A case of ampullary gangliocytic paraganglioma
Article information
Abstract
Gangliocytic paragangliomas (GPs) are rare tumors of the duodenum, presenting as single sessile or pedunculated polypoid masses. Clinical manifestations of duodenal GPs can vary from an incidental finding at endoscopy to frequent upper gastrointestinal bleeding caused by mucosal ulceration and abdominal pain. GPs are considered benign, but the disease can recur and spread to regional lymph nodes. A 41-year-old female presented with abdominal pain. Upper gastrointestinal endoscopy revealed a subepithelial tumor of the ampulla of Vater in the second portion of the duodenum. The tumor was resected using the endoscopic mucosal resection technique. The tumor was diagnosed as benign GP of the duodenum using histological and immunohistochemical staining procedures.
INTRODUCTION
Gangliocytic paragangliomas (GPs) are rare and peculiar benign tumors, encountered mostly in the periampullary area of the duodenum [1,2] and much less frequently in the jejunum or third part of the duodenum [3]. Some studies have reported that approximately 90% of GPs are found in the second part of the duodenum, from where the tumor can invade the ampulla of Vater (AOV) [4]. GPs of the duodenum may present as incidental endoscopic and radiologic findings or as gastrointestinal bleeding due to ulceration of the overlying mucosa. Gastrointestinal bleeding is the most common clinical presentation, followed by abdominal pain and anemia [5]. We present the case of a 41-year-old female with GP of the duodenum, along with the clinical data, histology, and immunohistochemical staining results that correlated well with previously reported characteristics of duodenal GPs.
CASE REPORT
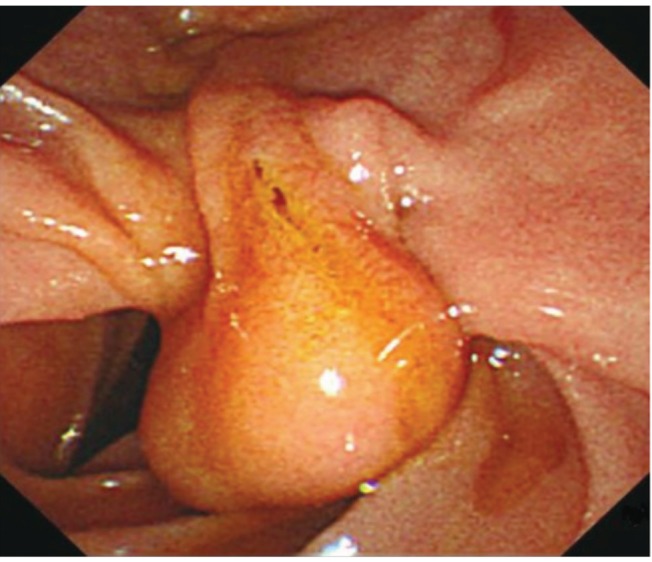
A 41-year-old female was admitted due to a history of abdominal pain. On admission, the patient had no gastrointestinal symptoms. She had no significant past history or family history. Routine hematologic, biochemical, and tumor marker tests were all normal. Contrast-enhanced computed tomography (CT) revealed a well-defined, enhancing, 2-cm, oval-shaped mass in the second portion of the duodenum, adjacent to the AOV. The biliary tree was not dilated. Magnetic resonance cholangiopancreatography showed a well-defined, 2-cm, oval-shaped subtle T2 hyperintense lesion in the second portion of the duodenum, adjacent to the AOV, as well as a normal common bile duct. Upper gastrointestinal endoscopy revealed a 2-cm subepithelial tumor in the ampullary portion of the duodenum (Fig. 1). Endoscopic ultrasonography showed a hypoechoic mass confined to the submucosal layer. Needle cutting was performed, followed by deep subepithelial forceps biopsy. Histopathology revealed spindle cells, ganglion-like cells, and epithelioid cells in the submucosal layer of the duodenum (Fig. 2). This case showed characteristic histologic features of a tumor composed of three cell types (epithelioid, spindle, and ganglion), which classified the tumor as a GP. Immunohistochemical staining for the S-100 protein revealed strong positive reactions in the spindle cells. The epithelioid and ganglion-like cells both expressed synaptophysin (Fig. 3). The immunohistochemical results confirmed the diagnosis of GP. The tumor was resected using endoscopic mucosal resection (EMR) (Fig. 4). Histology showed a well-demarcated lesion in the submucosal layer of the duodenum (Fig. 5). No distant metastasis was evident on positron emission tomography-CT. A follow-up upper gastrointestinal endoscopy performed 2 months later revealed scar formation in the resection site with convergence of the surrounding folds. The patient remains well with no tumor recurrence 6 months after the EMR procedure.

