Pathophysiology and Management of Irritable Bowel Syndrome
Article information
Definitions and prevalence of irritable bowel syndrome
Irritable bowel syndrome (IBS) is a chronic relapsing disorder of the gastrointestinal function, the main features of which are abdominal pain or discomfort and an alteration of bowel habit. IBS has a complex, multifactorial etiology and is recognised as the most common disorder diagnosed by gastroenterologists; it is also very commonly encountered in primary care practice. Consequently, it has a huge socioeconomic impact on health care resources in most industrialised societies1, 2).
Definitions of IBS have continued to evolve over the last two decades, initiated by the seminal study of Manning et al3) in which several symptoms which typically cluster together in IBS were identified. These included: pain relief by defecation, more frequent stools occurring at the onset of pain, looser stools occurring at the onset of pain, visible abdominal distension, passage of rectal mucus and a sensation of incomplete evacuation after defecation. Several years ago, an international consensus definition of IBS was termed the “Rome criteria”, based largely on the Manning criteria. In the Rome classification, functional (painless) diarrhea and functional (painless) constipation were regarded as separate entities from IBS.
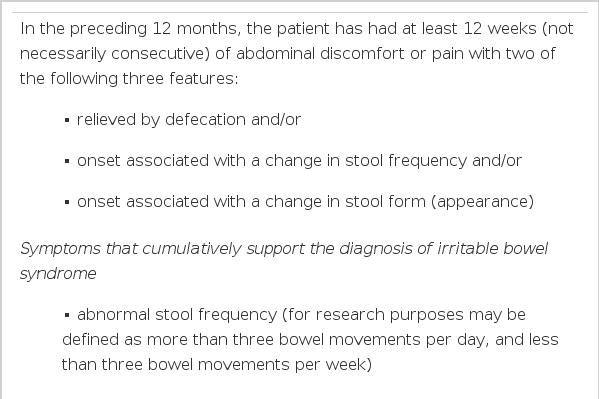
Over the last five years, the Rome criteria for IBS have become accepted as the state-of-the-art criteria for research studies. Recently, they have been refined, focusing on the essential components of abdominal pain and an altered bowel pattern (Table 1)4). Work is underway to further determine the specificity of these criteria, particularly in the light of new potential pathophysiological markers which include visceral hyperalgesia and detectable histological and immunohistochemical alterations in the small and large intestine. The importance of the Rome criteria lies in the fact that they can be used to diagnose IBS positively, in conjunction with the selective use of investigations to exclude “organic” disease.
The prevalence of IBS varies according to the diagnostic symptom criteria employed (for example, the Rome I or II criteria, the Manning criteria etc.), but ranges from about 3% in the US5) to up to 20% in population samples6): the incidence of IBS is 1–2% per year. Although the Rome II consensus does not recommend formal subgrouping of IBS according to the predominant bowel pattern, it does provide working definitions for constipation- and diarrhea-predominant subgroups, if required4). A third subgroup, so-called alternating IBS, can be recognised clinically; it is generally recognised that the above three subgroups each constitute about one-third of IBS cases. Recently, a Swedish report7) has characterised, by cluster analysis, three different subcategories of IBS - the first distinguished by hard stools, varying stool consistency and a highly disturbed stool passage; the second by loose stools and urgency; and the third by normal stools with little disturbance in stool passage, but with considerable abdominal pain and bloating. Interestingly, in this study no relationship was found between pain/bloating and bowel habit in terms of the subgrouping. Postprandial exacerbation of symptoms is common in IBS8), a factor not specifically included in the Rome criteria. Finally, extraintestinal symptoms are also common in IBS, including headache, backache, urinary and gynecological symptoms, and fatigue; these appear to be more common in the IBS-constipation subgroup.
In Western countries, women tend to present to doctors with symptoms of IBS more frequently than men, and a female-to-male ratio of up to 3:1 has been reported in some studies9, 10). The apparently higher prevalence of IBS in women is seen in all age groups and may be a reflection of the fact that women are likely to seek medical advice more often than men, although physiological differences in pain sensitivity and central responses to pain may also be important.
