Aortic Valve Involvement in Behçet’s Disease. A Clinical Study of 9 Patients
Article information
Abstract
Objectives
To assess the clinical features, pathologic findings, postoperative results and the effects of immunosuppressive therapy in patients with Behçet’s disease (BD).
Methods
We reviewed the postoperative course of the 9 BD patients who underwent a total of 17 aortic valve replacement procedures with prosthetic valves.
Results
Histological examination of the aortic valve commonly revealed diffuse myxoid degeneration (75 percent). Of 17 valve replacement surgeries, 13 surgeries resulted in complications, such as detachment of the prosthetic valve with perivalvular leakage and dehiscence of the sternotomy wound, within an average of 5 months (range from 1 month to 14 months). The rate of prosthetic valve detachment was 76 percent (13 of 17 surgeries). Four of the 9 patients (44 percent) who underwent aortic valve replacement procedures died of heart failure or infection associated with the detachment of the prosthetic valve, and perivalvular leakage within an average of 9 months. Aortic insufficiency associated with dehiscence of the prosthetic valve developed in 11 of 12 surgical cases (92 percent) with a mechanical valve and 2 of 5 surgical cases (40 percent) with tissue valves. Thirteen of 15 surgeries (87percent) which were not given postoperative immunosuppressive therapy developed complications, while none of 2 surgeries that used postoperative immunosuppressive therapy with prednisolone (1mg/kg/day) and azathioprine (100mg/day) had these complications.
Conclusion
The rates of prosthetic valve detachment in BD involving aortic valve were higher than those of other diseases. Aortic valve involvement was also one of the poor prognostic factors in BD. Intensive postoperative immunosuppressive therapy and surgical methods may be important factors for postoperative results.
INTRODUCTION
Behçet’s disease (BD) is an inflammatory condition of multiple organ systems in which recurrent oral and genital ulcers are the most typical signs1). BD associated with large vascular lesions is called vasculo-BD, the major manifestations of which are aneurysm formation, arterial occlusion and venous occlusion. Reported cardiovascular involvement includes pericarditis, myocarditis, conduction system disturbances, acute myocardial infarction and cardiomyopathy2–4). Aortic valvular involvement in BD, however, has rarely been reported. In 1980, Rae et al.5) first reported a case of BD with aortic insufficiency. Eight cases that have been reported in English literature revealed that most patients needed valve replacement and resulted in serious complications such as dehiscence of the prosthetic valve, perivalvular leakage, false aneurysm at the cannulation site, dehiscence of the sterntomy site and death5–11). Modified surgical technique, such as valved conduit procedure, recently has suggested decreasing the postoperative complications12,13). It is suggested that new surgical and medical therapies are needed to reduce the postoperative complications and mortality rates.
So, we have identified aortic valvular insufficiency in 9 patients with BD who underwent a total of 17 valve replacements. Clinical features, pathologic findings, postoperative complications, surgical methods and immunosuppressive therapy were compiled.
PATIENTS AND METHODS
1. Patients
We reviewed the medical records of the 10 Korean patients with BD who received aortic valve replacement because of severe aortic insufficiency. Three of the 10 patients underwent surgery at Seoul National University Hospital from 1986 to 1988. Seven of the 10 patients underwent surgery at Yonsei University Medical Center from 1990 to 1997. One of these 10 patients who had rheumatic fever in the past history, however, was excluded from the study.
None of the 9 patients had rheumatic fever, bacterial endocarditis or congenital heart disease before entering the study. All sera were negative for antinuclear antibodies, rheumatoid factor and VDRL. None showed the characteristic stenosis of the aortic arch and its branches as seen in Takayasu’s arteritis. None showed vegetations or calcifications on the aortic valve in echocardiography. None of the patients exhibited characteristic findings of rheumatic valvular disease, which includes thickening, deformity and shortening of multiple valves.
