Prognostic value of computed tomographic coronary angiography and exercise electrocardiography for cardiovascular events
Article information
Abstract
Background/Aims:
This study is a head-to-head comparison of predictive values for long-term cardiovascular outcomes between exercise electrocardiography (ex-ECG) and computed tomography coronary angiography (CTCA) in patients with chest pain.
Methods:
Four hundred and forty-two patients (mean age, 56.1 years; men, 61.3%) who underwent both ex-ECG and CTCA for evaluation of chest pain were included. For ex-ECG parameters, the patients were classified according to negative or positive results, and Duke treadmill score (DTS). Coronary artery calcium score (CACS), presence of plaque, and coronary artery stenosis were evaluated as CTCA parameters. Cardiovascular events for prognostic evaluation were defined as unstable angina, acute myocardial infarction, revascularization, heart failure, and cardiac death.
Results:
The mean follow-up duration was 2.8 ± 1.1 years. Fifteen patients experienced cardiovascular events. Based on pretest probability, the low- and intermediate-risks of coronary artery disease were 94.6%. Odds ratio of CACS > 40, presence of plaque, coronary stenosis ≥ 50% and DTS ≤ 4 were significant (3.79, p = 0.012; 9.54, p = 0.030; 6.99, p < 0.001; and 4.58, p = 0.008, respectively). In the Cox regression model, coronary stenosis ≥ 50% (hazard ratio, 7.426; 95% confidence interval, 2.685 to 20.525) was only significant. After adding DTS ≤ 4 to coronary stenosis ≥ 50%, the integrated discrimination improvement and net reclassification improvement analyses did not show significant.
Conclusions:
CTCA was better than ex-ECG in terms of predicting long-term outcomes in low- to intermediate-risk populations. The predictive value of the combination of CTCA and ex-ECG was not superior to that of CTCA alone.
INTRODUCTION
The American Heart Association/American College of Cardiology (AHA/ACC) guidelines for ischemic heart disease recommend exercise electrocardiography (ex-ECG) as the initial screening test for patients who are able to exercise and have a normal electrocardiographic result [1]. Ex-ECG provides acceptable sensitivity and specificity for diagnosis of coronary artery disease (CAD), and obtaining information on functional capacity and prognosis [2]. Ex-ECG is limited to provide information about the degree and location of coronary artery stenosis. Therefore, ex-ECG showed poor prognostic values in several reports [3-5]. In contrast to ex-ECG, computed tomography coronary angiography (CTCA) showed high sensitivity and specificity for diagnosis of coronary artery stenosis [4-7]. Besides its diagnostic accuracy, the high prognostic value of CTCA has been reported [5,8-11]. However, only a few studies have conducted a head-to-head comparison of the prognostic value between ex-ECG and CTCA [3-5,12]. In this study, the predictive values of ex-ECG and CTCA for cardiovascular outcome were compared. In addition, we tried to find the best prognostic parameter by using both tests.
METHODS
Study population
For the study, 1,011 patients who underwent both ex-ECG and CTCA for evaluation of chest pain at Gyeongsang National University Hospital between January 2007 and December 2013 were identified. Based on electronic medical records, patients with chest pain, those older than 18 years and those who had undergone both ex-ECG and CTCA were included. In this study, the interval of between performing ex-ECG and CTCA was limited to within 60 days. The following patients were initially excluded followings: patients who underwent both ex-ECG and CTCA at an interval more than 60 days (n = 418); those with unacceptable clinical information owing to incomplete medical records (n = 46); those who underwent percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) surgery within 60 days after ex-ECG and CTCA (n = 45); and those with unknown cardiovascular outcome due to loss to follow-up (n = 60). Finally, the remaining 442 patients were retrospectively enrolled in this study (Fig. 1). The mean interval between ex-ECG and CTCA was 7 ± 11 days. A total 296 patients (67.0%) underwent both exams at the same day. The ex-ECG was performed before CTCA in 68 patients (15.4%), and 18 patients (26.5%, 18/68) of them was positive result. The number of patient underwent CTCA first was 78 patients (17.6%), and 23 patients (29.5%; 23/78) had significant stenosis. From medical records at the first visit, information on age, height, sex, characteristics of chest pain, dyspnea, blood pressure, heart rate, and known cardiac risk factors including smoking, diabetes mellitus, hypertension, dyslipidemia, and chronic kidney disease were collected. Cerebrovascular accidents included transient ischemic attack, ischemic stroke and hemorrhagic stroke. Family history of CAD was defined as the incidence of CAD in first-degree relatives aged < 55 years in men and < 65 years in women. Institutional Review Board approval was obtained by local ethics committee and informed consent was waived.
