Importance of careful Tc-MIBI interpretation in patients with thyroid cancer and primary hyperparathyroidism
Article information
A 39-year-old woman presented to our clinic with incidentally detected hyperglycemia. Her medical history revealed no specific illness except for a previously diagnosed 2 cm sized thyroid nodule which was diagnosed benign nodular hyperplasia by ultrasound (US) guided fine-needle aspiration (FNA) biopsy for 3 years ago.
Laboratory findings show hyperglycemia, hypercalcemia, hypophosphatemia, and increased parathyroid hormone (PTH) level. So, we perform neck US and 99mTc-sestamibi scintigraphy (Tc-MIBI) forprimary hyperparathyroidism(PHPT) evaluation. Neck US showed a 2 cm ill-defined isoechoic nodule in the left thyroid that had previously existed (Fig. 1A).
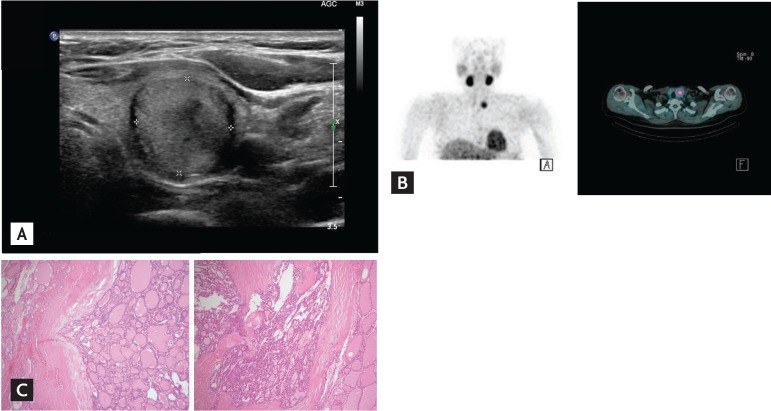
(A) Neck ultrasonography: the 1.69 × 1.70 cm, ill-defined isoechoic thyroid nodule. (B) Preoperative 99mTc-sestamibi scintigraphy scan: it shows a single lesion with strong, hot uptake in the left thyroid gland. (C) Follicular carcinoma cells are invading the capsule, and the tumor clusters are seen in the capsule (H&E, ×100).
Tc-MIBI showed a single focus of hot uptake (Fig. 1B) and pathology of the left mass after lumpectomy revealed a minimally invasive follicular thyroid carcinoma and uncorrected hypercalcemia (Fig. 1C). Follow-up Tc-MIBI showed a new increased focal uptake below the lower pole of the right thyroid (Fig. 2) which was confirmed parathyroid adenoma by reoperation. The serum PTH and calcium levels were normalized.

Postoperative 99mTc-sestamibi scintigraphy (Tc-MIBI) scan of the patient. Tc-MIBI shows a small lesion of hot uptake below the lower pole of the right thyroid gland, detected postoperatively. Yellow arrows indicate parathyroid adenoma.
Although neck US is sensitive method for neck mass evaluation, false-negative rate for thyroid FNA is still high and parathyroid tumors may be difficult to distinguish from thyroid follicular lesions, particularly when the tumor is located in the thyroid gland. While Tc-MIBI remains the most useful method for preoperatively localization of parathyroid adenoma, differentiated thyroid cancers can take-up Tc-MIBI during parathyroid imaging, resulting in a false-positive parathyroid scan. This is an important distinction given the association between PHPT and nonmedullary thyroid cancer.
However, little is known regarding the mechanistic relationship between PHPT and nonmedullary thyroid cancer, the overall incidence of thyroid malignancy with PHPT is 2% to 6%, proper diagnostic work-up with careful interpretation is essential for an accurate diagnosis in cases of coincidental presentation of a thyroid nodule and biochemical PHPT. When interpreting Tc-MIBI, the clinician should carefully consider parathyroid adenoma and thyroid cancer.
Notes
Conflict of interest: No potential conflict of interest relevant to this article was reported.