The Clinical Usefulness of Multidetector Computed Tomography of the Sacroiliac Joint for Evaluating Spondyloarthropathies
Article information
Abstract
Backgrounds
Due to the low sensitivity of plain radiography, the diagnosis of early stage ankylosing spondylitis (AS) is often difficult since many patients do not meet the radiographic criteria. The objective of our study was to investigate the diagnostic value of performing multidetector computed tomography (MDCT) of the sacroiliac (SI) joint in the evaluation of AS patients.
Methods
Thirty seven patients with definite or probable AS were evaluated. Plain radiography and MDCT imaging of the pelvis were performed for evaluating the SI joints. Two radiologists analyzed the images, and they graded the sacroiliitis on a scale of 0-4 according to the modified NY criteria. The clinical variables we analyzed included the disease duration, the treatment duration, the prescribed drugs, peripheral joint involvement, enthesopathy, the functional limitations and the BASDAI..
Results
MDCT detected more bilateral sacroiliitis as compared to the plain radiography (86.5% vs. 75.7%, respectively), and MDCT yielded a higher grade of disease in 32.4% (right SI joint) and 24.3% (left SI joint) of the patients. More patients satisfied the modified NY criteria with using MDCT as compared with that when using the plain radiography (81.1% vs. 54.1%, respectively, p=0.002).
Conclusions
Visualization of the sacroiliac joint by MDCT provided a better diagnosis of AS, and especially during the early stage of the disease.
INTRODUCTION
The diagnosis of ankylosing spondylitis (AS) is based on the modified New York (NY) criteria. The radiographic requirement of this set of criteria includes unilateral grade 3 or 4 sacroiliitis, or bilateral grade 2 to 4 sacroiliitis according to the plain radiography1). However, it is often difficult to diagnose AS in the early stage of the disease since many patients do not fulfill the radiographic criteria. This is due to the low sensitivity of evaluating the sacroiliac (SI) joint with using plain radiography, and especially at the early stage of the disease2, 3). In addition, grading the SI joint may vary between differnt observers since the SI joint lies oblique to the vertical plane, which often obscures a clear view of the SI joint on plain radiography4, 5). Several diagnostic modalities such as magnetic resonance imaging (MRI), computed tomography (CT) and scintigraphy have been suggested to overcome the limitations of plain radiography6-9). Although MRI is superior to the other modalities for detecting early bony changes, its application is limited by the high cost of this modality and the lengthy evaluation time10-12).
CT has also been applied for evaluating the SI joint. Although CT displays superiority over plain radiography as CT shows a more detailed image, the previous studies concerned with the diagnosis of sacroiliitis via CT have demonstrated controversial results. A few studies have shown the higher efficacy of CT over plain radiography4, 8), but other studies have reported similar efficacy by both modalities13). Since the time that these studies were reported, no other noteworthy CT studies concerned with AS have been performed. However, with the recent introduction of multidetector CT (MDCT), the diagnostic application of CT is expanding since MDCT provides better images in a short acquisition time. Therefore, application of MDCT for evaluating the SI joint is worth reconsideration. We performed the present study to evaluate the diagnostic value of MDCT for the SI joint in the evaluation of AS. We found that visualization of the sacroiliac joint by MDCT provided a better diagnosis of AS, and especially during the early stage of this disease.
MATERIALS AND METHODS
Patients and clinical assessment
We enrolled 37 patients with definite and probable AS, and these patients were seen and treated at Ewha Womans University Medical Center. The diagnosis of AS was based on the modified NY criteria. Those patients with probable AS didn't satisfy the radiologic criteria, but they fulfilled the clinical criteria. The clinical assessment included age, gender, the duration of disease, the duration of treatment, the treatment drugs, spine involvement, peripheral joint involvement, enthesopathy, uveitis, the Shober test, chest expansion, the mean ESR and CRP levels during the treatment, the HLA-B27 level and the BASDAI (Bath Ankylosing Spondylitis Disease Activity Index). The duration of disease was defined as the time between the first symptom of back disease and the radiographic evaluation.
