Extramedullary relapse of multiple myeloma presenting as massive upper gastrointestinal bleeding: a rare complication
Article information
To the Editor,
Multiple myeloma (MM) is a malignant disease of terminally differentiated B cells presenting with bone lesions, renal failure, infections, anemia, hypercalcemia, and hyperviscosity syndrome. The malignant plasma cells are usually confined to the bone marrow in MM. Extramedullary plasmacytoma (EMP) accounts for 4% of all plasma cell malignancies. EMP mainly occurs in the respiratory tract (82.2%), with gastrointestinal (GI) tract involvement in less than 5% of all EMP cases. The small bowel is the most common site of GI involvement, followed by the stomach, colon, and esophagus [1]. Here, we report a 69-year-old patient, admitted to hospital with hematemesis and melena, and finally diagnosed with massive upper GI bleeding caused by gastric plasmacytoma.
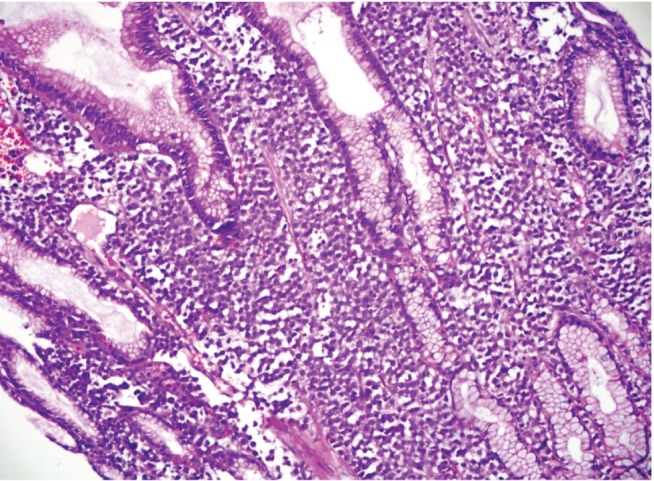
A 69-year-old male presented at the Emergency Unit with hematemesis and melena. He was known to have a history of MM and had previously been treated with vincristine, doxorubicin, and dexamethasone therapy with a very good partial response. The patient underwent emergent esophagogastroduodenoscopy. There was fresh blood in the lumen, oozing from an ulcerated, multilobulated mass 3 × 3 cm in diameter occupying the greater curvature of the proximal corpus (Forrest 1B). In addition, there were many separated polypoid, ulcerated masses about 1 cm in diameter in the body of the stomach (Fig. 1). The bleeding was successfully ablated with adrenaline injection and heater probe cautery. The patient was treated with intravenous fluids, proton pump inhibitors, erythrocytes, and fresh frozen plasma suspensions in the intensive care unit. A repeat endoscopy was performed 48 hours later, which revealed the previously identified gastric masses without evidence of bleeding. Biopsies were obtained from the lesions. The pathology specimens showed diffuse atypical plasma cell infiltration with prominent staining for CD38 and lambda immunostains leading to a pathological diagnosis of plasmacytoma (Figs. 2 and 3).
Extramedullary involvement, particularly involvement of the GI tract, is rare in MM. Most patients with gastric plasmacytomas are elderly and often present with nonspecific GI symptoms, including anorexia, weight loss, abdominal pain, vomiting, and rarely GI bleeding, usually from an ulcerated lesion. Intestinal obstruction or malabsorption may be the presenting symptom in patients with colonic or small bowel involvement [2]. On endoscopy, gastric plasmacytomas present as nodular ulcerated masses and occasionally irregular thickened gastric folds that can mimic gastrointestinal stromal tumor, lymphoma, or carcinoma [3]. The diagnosis is based on morphology and immunohistochemical demonstration of monoclonal kappa and lambda light chains or heavy chains found in plasma cells [4]. Although the treatment of EMP has not been standardized, managing mass-related local complications such as bleeding or bowel obstruction is critical in these patients. Surgery and irradiation with or without chemotherapy might be other treatment options [5]. Once GI involvement is present, the prognosis is very poor despite aggressive therapy. Consequently, although very rare, gastric plasmacytoma should be kept in mind in a patient with GI bleeding and atypical endoscopic lesions, especially those with a history of hematologic malignancy.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.