistance to antiviral agents resulting a breakthrough infection, and adverse effects by drugs, therefore it should be used on a case by case basis considering the influenza activity and condition of patients.
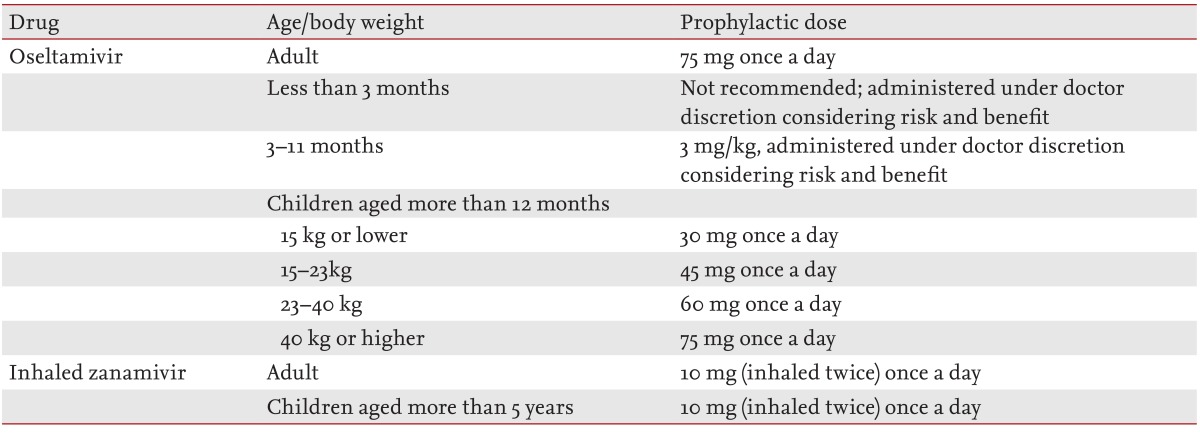
The use of antiviral agents for 10 days after exposure is recommended. Clinical research for prevention after exposure using oseltamivir has been usually conducted as a 7- or 10-day administration. A research using zanamivir was conducted as a 5- or 10-day administration. There have been few researches comparing the duration of prophylaxis for each drug. The prophylactic administration dosage is shown in Table 3.
When postexposure prophylaxis is not or cannot be offered, education about influenza symptoms should be provided and antiviral agents should be prescribed to patients who are observed to be developing flu-like symptom as soon as possible.
Outbreak
Definition of an outbreak
An outbreak at an institution can be suspected when there is a patient with laboratory confirmed influenza, and an epidemiologically related patient newly develops ILI within 72 hours.
Management
1) Adherence to precautions
The standard precautions and droplet precautions should be implemented.
2) Restriction of movement
Patients with suspected or confirmed influenza should be restricted from common activities, and they are to stay in individual rooms or cohorts.
3) Vaccination
Influenza vaccination should be provided to patients and medical personnel who were not immunized.
4) Administration of antiviral agents
The spread of influenza within a medical institution should be minimized by immediate administration of antiviral agents to laboratory confirmed patients and also to patients with suspected influenza. Prophylactic administration of antiviral agents to all hospitalized patients can result in premature termination of an outbreak [5]. However, the selection of patients and the decision for administration is made by the infection management staff and supervisor according to each outbreak situation and the characteristics of the medical institution.
Prophylactic use of antiviral agent is classified as pre-exposure prophylaxis and postexposure prophylaxis. Pre-exposure prophylaxis can be considered restrictively in persons at high risk of severe complications (e.g., patients at organ transplantation unit, severely immunocompromised patients, neonates at neonatal unit) for whom influenza vaccine is contraindicated or expected to have low effectiveness. Postexposure prophylaxis should be limited to high risk exposers. An alternative to chemoprophylaxis is administrating therapeutic antiviral agent to persons promptly who have developed signs and symptoms of influenza. For healthcare workers who did not or cannot receive a vaccination, prophylactic administration of antiviral agents should be considered. When there are differences between circulating strains and vaccine strains, administration of antiviral agents for all hospital workers can be considered during influenza season. Antiviral chemoprophylaxis can be administered up to 14 days after an outbreak, or up to 7 days from the initial day of the influenza-like symptoms of the last patient.
5) Active surveillance
During influenza season, surveillance should be performed every day to check for patients with fever and respiratory symptoms. When relevant to influenza-like symptoms, laboratory tests should be performed, and antiviral agents should be administered together with cohort isolation. Active surveillance is continued up to 7 days after the occurrence of the final patient. It should be considered that patients who have neurologic disease may not show the characteristic symptoms or signs of influenza.
Management and education of subjects excluding patients
Management of visitors
Visitors should be limited to only those who are necessary for emotional support and care. Visitors who have had contact with patients with influenza can be the source of influenza for other patients, staff and visitors. Visitors should be checked whether they have acute respiratory symptoms before entering the institution or ward.