Radiological assessment
Both plain radiography and MDCT (Sensation 16; Siemens Medical System, Erlangen, Germany) of the SI joints were performed withn 20 days. Each patient underwent anteroposterior (AP) radiography of the SI joints in the supine position with a 20 caudal tube angle. The SI joint radiographs were graded according to the modified NY criteria1): grade 0: normal, grade 1: changes suggestive of sacroiliitis, grade 2: minimal abnormality with small localized areas of erosion or sclerosis, and without alteration of the joint width, grade 3: definite abnormality with erosions, sclerosis, joint space widening or narrowing, or partial ankylosis, grade 4: complete ankylosis (Figure 1A). MDCT was performed without contrast enhancement and its parameters were as follows: 150 mA, 120 kVp, a 0.5-sec tube rotation speed and a beam pitch of 1. The transverse and coronal MPR (multiplanar reconstruction) MDCT images were obtained with a slice thickness of 3 or 5 mm and using a bone reconstruction algorithm. The MDCT images were analyzed by using the same grading system as was used for the plain radiography (Figure 1B). Two musculoskeletal radiologists independently reviewed the images without having any knowledge of the clinical information. Each set of images was reviewed again by each observer after 1 week.
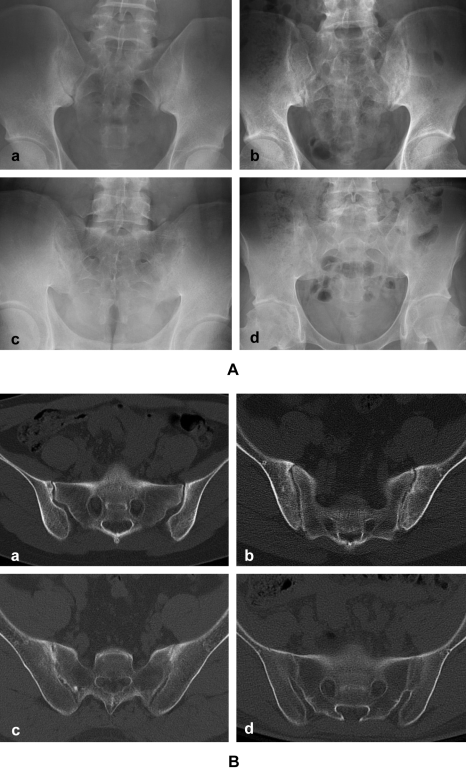
Grading of the SI joint in AS patients is shown on the AP view of the plain radiography (A) and on the axial image by CT (B). (a) grade 1 that is suggestive of sacroiliitis, (b) grade 2 with minimal abnormality along with small localized areas of erosion or sclerosis without alteration in the joint width, (c) grade 3 shows definite abnormality with erosions, sclerosis, joint space widening or narrowing, or partial ankylosis, (d) grade 4 shows complete ankylosis.
Statistical analysis
The clinical parameters are presented as means±SDs. The reliability of the radiologic assessment and the intra- and inter-observer agreement were evaluated by using Cronbach's alpha test and the kappa test. Comparisons of the clinical parameters and the radiologic grade of sacroiliitis between the plain radiographs and the CT scans were analyzed with using χ2-testing and ANOVA testing. The agreement between the 2 imaging modalities was evaluated with using the kappa test. Statistical analysis was performed using SPSS 12.0 (SPSS Inc, Chicago, IL) software. A p level < 0.05 was considered as a significant difference.
RESULTS
Patients characteristics
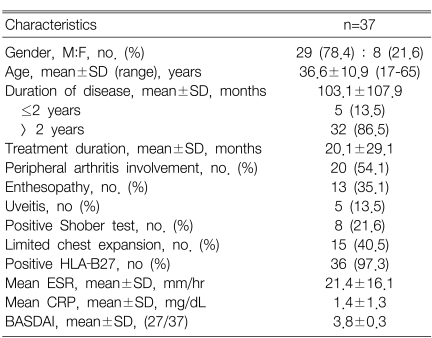
Twenty nine (78.4%) of the 37 AS patients were male with a mean age SD of 36.6±12.1 years (age range: 17-65). The mean disease duration was 103.1 months. Five (13.5%) patients were at an early stage of disease, which was defined as a disease duration of less than 2 years. The mean treatment duration was 21.2 months. Thirty six (97.3%) of the patients were positive for HLA-B27. Twenty (54.1%) of the patients had peripheral arthritis. Limitation of chest expansion was observed in 15 patients (40.5%). The mean ESR and CRP levels during the treatment were 21.4 mm/hr and 1.4 mg/dL, respectively. The BASDAI was evaluated for 27 patients, and the mean value was 3.8 (Table 1).