Clinical assessment of obstructive coronary artery disease
In this study, 442 patients who presented with chest pain were divided according to typical angina, probable angina, and nonangina chest pain, according to the nature of chest pain, that is, whether chest pain was provoked by stress (exertion or emotion), and relieved by rest or sublingual nitrates within minutes.
Pretest probability (PTP) was classified as low-, intermediate-, and high-risks with reference to previous studies [1,13,14]. Based on sex, age, and chest pain characteristics, PTP provided information on the possibility of coronary artery stenosis ≥ 50% luminal diameter. If the possibility of coronary artery stenosis ≥ 50% was less than 15%, the PTP indicated low-risk. If the possibility ranged from 15% to 85% and if it was higher than 85%, PTP indicated intermediate, and high risks, respectively.
Exercise electrocardiography
Ex-ECG was conventionally performed by using the Bruce protocol. During the ex-ECG, the physician monitored continuously the patient’s condition and recorded blood pressure, heart rate, presence of chest pain, and electrocardiography changes in each stage and recovery 3 to 5 minutes after peak exercise. Ex-ECG was commonly terminated when the heart rate of the patients reached 85% of the predicted maximum heart rate. Other indications for terminating ex-ECG, based on the 2002 update of the ACC/AHA guidelines for exercise testing [1], were as follows: (1) moderate to severe angina; (2) signs of poor perfusion (cyanosis or pallor); (3) decrease of > 10 mmHg in systolic blood pressure from the baseline; (4) increasing nervous system symptoms (ataxia, dizziness, or near-syncope); (5) subject’s desire to stop; (6) sustained ventricular tachycardia; and (7) ST segment elevation greater than 1.0 mm (0.1 mV) in two or more contiguous precordial leads or more adjacent limb leads. Positive results of ex-ECG were defined as follows: (1) ≥ 1 mm ST segment elevation in two or more leads; (2) ≥ 1 mm depression of horizontal or down-sloping ST segment more than 60 milliseconds after the J-point. In addition, the Duke treadmill score (DTS) was calculated and stratified to low-, intermediate-, or high-risk group (defined as ≥ 5, +4 to –10, and ≤ –11, respectively). An inadequate ex-ECG result was defined as failure to reach 85% of the predicted maximal heart rate in accordance with age and sex.
Computed tomographic coronary angiography
CTCA was performed with a 64-slice multidetector computed tomography (CT) scanner (Brilliance 64, Philips Healthcare, Best, The Netherlands). Patients with heart rates higher than 70 beats per minute received 25 mg of oral propranolol before undergoing CTCA. A low osmolar nonionic contrast agent (90 to 100 cc, Ultravist 370, Berlex, Wayne, NJ, USA) was injected into the peripheral vein at flow rates between 3.5 and 4.5 mL/sec. After the contrast injection, a retrospective ECG-gated spiral scan was obtained that covered the region immediately beneath the aortic arch to the apex of the left ventricle during an inspiratory breath hold of 10 to 20 seconds. The scanning parameters were as follows: gantry rotation, 330 to 420 ms; and spiral imaging with retrospective ECG gating and dose modulation (ECG pulsing) at 750 to 850 mAs, 120 kV, and 0.75-mm slice thickness. For all scanners, a multisegment algorithm was used to reconstruct overlapping images that were typically at 75% of the cardiac cycle. Coronary artery calcium scores (CACSs) were measured without contrast by using semi-automated software (HeartBeat CS, Philips Medical Systems, Amsterdam, The Netherlands) that displayed colored spots representing calcium that were manually marked by the operator and automatically calculated in order to calculate a summed CACS. Total calcium scores were measured by using the Agatston method of noncontrast-enhanced CT scan. The presence of plaque in the coronary artery was observed at all segments of the coronary artery. The degree of coronary artery stenosis was divided according to whether stenosis was significant (at least one segment with luminal diameter narrowing ≥ 50%) or not (at least one segment with luminal diameter narrowing < 50%) based on CTCA results interpreted by radiologists. According to the number of epicardial vessels with significant stenosis, the conditions were classified as one-vessel disease (1VD), two-vessel disease (2VD), and three-vessel disease (3VD). Multivessel disease was defined as 2VD, 3VD, and left main disease.
