Facility characteristics as independent prognostic factors of nursing home-acquired pneumonia
Article information
Abstract
Background/Aims:
Recently, the incidence of nursing home-acquired pneumonia (NHAP) has been increasing and is now the leading cause of death among nursing home residents. This study was performed to identify risk factors associated with NHAP mortality, focusing on facility characteristics.
Methods:
Data on all patients ≥ 70 years of age admitted with newly diagnosed pneumonia were reviewed. To compare the quality of care in nursing facilities, the following three groups were defined: patients who acquired pneumonia in the community, care homes, and care hospitals. In these patients, 90-day mortality was compared.
Results:
Survival analyses were performed in 282 patients with pneumonia. In the analyses, 90-day mortality was higher in patients in care homes (12.2%, 40.3%, and 19.6% in community, care homes, and care hospitals, respectively). Among the 118 NHAP patients, residence in a care home, structural lung diseases, treatment with inappropriate antimicrobial agents for accompanying infections, and a high pneumonia severity index score were risk factors associated with higher 90-day mortality. However, infection by potentially drug-resistant pathogens was not important.
Conclusions:
Unfavorable institutional factors in care homes are important prognostic factors for NHAP.
INTRODUCTION
The incidence of nursing home-acquired pneumonia (NHAP) is increasing, and it is now the leading cause of death among nursing home residents in Korea [1]. In the USA, the total number of cases of NHAP will approach 1.9 million episodes per year by 2030 [2], and the mortality rate in these patients is generally high, ranging from 13% to 41% [3].
Despite its high mortality rate, NHAP remains somewhat undefined. In the 2005 American Thoracic Society/Infectious Diseases Society of America (ATS/IDSA) guidelines, NHAP was included in healthcare-associated pneumonia (HCAP) and considered to be a type of nosocomial pneumonia [4]. The definition of the term “nursing home” in NHAP is also vague. Although nursing home patients are generally defined as severely disabled elderly patients, the type of care provided by nursing homes is not specified [5,6]. Although some studies indicated that medical staff size and physician presence on-site are associated with decreased hospitalization rates in acute care centers [7,8], few studies have examined outcomes after hospitalization. As the environment varies considerably among studies, the most effective antimicrobial treatments for NHAP remain controversial [5,6,9-11].
There are two types of long-term care facility (LTCF) in Korea: care homes ([yoyangwon] in Korean) and care hospitals ([yoyangbyeongwon] in Korean). Care homes resemble assisted living facilities or intermediate care facilities, while care hospitals resemble skilled nursing facilities in the USA. Care homes are under the control of Long-Term Care Insurance for the Elderly (i.e., national insurance for seniors’ welfare) and should be staffed by registered nurses (1 per 25 residents), physical therapists (1 per 100 residents), and social workers (1 per 100 residents), but not by physicians, who instead visit periodically. Care hospitals are under the control of the National Health Insurance system. Licensed physicians (1 per 40 residents) should supervise the care of each patient, and a nurse (one per six residents) or other medical professional is almost always on the premises.
In this study, we examined the clinical, microbiological, and institutional factors associated with risk of NHAP mortality.
METHODS
Data collection
Data on all patients ≥ 70 years of age admitted with newly diagnosed pneumonia between January 2009 and December 2010 were retrospectively reviewed from the medical record database at Myongji Hospital, a community hospital in Goyang, Korea.
In all patients, pneumonia or other accompanying infections (e.g., urinary tract infection [UTI]) were diagnosed as reported previously [12]. Emergency department physicians and pulmonologists decided whether to hospitalize the patients. To exclude overt hospital-acquired pneumonia (HAP), patients with any current malignancy, end-stage renal disease undergoing renal replacement therapy, or advanced liver cirrhosis were excluded from the study. Patients with HCAP in the community were also excluded. Data of patients with “do not resuscitate” orders were not analyzed.
The protocol was approved by the Ethics Review Committee and the Institutional Review Board of Kwandong University Myongji Hospital (IRB No. 11-020).