Pathophysiological mechanisms
Motility of the digestive tract encompasses the phenomena of contractile activity, tone, compliance and transit. Advances in the understanding of brain-gut interactions and the applied physiology of the ‘brain-gut axis’ have lead to a resurgence of interest in the pathophysiology of IBS. As stool volume is usually normal in patients with IBS, even in the IBS-diarrhea subgroup, the major mechanism underlying the symptoms appears to be enteric sensorimotor dysfunction11). Sophisticated techniques over the last few years have enabled assessment of intestinal tone and sensitivity, as well as the appreciation of external, intrinsic and local modulating factors on gut motility and sensitivity (Figure 1). Thus, various types of dysmotility have been documented repeatedly in IBS, and most likely reflect dysfunction at one or more levels of the brain-gut axis. Also, patients with IBS exhibit sensory afferent dysfunction, manifested as an altered perception to stimuli such as distension of the gut and selectively affecting the visceral territory. There remains no consensus, however, on the inter-relationships between dysmotility and hypersensitivity in IBS, although some evidence indicates that, at least postprandially, motor dysfunction is more prevalent in IBS patients with underlying visceral hypersensitivity in the basal (fasting) state12). Moreover, the considerable variability in motility and sensitivity between and within individuals, and the number of modulating factors, has made establishment of normal databases problematic.
Schematic representation of the applied physiology of digestive tract motility and sensitivity and the modulatory factors relevant to the brain-gut axis.
1. Enteric sensorimotor dysfunction in IBS
Although there is an extensive literature on gastrointestinal motility in patients with IBS, accrued over many years, it is only during the last fifteen years that more definitive characterisation of altered motor patterns in IBS has been obtained11). Most studies utilising the more invasive measurement techniques, particularly the earlier studies, have been undertaken in the colon (especially the distal colon) and rectum because of their greater accessibility. The major findings have been that various stimuli provoke increased or altered contractile/ myoelectric activity, whereas basal motor patterns (with the exception of subtle alterations in contractile activity and tone) may not differ from healthy subjects. IBS-diarrhea patients may have fewer contractions in the sigmoid colon, reduced short spike-burst activity, increased long spike-burst frequency and alterations in timing and extent of the gastro-colonic contractile and tonic response to food. The net result might be a lowered resistance to flow of luminal content and the passage of loose stool. An increase in high amplitude propagated contractions (HAPCs) has been documented in IBS-diarrhea and functional diarrhea patients; whether excessive activation of HAPCs on waking contributes to the “morning rush syndrome” in IBS-diarrhea is not known. IBS-constipation may have a decreased number of fast colonic and propagated contractions; rectal and colonic compliance and tone need further evaluation13).
Accelerated and delayed whole and segmental gut transit have been documented in IBS-diarrhea and IBS-constipation patients, respectively11). Thus, IBS-diarrhea patients may have accelerated ascending and transverse colon transit of luminal content, the degree of acceleration being positively correlated with stool weight14). Moreover, pharmacologically- induced delay in colonic transit (especially in the left colon) by the 5HT3 receptor antagonist alosetron has been associated with symptom improvement in non-constipated IBS patients15). IBS-constipation patients may have delayed colonic transit, often segmental, although the prevalence of this finding remains controversial as studies have not always clearly differentiated severe (idiopathic) functional constipation from IBS-constipation.
The small intestine in IBS has been explored in relatively few studies. However, a range of subtle alterations in small bowel interdigestive motor activity has been documented11, 16), including alterations in the periodicity of interdigestive cycles, small differences in MMC phase 3 duration and propagation velocity, and variations in MMC phase 2 contractile patterns. Such alterations, however, have not been confirmed in all studies of small bowel manometry in IBS, and so their clinical significance remains uncertain. In postprandial jejunal motor recordings in IBS patients, subtle alterations have also been observed; some patients have a shorter duration of the fed pattern and a higher amplitude, frequency and irregularity of contractions than healthy subjects, but the initial response of the small intestine to food appears intact. Jejunal clustered contractions during fasting and postprandially may be more prominent in IBS patients, with a longer duration of episodes of such clusters, especially in IBS-diarrhea. Small bowel transit time has been variably reported as normal or rapid in patients with IBS-diarrhea; if it is rapid, the colon may be presented with excessive amounts of undigested food products, some of which are osmotically-active, and some of which have secretary effects on the colon. Poorly absorbed carbohydrates, for example, can accelerate proximal colonic transit, while lower than normal stool short-chain fatty acid levels have been reported in IBS-diarrhea, suggesting impaired colonic salvage. Abnormal transit and handling of gas is another component of the motor dysfunction in IBS and, together with spatial summation and hyperalgesia phenomena which appear to amplify the sensory responses to intestinal gas pooling, can be correlated with the symptom of bloating17, 18).
