Early dipyridamole stress myocardial SPECT to detect residual stenosis of infarct related artery: comparison with coronary angiography and fractional flow reserve.
Article information
Abstract
Background
The detection of residual stenosis of infarct related artery (IRA) at early stage after acute myocardial infarction (AMI) is crucial in clinical decision making for interventional revascularization. The aim of this study was to evaluate the relevancy of early dipyridamole stress myocardial SPECT to detect functionally and luminologically significant residual stenosis of IRA after AMI.
Methods
Twenty five consecutive patients (M:F=19:6, age: 56±13yrs) with AMI underwent SPECT and coronary angiography within 5 days of the attack. Infarct related arteries with FFR < 0.75 and diameter stenosis (DST) >70% were regarded to have functionally and morphologically significant residual stenosis. Reversible perfusion defect was defined if there was improvement of the perfusion score more than one grade in infarct segments on rest images of SPECT compared with stress images.
Results
Mean FFR and DST were 0.76±0.14 and 74±15%. SPECT showed no significant correlation with both FFR and DST with Kendall’s coefficiency of 0.28 (p=0.05) and 0.13 (p=0.35). The sensitivity and specificity of SPECT to detect functionally and morphologically significant residual stenosis were 92%, 31% and 83%, 29%.
Conclusion
The early dipyridamole stress myocardial SPECT after AMI does not seem to be a useful non-invasive test for the detection of functionally and luminologically significant residual stenosis of IRA.
INTRODUCTION
The detection of the residual ischemia of the infarct myocardium through a non-invasive method is of great importance in evaluating the severity of the stenosis of infarct related artery (IRA) and in determining the need for a revascularization therapy1–4). There are numerous non-invasive methods to find the significant stenosis of the coronary artery, such as exercise, induced or drug-induced echocardiography and the myocardial SPECT. Of the studies mentioned above, dobutamine stress echocardiography, by detecting the biphasic response, is known to be a useful method in determining the residual stenosis of the IRA7–9). The safety and the prognostic predictability of early dipyridamole stress myocardial SPECT after acute myocardial infarction (AMI) has been studied previously10, 11) but no studies have been done on its efficiency as a diagnostic tool in evaluating the residual stenosis of the IRA.
In this study, to evaluate the relevancy of early dipyridamole stress myocardial SPECT to diagnose the residual stenosis of the IRA after an attack of myocardial infarction, we have compared with coronary angiography, the luminological aspect of the stenosis and fractional flow reserve (FFR), an index of the functional capacity of the IRA.
PATIENTS AND METHOD
1. Patients
We included in our study a total of 25 patients (19 male, 6 female; mean age, 56 years; range 43–69) who had been admitted to our hospital from Jan.1999 to Sept. 1999.
The diagnostic criteria of AMI were typical chest pain that did not resolve with the administration of sublingual nitroglycerin, an EKG finding of 2 mm elevation of the ST segment in more than two leads, a regional wall motion abnormality in more than two adjacent sites by the transthoracic echocardiography and finally, an elevation of the CK-MB by more than three-fold. We have excluded patients with a history of acute MI, patients who had previously undergone CABG, patients with a history of PTCA, anyone who was hemodynamically unstable and those with severe ventricular arrhythmia.
2. Methods
1) Coronary angiography
The coronary angiography was performed five days after the onset of MI. The coronary angiography was approached by the Seldinger method using a 6–8F guiding catheter which was introduced into the femoral artery and advanced into the ostium of the target vessel. Contrast dye was administered according to the routine procedure. The quantitative analysis of the stenotic vessel was done by the Targano projector. The percent diameter stenosis, DST% was derived by measuring the minimal luminal diameter (MLD) and comparing it to the reference artery diameter by using a caliber. An IRA having a percent diameter stenosis of more than 70% was considered to have a luminologically significant stenosis and such a case was revascualized by percutaneous coronary intervention with balloon or stent.