Radiological findings
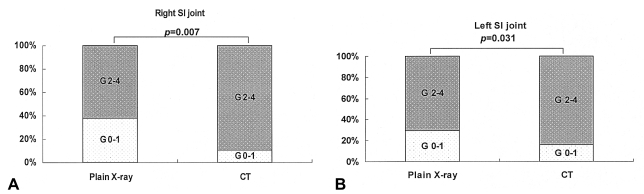
The intra-observer agreements between the plain radiographs and the MDCT images were good with value of >0.9. The inter-observer agreements were moderately good with a value of >0.5 (p=0.000) for the plain radiographs and >0.4 (p=0.000) for the MDCT image. When there was inter-observer disagreement for the grading, a consensus was reached through a discussion between the radiologists. Grading of the SI joints between the plain radiography and the MDCT showed moderately high agreement (κ=0.454 for the right SI joint, κ=0.612 for the left SI joint) (Table 2). MDCT detected a higher grade of right sacroiliitis in 11 (32.4%) patients who had a grade of 0-1 according to their plain radiography. Similarly, the left sacroiliitis in 9 (24.3%) patients showed a higher grade according to the MDCT than that of the plain radiography. 4 (10.8%) of the patients had a lower grade of right sacroiliitis according to CT, and left sacroiliitis was detected in 2 patients (5.4%) according to the CT as compared to the plain radiography. MDCT detected more bilateral sacroiliitis as compared to that detected via plain radiography, although this was not statistically significant (86.5% vs. 75.7%, respectively, p=0.081). The proportion of patients fulfilling the radiographic criteria of the modified New York criteria was significantly higher for the MDCT images as compared to using the plain radiography (81.1% vs. 54.1%, respectively, p=0.002) (Table 3). There were 10 (27%) patients who did not satisfy the modified NY criteria when using the plain radiography, but they did fulfill the criteria when they were imaged via MDCT. For the details, the sacroiliitis that was graded 0 or 1 by plain radiography was graded 2 or more by the MDCT (Table 3). High grades of 2-4 for the right sacroiliitis were observed more often by employing MDCT than by employing plain radiography (p=0.007), and this was also true for the (p=0.031) (Figure 2).
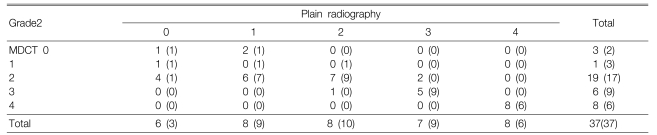
Comparison of the radiographic grade of sacroiliitis according to plain radiography and MDCT1. [Number of patients with right (left) sacroiliitis]
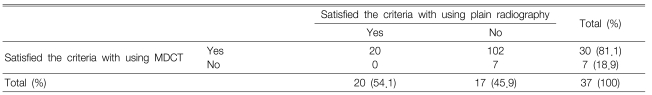
Analysis of patients satisfying the radiographic criteria of the modified NY criteria for diagnosing AS by plain radiography and MDCT [n=37]1
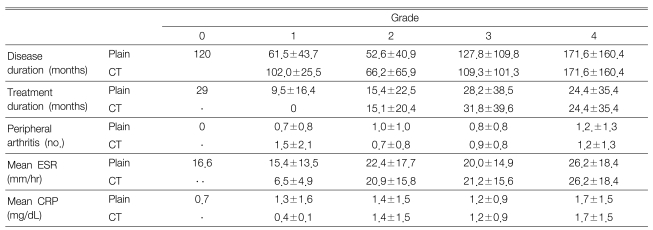
Comparison of the clinical parameters and the grade of the sacroiliitis
The clinical parameters failed to show significant correlation with the sacroiliitis grade. Although it was statistically not significant, the correlation between the disease duration and the radiologic grade showed a linear trend curve, and especially for the grades 3 and 4 sacroiliitis (Table 4).