A proportion of patients with IBS display an increased conscious perception to distending stimuli in the small bowel and colon11, 19) and, in some studies, an increased perception of apparently normal motor events in the gut20). Such hypersensitivity to distension has been well-documented in both the distal colon and more proximal colonic segments in patients with IBS. Although reports of pain from balloon distension studies can be influenced by response bias, the low thresholds for balloon distension occur even when controlling for neuroticism. Furthermore, patients with IBS have normal or even increased thresholds for pain or stimulation of somatic neuroreceptors. It is controversial whether a lower threshold for sensation of gas, stool and discomfort in the anorectum appears to be more common in IBS-diarrhea than other subgroups21); the increased rectal sensitivity can be accompanied by excessive reflex motor activity in the rectum. This latter phenomenon may account for the increased frequency of bowel movements, while the increased sensitivity may account for the sense of incomplete evacuation. An exaggerated sensory component of the “gastrocolonic” response to duodenal lipid infusion has also been demonstrated in IBS-diarrhea22).
The alternating bowel patterns in IBS may be due to fluctuations in regional gut sensitivity and in regional autonomic outflow, for example due to interacting physiological stimuli such as feeding and colorectal distension23) and/or differing levels of activity of enteroenteric reflexes, for example gastrocolonic, colorectal etc. Moreover, a specific psychological profile has been related to the combination of abnormal jejunal postprandial motility and hypersensitivity in IBS12). Provocation of symptoms by fructose and sorbitol does not, however, appear related to visceral hypersensitivity, at least to hypersensitivity in the small intestine24). Although visceral hypersensitivity in patients with IBS may affect different levels of the small bowel, whether the ileum exhibits greater or lesser hypersensitivity than the jejunum in IBS is not established. Patients with IBS also display a distorted referral pattern of gut sensation (altered viscerosomatic referral) and perceive intestinal distensions more diffusely over the abdomen than healthy controls. Several alterations in cerebral activation in response to rectal distension, measured by, for example PET or functional MRI scanning, have been reported in IBS; thus, IBS patients may have a propensity to activation of the dorsolateral prefrontal cortex rather than the anterior cingulate cortex during anticipation of rectal distension or during actual rectal distension25). Some evidence is available for specific perceptual alterations in female IBS patients and for differential cerebral activation in IBS-diarrhea versus IBS-constipation, but further studies are required.
2. Putative origins of sensorimotor dysfunction in IBS
A number of possible mechanisms, both central and peripheral, have been proposed to account for the above dysfunctions, and for which there are varying degrees of evidence available11). For dysmotility, mechanisms include: 1) enteric mechanisms such as motor dysfunction associated with ongoing neuroimmune activation, as a consequence of minor degrees of inflammation due to previous infective enteritis; 2) local reflex mechanisms, occurring in response to specific nutrients, such as lipid, or to mechanical distension; 3) extrinsic neural mechanisms, such as abnormalities in extrinsic autonomic innervation; and 4) central mechanisms, whereby higher neural centers modulate peripheral and intestinal motor activity. For enhanced perception, mechanisms include, in addition to those above; 1) altered receptor sensitivity at the viscus itself, occurring through recruitment of silent nociceptors or peripheral sensitisation in response to inflammation or ischaemia; 2) increased excitability of the spinal cord dorsal horn neurons, where repeated distension of the intestine produces central (spinal) hyperalgesia with enhanced intensity and expanded somatic referral of the visceral stimulus; and 3) altered central modulation of sensation, involving psychological influences on the interpretation of these sensations, or altered central regulation of ascending signals from the dorsal horn neurons in the spinal cord. Because the mechanisms of central interpretation of afferent signals are not known, it is not clear whether psychological or neurophysiological mechanisms operate alone or in concert in the conscious perception of incoming signals. Thus, it remains to be established whether the characteristic visceral hypersensitivity in IBS is due to abnormal central processing of normal peripheral stimuli/sensitivity, or due to normal central processing of abnormal peripheral stimuli/sensitivity, or due to a combination of both phenomena.