2) Fractional Flow Reserve (FFR)
The FFR was measured by the 0.014 fiberoptic pressure monitoring wire (Radi Medical System, Uppsala, Sweden) which was advanced through the catheter, introduced into the IRA and positioned distal to the stenosis before the initiation of the coronary intervention. 18–20 microgram of adenosine was then injected into the coronary artery to induce maximal coronary blood flow, corresponding with minimal distal coronary pressure. When steady-state hyperemia was achieved, FFR was calculated as the ratio of the mean distal intracoronary pressure measured by the wire to the mean arterial pressure measured by the coronary guiding catheter, simultaneously. If the FFR was below 0.75, the IRA was considered to be a functionally significant stenosis.
3) Dipyridamole stress myocardial SPECT
Dipyridamole stress myocardial SPECT was performed four days after the onset of MI. In the TI-201 group, rest TI-201 SPECT acquisition was initiated 10 minutes after the injection of 111–148 MBq (3–4 mCi) of TI-201 with the patient at rest. Repeated TI-201 SPECT acquisition was sequentially performed 30 minutes after injection of TI-201 in the same position. In the Tc-99 m-MIBI group, Tc-99 m-MIBI SPECT acquisition was initiated 1 hour after injection of 1110 MBq (30 mCi) of Tc-99 m-MIBI at peak dipyridamole stress (0.56 mg/kg for 4 minutes). Repeated Tc-99 m-MIBI SPECT acquisition was sequentially performed 70 minutes after injection of Tc-99 m-MIBI in the same position. Image acquisition was performed with a dual detector gamma camera (MultiSPECT; Chicago, III). The interpretation of the images reconstructed with 180 degrees acquisition was made on the basis of short axis and longitudinal and transverse long axis. Analysis of SPECT images was performed visually with semiquantitative scoring from 0 to 3: 0 (normal uptake), 1 (mild to moderately decreased), 2 (severely decreased) and 3 (defect) according to the 16-segment model. Infarct myocardium was considered to be a reversible residual ischemia when perfusion defect extent and/or severity was larger (>1 grade) on the stress images than the resting images.
4) Statistics
All the results were expressed by mean value±standard deviation and the results were analyzed by its comparison to Kendall’s coefficiency. The percent diameter stenosis (DST%) derived by coronary angiography and FFR were analyzed by the curvilinear regression analysis. The results with a p value of less than 0.01 were the only values that were considered statistically significant in this study.
RESULTS
1. Patients
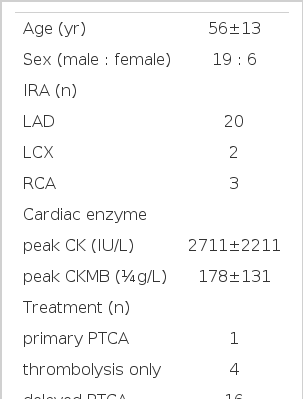
The total number of patients that had participated in this study was 25, with a male to female ratio of 19:6. Their average age was 56±13 years. Out of 25, 20 had IRA in LAD, 2 in LCX and 3 in RCA. One patient had primary percutaneous transluminal coronary angioplasty (PTCA) and 4 had thrombolytic therapy. Five days after the onset of MI, 16 patients underwent coronary angiography which revealed significant stenosis and, thereafter, had delayed PTCA. The remaining 4 patients had conservative management. The average of percent diameter stenosis (DST%) were 74±15% and the average of the FFR was 0.76±0.14 (Table 1).
2. Correlation of FFR and coronary angiography
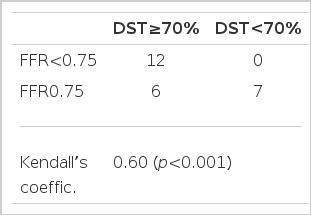
The FFR is a functional index of stenosis which holds any significance only when the value is less than 0.75. FFR less than 0.75 in detecting the stenosis of more than 70% on coronary angiography had shown a concordance by Kendall’s coefficiency of 0.604 (p<0.001) (Table 2). Furthermore, two indices have shown a meaningful correlation by the curvilinear analysis with r=0.82 (p<0.001) (Figure 1).