Microbiological studies
Respiratory samples, including sputa and bronchial aspirates, were collected via endotracheal suction or bronchoscopy within 48 hours of hospitalization. To minimize possible bias due to incomplete sampling or contamination from the oral cavity, the predominance of cultured organisms was also reported in comparison with α-hemolytic viridans group of streptococcus, representing part of the normal flora. Organisms more prominent than α streptococcus in adequate specimens were defined as pneumonia pathogens. Samples of most patients’ blood and urine were cultured, and a urinary antigen test for Streptococcus pneumoniae was performed in most patients. However, investigations for Mycoplasma pneumoniae, Legionella pneumophila, and viruses were not performed in most patients.
Potentially drug-resistant pathogens (DRPs) were defined as those multidrug-resistant [13] or resistant to antibiotics used for CAP, such as Pseudomonas aeruginosa and Acinetobacter spp. In some patients, DRPs were cultured after empirical treatment with antimicrobial agents that did not cover these organisms. In these cases, the treatment was designated as “inappropriate.”
Classification of patients according to quality of care
CAP was defined as a diagnosis of pneumonia in patients who did not meet any of the criteria for HCAP. Hospitalized patients with CAP were considered as the current standard group, and were compared to patients with NHAP. To compare the quality of care in nursing facilities, patients with NHAP were classified into two groups. Thus, the following three groups were defined: patients who acquired pneumonia in (A) the community, (B) care homes, and (C) care hospitals.
Statistical analysis
The independent-samples t test (Mann-Whitney U test for nonparametric variables) was used for comparisons of continuous variables. The chi-square test (or Fisher exact test) and binary logistic regression were used for univariate and multivariate analyses, respectively, of categorical data.
The Kaplan-Meier method was used to compare 90-day mortality among the three groups, and mortality rates were assessed by log-rank test. Further risks were estimated using Cox proportional hazards models. Potential predictors for multivariate modeling were selected by univariate analyses and subsequently entered in a stepwise forward-conditional manner with entry and retention in the model set at a significance level of 0.05. All analyses were performed using the SPSS version 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Baseline characteristics
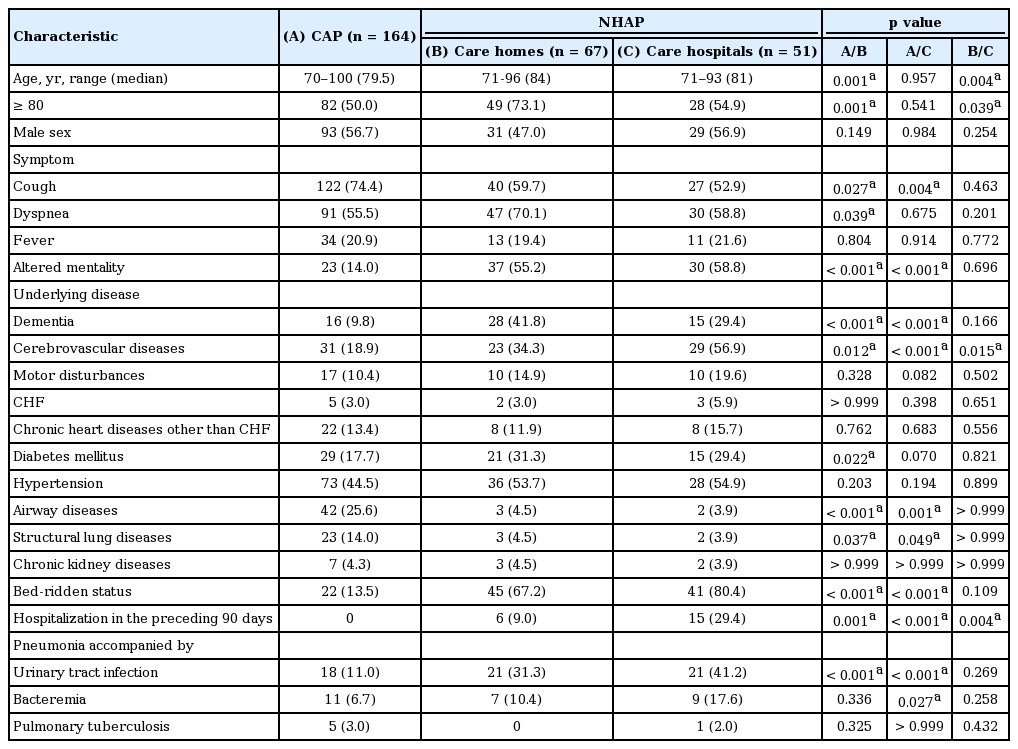
Medical records of 989 pneumonia patients ≥ 70 years of age were reviewed, and 707 patients were excluded from the analysis because they had overt HAP, malignancy, end-stage renal disease, or advanced liver cirrhosis (Fig. 1). Data were collected for 282 patients; 164 of these patients contracted pneumonia in community settings, while the remaining 118 cases were considered NHAP (67 patients contracted pneumonia in care homes, and 51 in care hospitals) (Table 1).