Central mechanisms
Stress : The level of severe and highly threatening chronic life event stress is correlated with symptom intensity in IBS patients over time26), and also has been related to the onset of post-infective IBS. Of great interest is that, in animal models, chronic stress can provoke an increase in colonic mucosal mast cells and epithelial permeability27). Although results from laboratory based studies, examining various types of mental stressors on colonic or small bowel sensorimotor function, have been variable, there is recent evidence that the colon contractile activity in IBS patients may be more responsive to corticotropin releasing factor when compared to controls. Colonic sensitivity may also be affected by stress differently in IBS patients; thus, in health, mental stress increases sensitivity while relaxation tends to reduce sensitivity in the sigmoid colon to mechanical distension.
Autonomic and endocrine dysfunction : there is growing consensus that an imbalance between sympathetic and vagal function is present in IBS, with an increased sympathetic tone particularly prominent in IBS-diarrhea28); the hypothalamic-pituitary-adrenal axis appears characterised by a low baseline and blunted responsiveness. It is possible that the increased sympathetic tone - which may be evident even during sleep - contributes to the visceral hypersensitivity present in IBS. It remains unclear, however, whether the objective and subjective disturbances of sleep reported in IBS actually contribute to the disease expression, or are the result of an inherent autonomic imbalance. Vagal nerve dysfunction has been demonstrated in several reports, especially in IBS-constipation patients28), but more sophisticated assessments are required in a larger number of patients.
Peripheral mechanisms
Up to 25% of IBS-diarrhea patients report that the onset of symptoms appeared to follow an episode of gastroenteritis29). Increasing experimental evidence now suggests that inflammation in the gut can persistently alter neuromuscular function, and give rise to chronic changes in visceral sensitivity30). Indeed, low-grade inflammation, and an increase in mast cell numbers in the gut (especially in the ileo-cecal region), have been demonstrated in ‘post-infective’ IBS-diarrhea patients31). This is of interest given that the ileum of IBS patients has been previously shown to be excessively sensitive to the secretary effects of perfused bile acids and, also, that cramping abdominal pain in some IBS patients can be directly related to the high amplitude peristaltic contractions which normally sweep through the ileum from time to time, especially postprandially16). Moreover, a recent report shows that enteroendocrine cell hyperplasia can persist after Campylobacter infection, that increased numbers of CD-3 (T) lymphocytes can be present in the lamina propria of colonic biopsies and that an increase in small bowel mucosal permeability can occur32). 5HT release from enteroendocrine cells mediates a component of the peristaltic reflex, and enhanced postprandial release of 5HT in IBS-diarrhea patients has also been documented. Although the role of adverse food reactions and food allergens in the pathogenesis of IBS-diarrhea remains unclear, one may speculate that these have a genesis related to some of the above observations.
In conclusion, a number of factors throughout the brain-gut axis modulate gut sensorimotor function. In the evolution of the pathophysiology of IBS, there has been increasing evidence to support neuroimmune alterations in the bowel in IBS, linking factors such as chronic life event stress and related psychosocial features with peripheral inciting events such as inflammation (Figure 2). The implications from these advances relate to the potential for early psychological and/or pharmacological strategies to prevent the full clinical expression of IBS.
Management strategies
1. General aims and principles of therapy
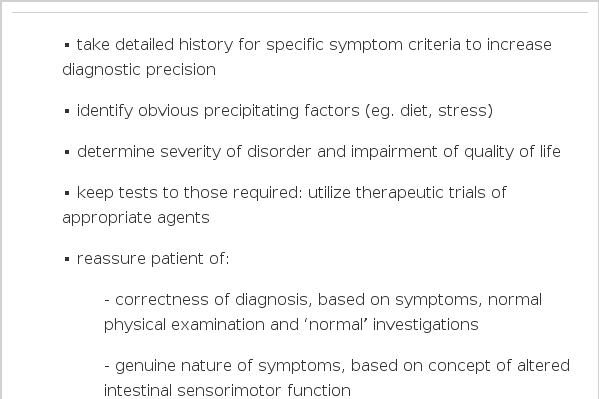
The main aims of therapy in IBS are to achieve a rapid and sustained relief of most - if not all - of the troublesome symptoms, to improve the patient’s quality of life over the longer term33), and to reduce patient health care-seeking behaviuor by empowering him/her to take control of the requirements for, and timing of, therapy. Although the general principles of therapy for IBS have changed little over the years34), the value of a graded multicomponent approach to treatment has been emphasised in recent years35). Moreover, as outlined earlier, there are specific areas where new information is available, leading to a reassessment of specific management strategies. As there is no cure for the disorder, both initial and longer term management strategies, as outlined in Tables 2 and 3, are required to produce optimum outcomes.