3. Dipyridamole stress myocardial SPECT and FFR
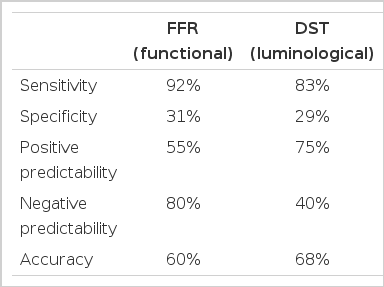
Dipyridamole stress myocardial SPECT and the FFR of the IRA have low concordance, with Kendall’s coefficiency of 0.28 (p=0.05) (Table 3). The dipyridamole stress myocardial SPECT in detecting FFR less than 0.75 had a sensitivity of 92%, specificity of 31%, a positive predictive value of 55% and a negative predictive value of 80% (Table 4).
DISCUSSION
After an attack of acute myocardial infarction, there are not infrequently residual stenosis in the infarct-related arteries1), In estimating the degree of the residual stenosis of the IRA, one can predict the outcome of the disease course, such as sudden death, congestive heart failure, the recurrence of myocardial infarction and post myocardial infarction angina2–4). Therefore, in order to prevent such cardiac events and to improve the prognosis of the disease course, it is customary to revascularize the IRA with the residual stenosis on admission5, 6). The early detection (<1 week) of the residual stenosis by a non-invasive method is of great importance in determining the therapeutic approach. There are numerous studies on the non-invasive diagnostic tools, such as the treadmill test, exercise or drug-induced echocardiography and myocardial SPECT. Out of these tests, the early dobutamine stress echocardiography after AMI, in many studies, has been described to be an efficient test in diagnosing the residual stenosis of the IRA7–9). Gibson et al.3) Travin et al.4) and recently, Brown et al.10) state the efficiency of the early dipyridamole myocardial SPECT within a week after the onset of MI in predicting the prognosis of the disease course. But the efficiency of the early dipyridamole myocardial SPECT in determining the residual stenosis is inadequate, for there has been only a limited amount of studies that have been done on the matter. Therefore, the objective of this paper is to evaluate the relevancy of early dipyridamole stress myocardial SPECT in the early detection of the residual stenosis of the IRA and this can further contribute to the determination of the need for an early revascularization before discharge from medical care after acute onset of MI. Therefore, we have compared myocardial SPECT with coronary angiography, an anatomical index of stenosis and the fractional flow reserve, a functional index of stenosis.
1. Fractional Flow Reserve
The FFR is a useful functional index in analyzing the residual stenosis of the coronary artery. This index, first introduced by Pijls et al.13) was derived by the ratio of the mean distal intracoronary pressure measured by the wire to the mean arterial pressure measured by the coronary guiding catheter13, 14). FFR is independent to the changes of blood pressure, heart rate and hemodynamic changes such as the diastolic ventricular volume15). In the case of multiple coronary artery stenosis, the FFR is known to be the lesion-specific functional index16). Furthermore, the FFR has proven, in many studies, to be a well-defined cutoff value of 0.75 and it has been shown to accurately distinguish stenosis capable of inducing myocardial ischemia (FFR<0.75) from those that are not (FFR≥ 0.75)17–19). Likewise, in this study, by the curvilinear regression analysis, the residual stenosis determined by the coronary angiograpgy and the FFR had shown a significant correlation with the coefficency of 0.82 (p<0.001). The FFR, being less than 0.75, correlates to the residual stenosis of more than 70% by the coronary angiography, with Kendall’s coefficient of 0.604 (p<0.001). In our study, 12 patients with a significant stenosis of more than 70% had a FFR value of less than 0.75 and 6 out of 13 patients (46%) with an FFR value of more than 0.75 had a residual stenosis of more than 70% showing false negative. We presume the false negative of the study to be due to the partial necrosis of the myocardium, the loss of the microvasculature and the increase in the resistance of the microvasculature with dilative dysfunction which, in turn, increases the FFR compared to the actual luminological stenosis20, 21).
2. The efficiency of an early dipyridamole stress myocardial SPECT in diagnosing the functionally significant stenosis of the IRA
Out of the 20 patients with a positive early dipyridamole stress myocardial SPECT, 11 with an FFR of less than 0.75 have shown to have functionally significant stenosis, whereas those with an FFR of more that 0.75 had no functionally significant stenosis which reflected false positive. Four out of the five patients with negative results of the early dipyridamole stress myocardial SPECT had no functionally significant residual stenosis and only one had shown a false negative with a functionally significant stenosis. As a result, the early dipyridamole stress myocardial SPECT and the FFR had a low concordance with Kendall’s coefficient of 0.28 (p=0.05), which had shown a high sensitivity of 92%, negative predictability of 80% and low specificity of 31% and a positive predictability of 55%.