A greater proportion of patients ≥ 80 years of age resided in care homes (n = 49, 73.1%) than in the community (n = 82, 50.0%) or in care hospitals (n = 28, 54.9%). Respiratory symptoms, such as cough and dyspnea, were frequently found in patients with CAP, and acute altered mental status was more frequent in patients with NHAP. Dementia and cerebrovascular diseases were common in patients with NHAP, and more than 60% of NHAP patients were bed-ridden (67.2% of patients in care homes, and 80.4% of those in care hospitals). However, airway or structural lung diseases were more frequent in patients with CAP. More NHAP patients in care hospitals (n = 15, 29.4%) had a history of hospitalization within the preceding 90 days compared with NHAP patients in care homes (n = 6, 9.0%). In NHAP patients, pneumonia accompanied by UTI was common. Whereas 11.0% of CAP patients had a UTI, 31.3% in care homes and 41.2% in care hospitals had pneumonia accompanied by a UTI. The same pathogens were discovered in respiratory and urinary tracts in only six patients (10.0% of 60 pneumonia patients with UTI).
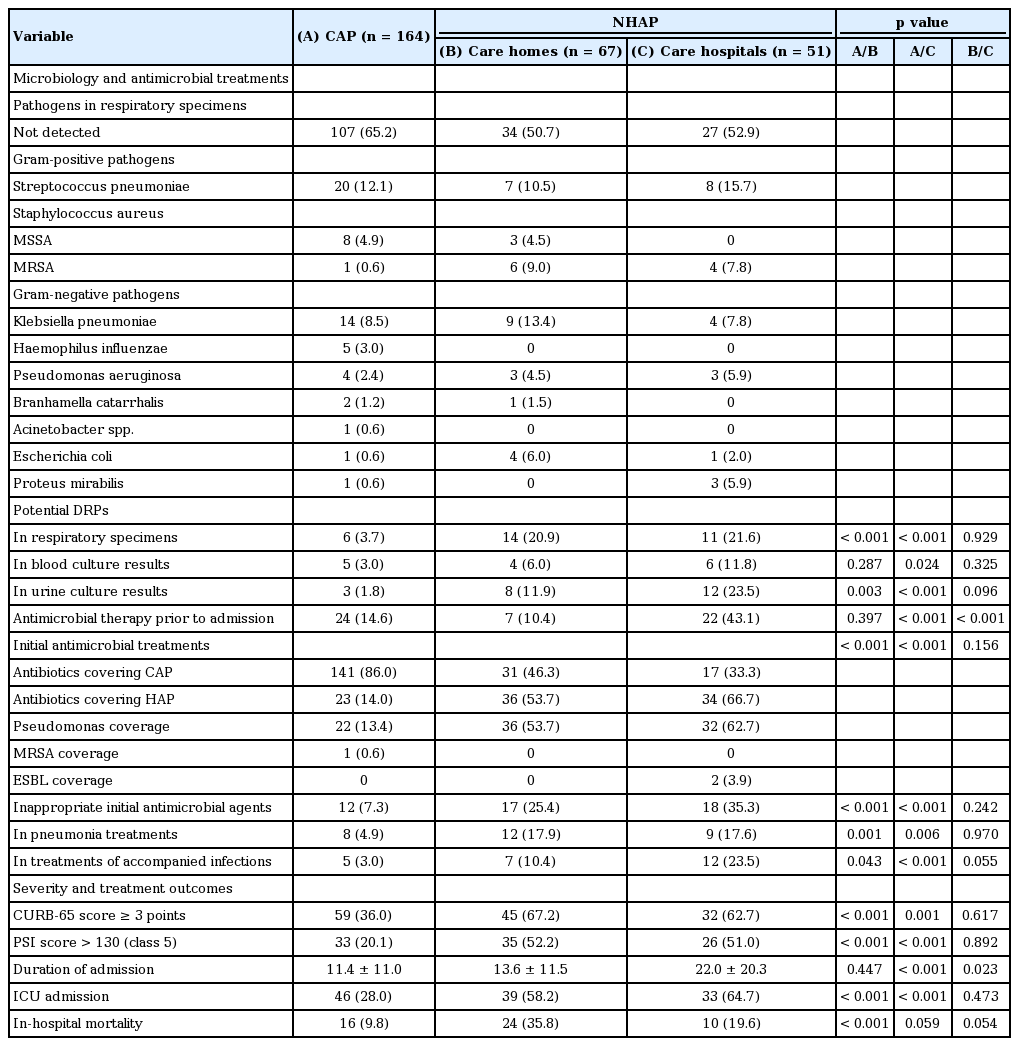
Comparison of microbiology results and antimicrobial treatments
Pathogens were detected in respiratory specimens from less than half of the patients (Table 2). In each group, S. pneumoniae was the most frequent pathogen. More DRPs were detected in patients with NHAP than CAP, but the prevalence of pneumonia caused by DRPs did not differ between patients in care homes and those in care hospitals (p = 0.929). Whereas 23 CAP patients (12.8%) were treated with