2. Initial management strategies
Initial management begins with a detailed history and examination, focusing on the presence of symptoms according to the Manning and the Rome criteria, and the absence of “alarm” symptoms and signs; these symptom criteria will enhance the diagnostic precision and enable a positive diagnosis in most cases, including the type of IBS subgroup36). The reason for the patient’s presentation at this time should be addressed, for example fear of cancer, recent stressful life event etc. In this way, initial treatment strategies can be tailored to the individual and, with further questioning, the degree to which the symptoms affect his/her quality of life can be ascertained. Whether the patient’s IBS is mild, moderate or severe will affect the management plan and the extent of continuing consultation35); in general the greater the severity of the IBS, the greater is the impairment of the quality of life. Also at this stage, any obvious precipitating factors can be identified. A careful dietary history should be taken. If the patient reports that certain foods precipitate symptoms, a food diary may facilitate the more objective identification of any recurrent patterns. High caffeine intake (from coffee, tea and soft drinks) may contribute to diarrhea, and it is important to remember that both prescription and over the counter medicines may affect bowel habit. The presence of obvious stressors, such as work or family problems, should be identified and the relationship of these problems to symptom exacerbations should be sought. It may be appropriate to later embark on management strategies to reduce stress, if support for a relationship between stress and symptoms can be obtained.
A limited series of diagnostic tests can then be employed, but in some cases such tests may be best undertaken only after a therapeutic trial or trials of dietary manipulation or medication (see below). Patients with IBS-diarrhea may require a greater number of investigations to exclude structural, metabolic or infective disorders than the other IBS subgroups. In general, depending on the patient’s age, most patients with IBS should undergo a full blood count, ESR or CRP, and sigmoidoscopy to help exclude inflammatory bowel disease or malignancy. Indeed, it is possible that, in the future, a flexible sigmoidoscopy to obtain a rectal and/or colonic biopsy may enable the documentation of specific histological and/or neuroimmune mucosal alterations which will strongly support or exclude a specific etiology, for example ‘post infective’ IBS. Visualisation of the entire colon (by colonoscopy or barium enema and flexible sigmoidoscopy) should be performed in patients over the age of 40 years presenting for the first time with suspected irritable bowel syndrome. This also applies to patients with a family history of colon cancer or polyps, where colonoscopy is the preferred investigation. Folate deficiency, iron deficiency or steatorrhoea may suggest small bowel malabsorption and screening blood tests and/or small bowel biopsy may be necessary to exclude coeliac disease. In the female patient, pelvic pathology may masquerade as irritable bowel syndrome and gynecological examination and pelvic ultrasonography may be valuable. If intermittent abdominal pain in association with abdominal distension is a prominent symptom, abdominal X-rays (erect and supine) taken during an episode of pain may be useful; this may be particularly important for the patient who has had prior abdominal surgery and is prone to adhesion formation.
Therapeutic trials depend on the most prominent symptoms or on the IBS subgroup. Such trials may include those of dietary fibre supplementation (20–30 g per day) for IBS-constipation and some cases of IBS-diarrhea, dietary manipulation, for example reduction in lactose, fructose or sorbitol intake37), and/or antidiarrheal agents, for example loperamide, for IBS-diarrhea, and antispasmodics for prominent pain in any of the IBS subgroups. Fibre supplementation, using either dietary or a semi-synthetic agent, should be introduced gradually to avoid side effects, and continued for at leasta month before its effect is judged. Empirical antibiotic therapy for giardiasis, especially in the nonconstipated forms of IBS, is sometimes presented because this infection is prevalent and because the yield from stool microscopy can be low; there is no evidence to support the efficiency of this strategy or its cost-effectiveness.