None of the patients were older than 42 years of age. Seven of the 9 patients developed aortic insufficiency during the follow-up for BD; two patients were diagnosed with BD after developing aortic insufficiency.
2. Surgical methods and follow-up (Table 2)
These 9 patients underwent a total of 17 aortic valve surgeries. The operation time was dyspnea associated with heart failure or moderate to severe aortic regurgitation on echocardiography. The surgical procedures of aortic valve replacement were with the following prosthetic valves: st. Jude, Carbo Medics (S-J, C-M) (Nos. 2a, 2b, 3a, 3b, 3c, 4, 6a, 8b, 9a, 9b, 9c), tissue valves: Inoescu Shiley (IS) (Nos. 7, 8a) and autografts with pulmonic valve or pericardium (Nos. 1, 5, 6b). We followed up to see postoperative complications with transthoracic or transesophageal echocardiography at 2 to 3 months intervals after surgery (range from 2 months to 3 years and 10 months).
3. Immunosuppressive therapy
After surgery, immunosuppressive therapy with prednisolone (1 mg/kg/day) and azathioprine (100 mg/day) was given in 2 patients (Nos. 5, 6b) who had no evidence of bacterial or fungal infection on the frozen section of valve or endocardium, or during tissue culture. Prednisolone was tapered after 2 months and azathioprine was continued at the same dose for an average of 19 months.
4. Statistical analysis
The association with postoperative complications between each surgical method and immunosuppressive therapy were analyzed using Fisher’s exact test. The level of significance was set at p<0.05.
RESULTS
The mean age of 5 men and 4 women patients when entering into the study was 33±6 years (range from 22 to 42 years of age).
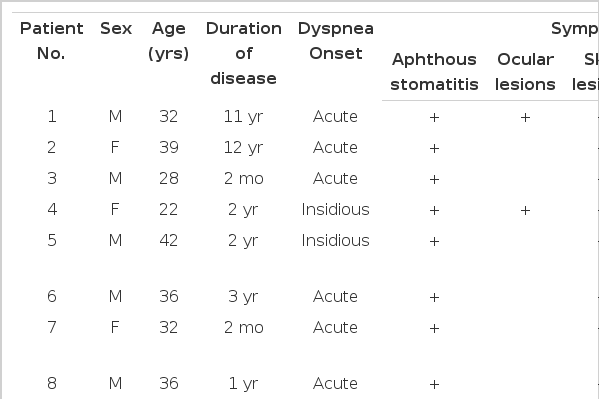
Five patients (Nos. 1, 2, 4, 8, 9) had three or more major symptoms (aphthous stomatitis, genital ulcers, skin lesions and/or ocular lesions). Two patients (Nos. 5, 7) had two major symptoms (aphthous stomatitis and skin lesion) and two minor symptoms (arthritis and vasculitis). Two patients (Nos. 3, 6) had two major (aphthous stomatitis and skin lesions) and one minor symptom (vasculitis) (Table 1). According to Shimizu’s classification (14), we had one (Nos. 1) complete BD, 4 (Nos. 2, 4, 8, 9) incomplete BD and 4 (Nos. 3, 5, 6, 7) suspected BD. Three patients (Nos. 7, 8, 9) were previously reported as cases15). The major manifestations of BD were aphthous stomatitis and skin lesions (100 percent), genital ulcers (44 percent) and ocular lesions (22 percent) (Table 1).
Seven patients (78 percent) acutely developed dyspnea on exertion. Aortic insufficiency was developed late in the course of BD (average of 3 years and 11 months: range from 2 months to 12 years) (Table 1).
Valve involvement consisted of 5 isolate aortic insufficiency (56 percent) and 4 combined aortic and mitral insufficiancy (44 percent). Two patients (Nos. 1, 2) had concomitent complete atrioventricular block (Table 2).