antimicrobial agents for HAP according to ATS/IDSA guidelines for HAP, a greater proportion of NHAP patients were treated with these agents: 36 patients (53.7%) in care homes and 34 (66.7%) in care hospitals [4]. Initiation of inappropriate antibiotics was more frequent in patients with NHAP. Seventeen patients (25.4%) in care homes and 18 (35.3%) in care hospitals were initially treated with antimicrobial agents inappropriate for pneumonia or other accompanying infections (UTI and bacteremia). Although antimicrobial treatments did not differ between patients in care homes and care hospitals, more patients in care hospitals seemed to be treated inappropriately for accompanying infections, although this difference was not statistically significant (10.4% vs. 23.5%, respectively; p = 0.055).
Severity and treatment outcomes
NHAP was more severe than CAP (Table 2). More NHAP patients than CAP patients had CRRB-65 (confusion, urea, respiratory rate and blood pressure) scores ≥ 3 points and pneumonia severity index (PSI) scores > 130 (class 5). The rates of admission to Intensive Care Units and in-hospital mortality were also higher in patients with NHAP. Most parameters associated with severity and treatment outcomes did not differ between patients in care homes and those in care hospitals, but the duration of admission was longer in pneumonia patients residing in care hospitals (13.6 ± 11.5 vs. 22.0 ± 20.3, respectively; p = 0.023). There was no difference in the in-hospital mortality rate between patients in care homes and care hospitals (35.8% vs. 19.6%, respectively; p = 0.054).