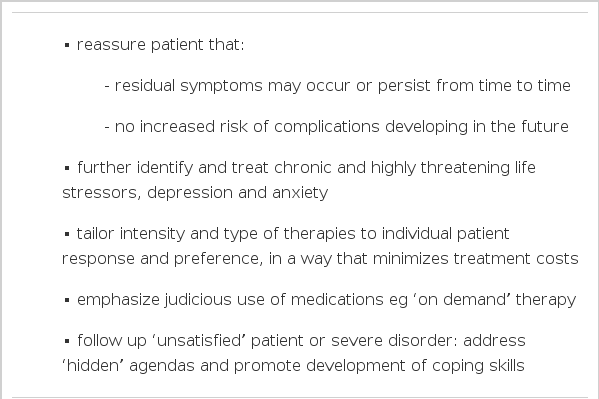
Reassurance of the patient is vital in the initial management stages and four key areas are important to address. Firstly, the fact that the symptoms and results of investigations positively confirm the correctness of the diagnosis should be emphasized. Secondly, that the disorder is a well-recognised entity, with its complex pathophysiology being increasingly defined, for example the reproducible visceral hyperalgesia present in the majority of patients and the evidence for brain-gut dysregulation which readily enable stress to aggravate symptoms. Thirdly, that despite the most appropriate therapies, residual symptoms are likely to recur or persist from time to time, often without any specific provoking factor; in fact there may be considerable shifting between functional diarrhea and IBS-diarrhea, and functional constipation and IBS-constipation. Fourthly, that IBS is a “safe” diagnosis without serious complications or structural complications, such as diverticular disease, and that the disorder is not in any way related to colon cancer; available data indicate that although patients followed up years after a diagnosis of IBS remain, or are again, symptomatic, few patients develop structural GI disorders.
In the future, however, it may be possible to better predict the prognosis depending on the main etiological factors, for example ‘post-infective’ IBS. Finally, the patient should be given the chance to discuss any other specific concerns they may have regarding the symptoms and the diagnosis.
3. Longer-term management strategies
The results of therapeutic trials will lead to confirmation, in many cases, that longer term management will be required. Indeed, it is important to emphasise to the patient that a long-term management plan is usually required. Because IBS is a chronic disorder, non-drug therapy, with lifestyle modification, is preferable to drug therapy, not the least in order to minimise costs. However, ultimately the intensity and specific type of therapies used in the longer-term depends on the individual patient response and preference. Current approaches to the longer term management of IBS include dietary measures, fibre and bulking agents, antispasmodic agents, antidiarrheal agents, laxatives, psychotropic drugs and psychotherapy and other forms of psychological and behavioural therapy34). Evidence for the efficacy for each of these approaches is scarce, largely because of methodologic flaws in most of the studies and because of the presence of a large placebo response in IBS.
Psychological considerations include a firm identification of disorders of mood and of sleep, of previous psychiatric disease, of previous or current physical or sexual abuse and, importantly, of chronic and highly threatening life stressors. The role of psychological treatments, where the above factors are identified, should be discussed. These may include trials of simple relaxation therapy, and/or dynamic psychotherapy, cognitive behavioural therapy and the use of centrally-acting pharmacologic agents. The efficacy of psychological treatments, such as cognitive behavioural treatments, dynamic psychotherapy and hypnotherapy, has not been clearly established; the use of these modalities has been considered in detail recently38). There is evidence that combining multicomponent behavioural therapy with medical therapy produces superior improvement in IBS than that using medical therapy alone39).
Although subgroupings of IBS patients can help in determining the types of therapy, in many cases, the choice of therapy depends most on the dominant single symptom. Because the symptoms of IBS typically fluctuate, and specific drug treatments are limited, medications should be prescribed as required and judiciously, rather than on a regular basis (except for the use of low-dose antidepressants). For abdominal pain, if symptoms are moderate or severe, antispasmodics and anticholingerics may be used to relieve cramping abdominal pain. Although controlled clinical trials with these agents have generally been disappointing40), meta analyses do suggest that certain smooth muscle relaxants can be beneficial in some cases41); the availability of these drugs, however, is not widespread and the effects are relatively modest. These types of drugs, if shown to be helpful, are ideally used in the short term during an exacerbation of symptoms. In resistant cases, low-dose tricyclic antidepressants have been used to treat the abdominal pain of IBS42); the evidence for the use of these agents is, however, limited, although a meta analysis suggests that tricyclic antidepressants are effective in providing overall improvement, with the effect on abdominal pain/discomfort being less pronounced41). Furthermore, it is unclear whether the effect is independent from an effect on depression. Randomised trials of selective serotonin reuptake inhibitors (SSRIs), although often used in IBS, are lacking.