Visitors should be educated about hand hygiene, standard and droplet precautions. Visitors are not allowed in areas where procedures generating aerosol are performed, and they should be instructed to minimize their movement within the medical institution.
Management of caregivers
If a caregiver did not receive an influenza vaccination, immunization should be recommended. Hand hygiene should be performed with water and soap, or hand sanitizer before and after contact with patient. Masks should be put on when contact is made within 1 m from patients. Surveillance should be performed to check for symptoms or signs of suspected influenza infection, and treatment should be given promptly when suspicious symptoms develop. Symptomatic caregivers should be discouraged from caring of the patient until their symptoms completely improve.
Management of healthcare workers
Healthcare workers should receive vaccination for seasonal influenza. They should be aware of the symptoms, signs, and complications from influenza, so consultation and early treatment should be received as soon as influenza-like symptoms develop. Standard precautions and droplet precautions are to be followed when contacting with influenza patients or patients with ILI. Airborne precautions should be implemented when performing aerosols-generating procedures such as tracheal intubation.
Healthcare workers with suspected or confirmed influenza
When healthcare workers have acute respiratory symptoms during influenza season, they should wear masks immediately and contact with patients should be suspended, and the infected person should report to supervisor. Duties are only to be resumed after confirming that fever is not present for 24 hours or more without the use of antipyretics. When respiratory symptoms remain at the time of returning to work, the symptomatic person should wear masks continually and perform hand hygiene thoroughly.
Medical staffs who contact with patients requiring a protected environment
When patients with severe immunodeficiency are infected with influenza, there is a high possibility of severe influenza, and the duration of viral shedding is also longer despite antiviral treatment. Hence, there is a high risk of influenza transmission and developing of drug resistance, therefore a protected environment is necessary. When workers who come in contact with severe immunodeficient patients with suspected or confirmed influenza, they are to be excluded from duties in the protected environment by changing duties or taking time off. The period being excluded from duties is to be for 7 days after the onset of symptoms. When respiratory symptoms continue for more than 7 days, the duration is extended until the symptoms disappear.
Duties of healthcare workers at higher risk for complications
Healthcare workers at higher risk for complications can be assigned to duties which refrain from exposure to influenza virus (e.g., refrain from procedures which can generate aerosols on patients with suspected or confirmed influenza).
Environment management
Influenza virus is usually spread through droplet while coughing, sneezing, or talking, but it can survive for 1 to 2 days on an environmental surface, and it can spread by contacting an environmental surface contaminated with influenza virus [39]. However, it is possible to remove with heat at 75℃ or higher, chlorine, hydrogen peroxide, iodophors (iodine-based antiseptics), and disinfectants such as alcohol [40].
Cleaning and disinfection
Cleaners should wear masks and gloves.
Surfaces that are frequently touched by patients (doorknobs, bedrails, tables, mattresses, phones, call bells) should be thoroughly disinfected every day and after patient discharge using environmental disinfectant (e.g., degree 4 ammonium agent, chloride based disinfectant [bleach diluted to 1:100]).
Surfaces such as floors and table tops should be cleaned regularly.
Walls, blinds, and window curtains are only cleaned when contamination is visible.
Disinfectant should be not sprayed when cleaning.
When blood or other potential infective material is spilled, contaminants should be removed immediately using a spill kit.
Used instruments should be disinfected with disinfectant before using with other patients.
Management of linen
It can be washed together with other laundry but take precautions that workers moving the laundry do not contact with the contaminated linen and do not shake the laundry.
Put into a separate bag and seal it within the room.
Wear gloves when moving linen.
Wear gloves and a gown when coming in direct contact with contaminated laundry.
Perform hand sanitation after laundry.
Management of tableware
Perform mechanical dishwashing with hot water. Washing with hands is not advisable.
NOTE
Limitations
This guideline was designed to provide recommendations by searching as many literatures as possible with a systematic literature review. However, there were not many study results which might be used as a basis for the recommendations was particularly insufficient. Therefore, this guideline may need to be revised by continuously conducting relevant studies in the future. In addition, when this guideline is applied to the individual institution, the range of applying this guideline may be dependent on the state of each institution.
Plan for revision
Up-to-date results with respect to the recommendations in this guideline will be periodically reviewed every 3 years. The guideline will be revised if there are new research results which may provide an appropriate basis for the recommendations.
Acknowledgments
The development of this guideline was supported by the Health and Medical Technology Research and Development Project of Ministry of Health and Welfare (grant number: A103001).
Notes
All the committee members who participated in the development and review of this guideline certify that the financial support did not affect the final recommendation, that no other financial support which might affect the development of this guideline was received, and that the committee members were not influenced by any particular interest group.