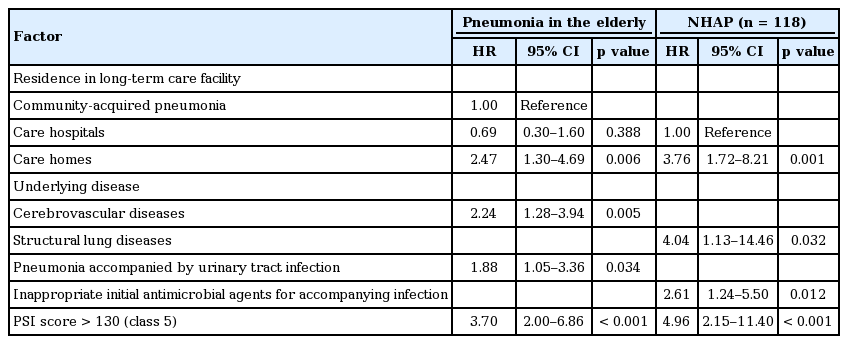
In univariate log-rank tests, 90-day mortality was higher in patients in care homes (Fig. 2). Although there was no difference in mortality between CAP (12.2%) and NHAP patients in care hospitals (p = 0.126), the patient mortality rate was higher in care homes (40.3%) than in either the community (12.2%; p < 0.001) or in care hospitals (19.6%; p = 0.011). Risk factors for 90-day mortality are presented in Table 3. When all patients were included in the analysis, residence in a care home (adjusted hazard ratio [HR], 2.47; 95% confidence interval [CI], 1.30 to 4.69), cerebrovascular disease (adjusted HR, 2.24; 95% CI, 1.28 to 3.94), and pneumonia accompanied by a UTI (adjusted HR, 1.88; 95% CI, 1.05 to 3.36), but not age, were risk factors for mortality. Within the 118 NHAP patients, residence in a care home (adjusted HR, 3.76; 95% CI, 1.72 to 8.21), structural lung diseases (adjusted HR, 4.04; 95% CI, 1.13 to 14.46), and treatment with inappropriate antimicrobial agents for accompanying infections (adjusted HR, 2.61; 95% CI, 1.24 to 5.50) were risk factors. In both analyses, residence in a care home and a high PSI score, but not DRP infection, were factors significantly associated with 90-day mortality.
The 90-day survival results of pneumonia patients by log-rank test. (A) All patients. (B) Patients < 80 years of age. (C) Patients ≥ 80 years of age.
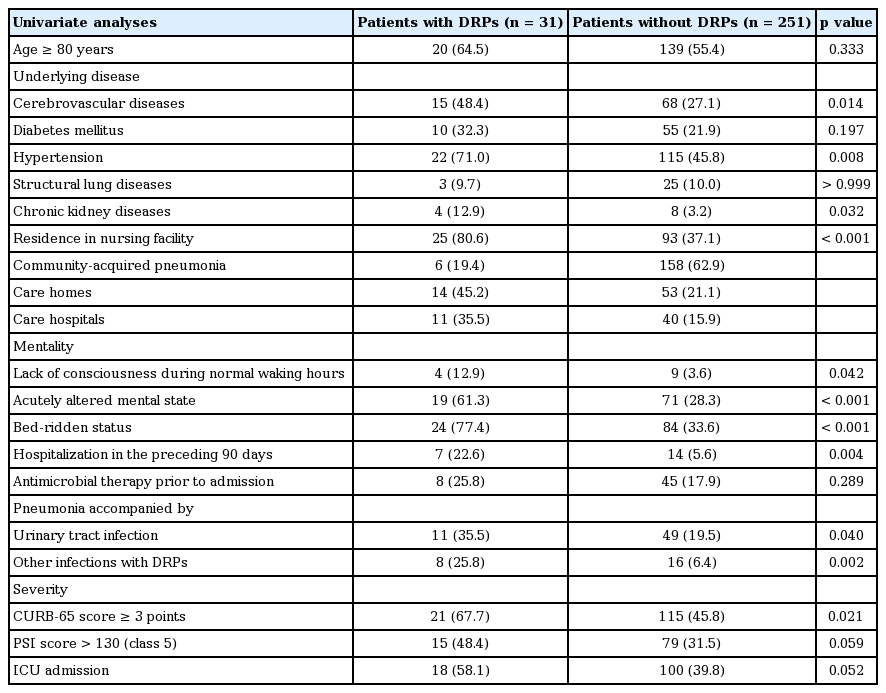
Risk factors for infection with potentially drug-resistant pathogens
Risk factors associated with DRP infection are described in Table 4. In univariate analyses, residence in a nursing facility was an important factor related to DRP infection (p < 0.001). Cerebrovascular diseases (p = 0.014) and chronic kidney diseases (p = 0.032) were also important factors. Lack of consciousness during normal waking hours (p = 0.042), acutely altered mental state (p < 0.001), bed-ridden status (p < 0.001), and prior hospitalization (p = 0.004) were common in patients infected with DRPs. The risk of pneumonia caused by DRPs was higher when accompanied by UTI (p = 0.040) or other infections with DRPs (p = 0.002). Pneumonia caused by DRPs was more severe than that caused by drug-susceptible pathogens (p = 0.021). In multivariate analysis, the presence of chronic kidney diseases (adjusted odds ratio [OR], 4.30; 95% CI, 1.08 to 17.05; p = 0.038) and bed-ridden status (adjusted OR, 6.68; 95% CI, 2.74 to 16.26; p < 0.001) were significantly associated with DRP infection.