For diarrhea, clinical trials have shown that antidiarrheal drugs are effective, but loperamide seems to have little effect on abdominal pain/discomfort. This medication, if shown to be helpful initially, can be used effectively on an ‘as-needed’ basis, for example if a patient develops diarrhea predictably after eating a larger meal, or in order to attend social engagements. In selected cases, a trial of cholestyramine to control possible bile salt malabsorption may be useful.
For constipation, an increase in dietary fibre and/or dietary fibre supplements should be continued in the longer term, if helpful initially. If symptoms continue, a trial of osmotic laxatives, such as magnesium - containing salts, lactulose or sorbitol can be tried; these medications are safe to use in the longterm and are often effective. Stool softeners can be added to this regimen from time to time. Stimulant laxatives, such as senna, should be avoided in the long term, although some patients find them helpful when used intermittently.
4. Novel therapies and strategies under development
There remains a great need for safe and effective agents which improve the symptom cluster of IBS, which are validated in clinical trials, and which are targetted at the underlying pathophysiological sensorimotor disturbances in IBS. The same considerations apply to psychological approaches, particularly those targeted at the continuing effects of the chronic stress/threat component of the illness. There has been a resurgence of interest in the development of more powerful and effective pharmacological therapies which appear to be able to improve the multiple symptoms of IBS and can address clinically relevant and explicit end-points, such as the overall global symptom improvement or improvement in the quality of life. An example of this is the development of medications which, because of the recent evidence that the sensorimotor disturbances in IBS may - at least in part - be related to disturbed serotonergic mechanisms in the gut, act on 5HT3 and 5HT4 receptors43). The selective 5HT3 antagonist, alosetron, has been shown to be effective in treating the symptoms of urgency, loose stool consistency and abdominal discomfort in female patients with IBS-diarrhea15). However, constipation can occur, in keeping with its pharmacological property of slowing colonic transit as well as reducing visceral sensitivity. Unfortunately, because of concerns regarding the development of severe constipation, as well as that of the rare occurrence of ischemic colitis, this apparently useful medication was withdrawn from the market. Other 5HT3 antagonists remain under development.
Serotonergic agents which have agonist activity have also been shown to have potential clinical benefit. The 5HT4 partial agonist, tegaserod, has been reported to be well tolerated in Phase 3 clinical trials of sixteen weeks duration (four week placebo run-in phase and twelve weeks active treatment) in patients with IBS-constipation. Reported adverse events were comparable between tegaserod and placebo, with the exception of transient diarrhea which was slightly higher in the tegaserod groups compared to placebo. This symptom usually resolved without the need for withdrawal of the study medication. In these trials, tegaserod 6 mg bd resulted in a significant increase in the proportion of patients achieving the symptom global assessment of relief (including overall well-being, abdominal pain, altered bowel function and bloating) in comparison to placebo. The difference was typically 12–15%, and the onset of relief was rapid with many patients responding in the first few days of treatment44).
The clinical availability of such potentially more useful agents may change the traditional clinical management paradigm as outlined above. Thus, by analogy to gastroesophageal reflux disease, one may need to not only consider ‘step-up’ but also ‘step-down’ approaches. The optimum use of such agents will also require better identification of specific symptom subgroups and, of course, the use of such medications will be largely driven by cost considerations. The ‘step-up’ approach (minimum initial therapy) would have the advantages of avoiding overtreatment and containing initial drug costs; the disadvantages would be that patients may continue with symptoms unnecessarily and this may lead to unnecessary investigations. ‘Step-down’ therapy (higher level initial therapy) could have the advantages of rapid symptom relief and the avoidance of unnecessary investigations and associated costs; the disadvantages would be a potential for overtreatment and higher initial drug costs.
There are a number of other agents that offer promising opportunities for the future treatment of IBS and which are undergoing clinical development or evaluation. These include agents with visceral analgesic and sensorimotor-modulatory properties, such as the kappa opioid agonist fedotozine45), other serotonergic agents, neurokinin antagonists, newer antimuscarinic agents, cholecystokinin antagonists, the alpha 2-adrenergic agonist, clonidine. Other strategies of potential use, but entirely speculative at present, involve the earlier treatment of selected cases of infective gastroenteritis with antibiotics, and the use of neuroimmune modulators to alter the course of post-inflammatory or even stress-response neuroimmune processes.