The macroscopic findings of the aortic valve and aortic wall included central perforation of the cusp with aneurysm of the Valsalva sinus in 4 patients (44 percent), annular dilatation in 3 patients (33 percent) and fused valves with or without myxoid change in 2 patients. The microscopic pathologic features of the aortic valve among 8 valves that were available after surgery included diffuse myxoid change and fibrin exudation in 6 cases (75 percent), focal nodular necrosis in 1 case and fibrous thickening with mucin deposit in 1 case. The microscopic findings of the aortic wall among 6 aortic walls that were available after surgery included destruction or cystic degeneration of the tunica media in 3 cases (50 percent), fibrotic change in 2 cases (30 percent), active inflammatory cell infiltration on media, adventitia and peri-vasa vasorum in 1 case and marked mucopolysaccharide deposition in 1 case (Table 3).

Pathlogic findings of the aortic valves and thoracic aorta in surgical patients with aortic regurgitation caused by Behçet’s disease.
Nine patients underwent a total 17 valve replacement surgeries and 13 surgeries resulted in complications (dehiscence of the prosthetic valve with perivalvular leakage, death due to heart failure or infection associated with dehiscence of the prosthetic valve and dehiscence of the sternotomy site). The rate of prosthetic valve detachment was 76 percent (13 of 17 months) (Figure 1). Aortic insufficiency associated with dehiscence of the prosthetic valve developed in 11 of 12 surgical cases (92 percent) with a mechanical valve and 2 of 5 cases (40 percent) with tissue valves (Table 2). The rates of postoperative complication in surgeries with tissue valves were lower than those with mechanical valves (p=0.053).

Survival curve and freedom from reoperation curve for postoperative complications in surgical patients with aortic regurgitation caused by Behçet’s disease.
Thirteen of 15 cases (86 percent) were not given immunosuppressive therapy after surgery developed complications. On the other hand, 2 cases which were given postoperative immunosuppressive therapy were free from complications during an average of 19 months (range from 18 months to 20 months). The rates of postoperative complication in cases with immunosuppressive therapy after surgery were lower than those without immunosuppressive therapy after surgery (p=0.044).
Four of 9 patients (44 percent) died of heart failure or infection associated with dehiscence of the prosthetic valve and perivalvular leakage within an average 11 of months (range of 2 to 19 months) after surgery (Figure 1).
DISCUSSION
The primary target organs of BD are mucous membranes of the mouth, genitalia and eye. Arterial involvement is not well recognized, but in some cases it may be in the forefront and life threatening16). Aortic valve involvement occurred late in the course of BD as an arterial lesion of BD that occurred at 3.2 to 7.9 years in the course of BD17). We observed the mean period of 3 years and 11 months between the first sign of BD and the discovery of aortic valvular lesion. However, most patients (78 percent) experienced abrupt dyspnea on exertion.
The pathogenesis of valvular regurgitation in BD is unknown. The contributive factors were suggested as dilatation of the aortic or mitral annulus caused by atypical inflammation, destruction of the valve tissue itself, diffuse aortitis of the ascending aorta and aneurysm of Valsalva sinus6,8,10). The microscopic features of the aortic valve in BD have been reported from normal to fibrosis with/without inflammation5,6,8,10). The histologic features of the aortic wall have also been reported as normal, fibrosis or acute aortitis5,6,10). The histologic findings of aortitis in BD are well known; the active vasculitis stage is characterized by intense infiltration of inflammatory cells, particularly involving the media and adventitia. They consist predominantly of neutrophils, lymphocytes and plasma cells, mixed with histiocytes and eosinophils and sometimes with giant cells. In the scar stage, fibrous thickening of intima and adventitia were observed, as well as fibrous scar with condensation of elastic lamina in media18).