DISCUSSION
A more accurate and sensitive technique for imaging the SI joint is required for making the diagnosis of AS, and especially during the early phase of the disease. We have applied MDCT for evaluating the SI joint in AS patients, and we found that MDCT showed benefit over plain radiography for detecting early sacroiliitis. MDCT was able to detect abnormalities in the normal or suspicious lesions that were found on plain radiography, and MDCT yielded higher grades of sacroiliitis compared to the plain radiography. This finding was consistent with other previous CT studies that focused on early AS, that is, CT was able to detect sacroiliitis more accurately in 56.7% of the cases, and using CT resulted in obtaining a higher AS grade in 71.4% of the cases, as compared to the AS grade obtained with using plain radiography8, 14). We found that the ability of MDCT to diagnose AS was higher compared to that with using the plain radiography (81.1% vs. 54.1%, respectively). In our study, this ability of CT to evaluate the SI joint was higher than that of the previous reports (38% to 75%)14, 15). This was certainly due to the merits of MDCT. The two-dimensional detector array of MDCT permits CT scanners to acquire multiple slices or sections simultaneously, and it greatly increases the speed of CT image acquisition. As a result, we were able to diagnose AS with using MDCT in 10 out of the 37 patients who did not meet the radiographic criteria of the modified NY criteria when using plain radiography. Moreover, MDCT was able to more frequently detect bilateral sacroiliitis, which is a more common feature of sacroiliitis in AS as compared to the other seronegative spondyloarthrophathies16, 17). The high sensitivity of MDCT that was noted in our study provides evidence for applying MDCT during the initial evaluation of AS.
CT is known to be superior for detecting such bony changes as cortical erosion, subchondral sclerosis and ankylosis, as compared to MRI or plain radiography10). When we analyzed the distribution of the sacroiliitis grades in detail, we found that MDCT detected the grade 2 and 3 lesions with more sensitively than did the plain radiography. A previous study on healthy controls reported the possibility that sclerosis and ankylosis were over-diagnosed by CT because of the normal aging process, which results in joint space narrowing and erosions18, 19). Even though we did not perform direct comparison between age and gender matched healthy controls and the patients, we found that age and the grades according to MDCT did not show significant correlation (p=0.227: the data is not shown), suggesting that this is not a confounding factor in this study. The plain radiography overestimated the sacroiliitis grades over MDCT in less than 4 cases. Grades 1, 2 and 3 according to the plain radiography were read as grades 0, 1 and 2 according to MDCT. This may be due to the fact that individual variations exist in the alignment of the SI joints. The diseased SI joints might have been positioned more parallel to the coronal plane than were the normal SI joint, and this probably resulted in obscuring the SI joint space that can be read as partial ankylosis. The direction of the beam may also cause overestimation by plain radiography.
We found that the clinical parameters did not correlate with the changes of the radiologic grades by both plain radiography and MDCT in the AS patients. It is generally accepted that clinical symptoms can not predict the radiographically determined damage in AS patients. However, Muche et al. have suggested there was positive correlation between the disease duration and the sacroiliitis grade according to MRI17). We also found a trend toward positive correlation between the disease duration and the sacroiliitis grades 2 to 4. We could not find any correlation between the mean ESR and CRP levels and the radiologic grade. Spoorenberg et al. also reported that the degree of inflammation can not explain the destruction of the SI joints20). The other clinical parameters, including peripheral arthritis, spinal involvement, enthesopathy, uveitis, the Shober test and limited chest expansion also did not show correlation with the sacroiliitis grade, suggesting that the radiological severity of sacroiliitis cannot be predicted by the clinical activity and the functional status of the patients.
In conclusion, visualization of the sacroiliac joint by MDCT provided a better diagnosis of AS, and especially during the early stage of disease. MDCT of the SI joints can be used to for correctly diagnosing AS, and performing MDCT can help arrive at a higher grade of this disease, and this is especially true when the diagnosis of sacroiliitis is ambiguous according to plain radiography. Moreover, MDCT can provide better imaging of the SI joint abnormalities.