3. The efficiency of the early dipyridamole stress myocardial SPECT in diagnosis of the luminologically significant stenosis of the IRA
15 out of the 20 patients with a positive result of the early dipyridamole stress myocardial SPECT had shown more than 70% residual stenosis, whereas 5 had shown less than 70% residual stenosis, representing a false positive. 2 patients out of the five with a negative early dipyridamole stress myocardial SPECT had no significant residual stenosis by the coronary angiography, whereas 3 had shown to have a significant residual stenosis with a false negative. As a result, the early dipyridamole stress myocardial SPECT and the FFR had a low concordance, Kendall’s coefficient value of 0.13 (p=0.35), showing a high sensitivity of 83%, positive predictability of 75%, a low specificity of 29% and a negative predictability of 40%.
Therefore, the FFR an index of the functional stenosis of the IRA and coronary angiography, a luminologic index of the stenosis, both had shown a relatively high sensitivity but a low specificity, with practically no or very little correlationship to each other. Currently, as shown in numerous studies, a low value of coronary flow reserve (CFR), after revascularization procedure in patients with AMI, has been reported which is the result of a transient vasodilatory dysfunction22, 23). Likewise, the dipyridamole stress myocardial SPECT may also be affected by the dysfunction of the epicardial coronary arteries and the microvasculature of the myocardium24). After a successful PTCA without any residual stenosis, a perfusion defect can be seen by the myocardial SPECT image which is due to the transient dysfunction of the microvasculature of the myocardium and as claimed by Manyari et al.25) does not mean that there is any evidence of a significant residual stenosis. After a successful thrombolytic therapy or a natural reperfusion event, a transient perfusion defect may take place without any significant myocardial damage or necrosis20, 26). This, in turn, can compromise the dilative perfusion of the myocardium. This phenomenon can help explain the false positive results of the early dipyridamole stress myocardial SPECT of this study (Figure 2). Likewise, there can be a perfusion defect of both the resting and stressed image which is due to the transient dysfunction of cell membrane and edema of the cells of the microvaculature which has undergone a stunning phenomenon, with/without significant damage (Figure 3). In this phenomenon, when recovered from the stunned state, the perfusion defect of the resting and the stress image can be eventually recovered27, 28). Therefore, it is necessary to compare the stressed image with the 24hr delayed or re-injection image rather than the resting image of the myocardial SPECT29–31) (Figure 4).

A case showing inconsistency of early dipyridamole myocardial SPECT with FFR and coronary angiography. A) Coronary angiogram showing luminologically insignificant stenosis (DST=36%) of LAD (arrow). B) Coronary pressure trace showing functionally insignificant stenosis with FFR of 0.92. C) Early dipyridamole myocardial SPECT showing significant reversible perfusion defect of anteroseptum (arrows). FFR, fractional flow reserve; DST, percent diameter stenosis; LAD, left anterior descending artery.
A case showing consistency of early dipyridamole myocardial SPECT with FFR but inconsistency with coronary angiography. A) Coronary angiogram showing luminologically significant stenosis (DST=80%) of LAD (arrow). B) Coronary pressure trace showing functionally insignificant stenosis with FFR of 0.88. C) Early dipyridamole myocardial SPECT showing fixed perfusion defect of apex (arrows). DST, percent diameter stenosis; LAD, left anterior descending artery.
A case of stunned myocardium showing inconsistency of early dipyridamole myocardial SPECT with coronary angiography. A) Coronary angiogram showing luminologically significant stenosis (DST=78%) of LAD (arrow). B) Anterior wall (arrows) showing fixed perfusion defect on early dipyridamole myocardial SPECT showed improvement of perfusion on 24 hr delayed image. DST, percent diameter stenosis; LAD, left anterior descending
In conclusion, the early dipyridamole stress myocardial SPECT does not seem to be a useful non-invasive test for the determination of the residual stenosis of IRA because of the stunning phenomenon and the transient functional disability of the microvasculature, which very often occur within a week of the AMI and can have an effect on the myocardial perfusion.