In our cases, we observed central perforation of the cusp with Valsalva sinus aneurysm in 4 cases and annulus dilatation in 3 cases among 9 surgical cases. The pathologic finding of the aortic valve was nonspecific and the diffuse myxoid degenerative change was common (75 percent). Aortic wall exhibited evidence of medial destruction with nospecific inflammation to active aortitis. Therefore, we speculated that aortic insufficiency in BD might be associated with myxoid degeneration of the aortic valve, annular ectasia, aneurysm of Valsalva sinus with nonspecific inflammation or with vasculitis of the aortic wall.
BD infrequently requires intestinal or vascular surgical procedures. The recurrence rates were reported as 40 to 55 percent in aortic valve surgery 40 to 80 percent in intestinal surgery and 74 percent in arterial surgery12,13,17,18). Ando et al.13) showed that the rates of mortality and prosthetic valve detachment were 20 percent and 40 percent after surgical treatment of the 10 patients with BD involving aortic regurgitation in comparison with 44 percent and 67 percent in our study (Figure 1). But they used postoperative steroid in all patients. The recurrence of intestinal ulceration, arterial aneurysm, graft thrombosis and prosthetic valve detachment developed in situ or in a nearby operation site. Le Thi Huong17) suggested that the high recurrent rate of aneurysm or graft thrombosis was developed at the anastomosis site with synthetic prosthetic prosthesis or venous graft in the arterial lesion with BD. The pathogenesis for the high rate of tissue destruction at the operation site is unknown. Le The Huong, however, suggested that it was “arterial wall aphthae” resulting from pathergy phenomenon, indicating that the aneurysmal wall of the artery has severe medial necrosis resembling epidermal and dermal junction necrosis in the mucocutaneous lesions17,19). He also suggested that the efficacy of corticosteroid and/or immunosuppresive drug might reduce inflammation.
In our study, 13 of 17 surgeries resulted in inflammation at the detached prosthetic valve and fragile lesions at the suture site. One case showed poor tissue healing at the sternotomy site. We observed a similar phenomenon to pathergy with pustules or a sterile abscess-like lesion at the suture site or incision site. These also showed detachment of the prosthetic valve with perivascular leakage and inflammation at the suture site. We could not, however, document the medial necrosis of the aortic wall in 2 surgical cases.
Intensive anti-inflammatory therapy might reduce the inflammatory reaction on the anastomotic site of the aortic wall and reduce complications, such as dehiscence of the prosthetic valve or sternotomy wound. Several authors12,13,17,19) have reported that corticosteroids and/or immunosuppressive therapy were effective in reducing inflammation. Therefore, we initiated immunosuppressive therapy with prednisolone 1 mg/kg and azathioprine 100 mg daily in 2 cases. These 2 cases have not shown complications after aortic valve replacement. In contrast, 13 of 15 surgical cases (87 percent) which were not given postoperative immunosuppressive therapy showed several complications, such as dehiscence of the prosthetic valve and perivalvular leakage.
Two kinds of aortic valve, including mechanical valve, bovine or autologus tissue valve (pulmonic valve, pericardium), were used. Eleven of 12 cases with mechanical valves and 2 of 5 cases with tissue valve developed postoperative complications. The recurrence rate was higher in the mechanical valves (92 percent) than tissue valves (40 percent). Even though the differences between mechanical and tissue valves were not statistically significant because of low parameter, it could be considered as one of the factors associated with postoperative complication.
Poor prognostic factors in BD include male gender and a young age of onset, involvement of CNS and arterial or venous involvement, vein and gastrointestinal perforation17). In addition, we suggest including aortic valve involvement as a poor prognostic factor because of the high mortality rate (44 percent) in our cases.
In summary, perforation of the valve cusp, aneurysm of Valsalva sinus and diffuse myxoid degeneration of the valve were common pathologic findings. Valve replacement with tissue valves and intensive postoperative immunosuppressive therapy may be important factors for postoperative complications. But further studies are needs to get clinical significance.
Acknowledgements
We appreciate S. Louis Bridges, Jr. at the University of Alabama at Birmingham for excellent comments and review.