Histology showing the tumor consisted of spindle cells, ganglion-like cells (arrow, A), and epithelioid cells (B). The epithelioid cells are arranged in nests of ribbon-like structures (arrow, B) (H&E, ×200).

Immunohistochemical stains for S-100 protein revealed strong positive reaction in the spindle cells (A). Epithelioid cells and ganglion-like cells (arrow) expressed synaptophysin (B) (HRP-multimer, ×100).

Endoscopic image of the resected tumor's base with plastic stent inserted after endoscopic mucosal resection.
DISCUSSION
Various theories of the pathogenesis of duodenal GPs have been proposed, but the histogenesis of these tumors is uncertain. A GP is known as a "10% tumor," based on the frequency of the inherited forms of the disease [6]. Approximately 30% of GPs show 10 types of susceptibility gene ("10-gene tumor") [7]. No known theory has yet explained the histogenesis and pathogenesis of GP. Advances in the genetic studies of paragangliomas will have important consequences for the monitoring of patients, from genetic counseling to personalized clinical management.
Typical histologic patterns of GP include an admixture of ganglion-like cells, carcinoid tumor-like areas, and spindle cell proliferation. Immunoreactivity to neuroendocrine markers in both epithelioid and ganglion cells has been reported extensively. Immunohistochemical staining of this tumor showed a strong positive reaction for the S-100 protein in the spindle cells, while the epithelioid and ganglion-like cells expressed synaptophysin (Fig. 5). Several authors have reported that the epithelioid and ganglion cells are positive for neuroendocrine peptides, such as somatostatin, pancreatic peptide, and serotonin.
The age of patients with duodenal GPs ranges from 15 to 80 years. The incidence of GPs is slightly higher in males than in females (1.8:1), and the mean age of appearance is 54 years (range, 17 to 83). GP is well defined by ultrasonography and is visualized as a hypoechoic mass. GPs are considered benign even though they occasionally involve the regional lymph nodes and display distant metastasis or tumor recurrence, features suggestive of malignancy [1,8]. The characteristic ulceration and bleeding of the overlying mucosa lead to the usual clinical manifestations of melena and sometimes massive hematemesis and unexplained anemia [9]. Approximately 50% of patients seek medical attention for gastrointestinal bleeding, but this case did not have a history of gastrointestinal bleeding episodes [10]. Duodenal GPs are larger than 1.5 cm in at least one dimension and tend to be ulcerated and to bleed. Obstructive jaundice is less common in ampullary GP, but obstructive jaundice due to paragangliomas has been reported.
The majority of reported duodenal GP cases have been benign in nature, and simple excision of the tumor is deemed sufficient. The EMR procedure is safe and easy to perform, because the tumor protrudes into the duodenum. When endoscopic resection is not possible, surgical resection is indicated, and when regional lymph nodes are positive for metastasis, pancreaticoduodenectomy followed by local radiotheraphy is recommended. Because the possibilities of recurrence and metastasis cannot be excluded completely, decisions on the treatment method to use must be made after careful preoperative staging of the disease prior to local treatment. Furthermore, continuous follow up at the outpatient department for early detection of recurrence is necessary.
Notes
No potential conflict of interest relevant to this article was reported.