DISCUSSION
The most important finding of this study was that residence in a care home was an independent risk factor for 90-day mortality in NHAP, and that facility characteristics had a greater influence on mortality risk than microbiological factors.
Many recent studies have examined the relationship between prognosis of NHAP and infection with DRPs. Although DRPs were more frequent in NHAP than CAP patients, DRP infection did not increase NHAP mortality [6,10]. This is contrary to the hypothesis that excess mortality is related to inadequate treatment for DRPs using antimicrobial treatments for CAP [6]. Some investigators have suggested that NHAP should not be treated as nosocomial pneumonia [14] and host factors such as age and comorbidity should be considered as potential risk factors for mortality [6,9]. In the present study, DRPs in respiratory specimens did not contribute significantly to the risk of mortality. Only accompanying infections, such as UTIs, and treatment with inappropriate antimicrobial agents exhibited significant associations with mortality. Further high-quality randomized controlled trials are required to determine the effects of antimicrobial treatments [2,11,14-17].
In this study, residence in a care home was an important prognostic factor for 90-day mortality. Several recent studies have revealed the prognostic importance of environmental factors. In a study of HCAP, nursing home residence was the main risk factor for mortality [18]. Several studies performed in nursing homes showed that medical staff organization, nurse turnover, and staff attitude regarding treatment guidelines were important risk factors for hospitalization in acute-care centers [19-22]. In the present study, the associations of environmental, host, clinical, and microbiological factors with mortality were analyzed simultaneously. Residence in a facility with fewer registered nurses or physical therapists, or without an on-site physician, was associated with increased 90-day mortality of NHAP. Inadequate pre-hospitalization management could explain the increased mortality rate in care home residents. Although many factors were similar in patients in care homes and care hospitals, fewer patients in care homes were treated with antibiotics. The availability of fewer registered nurses or physical therapists may result in poor oral hygiene or lack of nursing care help with activities of daily living. The clinical significance of pre-hospitalization factors remains to be determined in further studies.
This study was limited by its retrospective nature. In addition, the facility characteristics in this study may be unique to Korea. However, most studies associated with LTCFs tend to have limited value because (1) available medical resources are always limited in LTCFs and (2) long-term care systems are diverse in all countries. Another limitation of this study is that there was a paucity of data regarding nursing facilities, so reasonable interpretation of the results is difficult. As there have been no Korean studies of nursing facilities, it was impossible to consider pre-hospitalization factors. We assumed that unfavorable institutional factors, such as residence in a facility with fewer registered nurses and without a full-time physician, would be important prognostic factors for NHAP. These pre-hospitalization factors should be considered in the design of future trials to identify the optimal antimicrobial treatments.
In conclusion, unfavorable institutional factors were important prognostic factors for NHAP. However, further studies are required to understand this result.
KEY MESSAGE
1. Residence in a care home is an independent risk factor for 90-day mortality in pneumonia in the elderly, and facility characteristics had a greater influence on mortality risk than microbiological factors. However, further studies are required to interpret these results.
2. These pre-hospitalization factors should be taken into consideration in the design of future trials to identify the optimal antimicrobial treatments and outcome measurements.
Notes
No potential conflict of interest relevant to this article was reported.