Assessment of clinical long-term outcome
Patient follow-up data were obtained retrospectively from electronic records or telephone interview conducted by physicians and researchers. The mean patient follow-up duration was 2.8 ± 1.1 years. Information about all clinical events, including acute coronary syndrome (including unstable angina and myocardial infarction), revascularization (PCI or CABG), cardiac death, heart failure, stroke, and all-cause of death, was collected. Variant angina and stable angina without percutaneous coronary angiography were excluded in the events. Information about stroke and all-causes death was also collected but was not included in the cardiac events. If patients had two or more events, the first event was regarded as the clinical outcome.
Statistical analysis
Categorical values were computed with Pearson correlation method and expressed as number and proportion (%), and continuous variables were calculated with Student t test and presented as mean ± standard deviation. The analysis of baseline characteristics of ex-ECG parameters and CTCA parameters in all groups was performed to identify predictors of cardiac events. The predictive values of clinical outcome, including result of ex-ECG, significant coronary stenosis, and total CACS were evaluated by performing a binary logistic regression analysis. To examine cardiac event with CACS, cut-off value of CACS was obtained with the receiver operating characteristic (ROC) curve analysis. We chose CACS 40 as the cut-off value for prediction of cardiac events. For the comparison of two or more independent ROC curves, comparison of ROC curves as a statistical analysis described by Delong et al. [15] was performed with following significant variables: coronary artery stenosis ≥ 50%, presence of plaque, CACS, and DTS. Integrated discrimination improvement (IDI) and net reclassification improvement (NRI) were evaluated to determine the incrementally prognostic impact of ex-ECG and CTCA [16,17]. To identify independent predictive value of cardiac event and correct for confounding factors such as baseline characteristics, cardiovascular risk factors, ex-ECG and CTCA parameters, multivariable analysis and Cox regression model analysis were calculated. Event-free survival curves were obtained with the Kaplan-Meier method for cardiac event and compared using the log rank test. A p < 0.05 was considered statistically significant. Data were analyzed by using SPSS version 21.0 (IBM Co., Armonk, NY, USA), Medicalc version 13.3.3.0 (Medcalc, Ostend, Belgium), and SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Clinical characteristics
A total of 442 patients who underwent ex-ECG and CTCA between January 2007 and December 2013 in our hospital were selected for evaluation of chest pain by using their medical records. The mean age of the patients was 56.1 ± 10.2 years. Of the patients, 61.3% were men. The mean follow-up duration was 2.8 ± 1.1 years. The total number of clinical events, including all-cause death and stroke, were 29. Fifteen patients (15/442, 3.4%) experienced cardiac events during the follow-up. One patient (0.2%) died from acute myocardial infarction. Ten patients (2.3%) had acute coronary syndrome. Eleven patients (2.5%) underwent coronary revascularization. Among them, eight patients underwent PCI for acute coronary syndrome, three patients underwent PCI because of medically intractable angina pain. Three patients (0.7%) were hospitalized for heart failure. For noncardiac events, six cases of stroke (1.4%) and seven cases of noncardiovascular death (1.8%) were found. The causes of noncardiac deaths were organophosphorus intoxication, pancreatic cancer, hepatocellular carcinoma, pneumonia, acute leukemia, lung cancer, and stomach cancer.
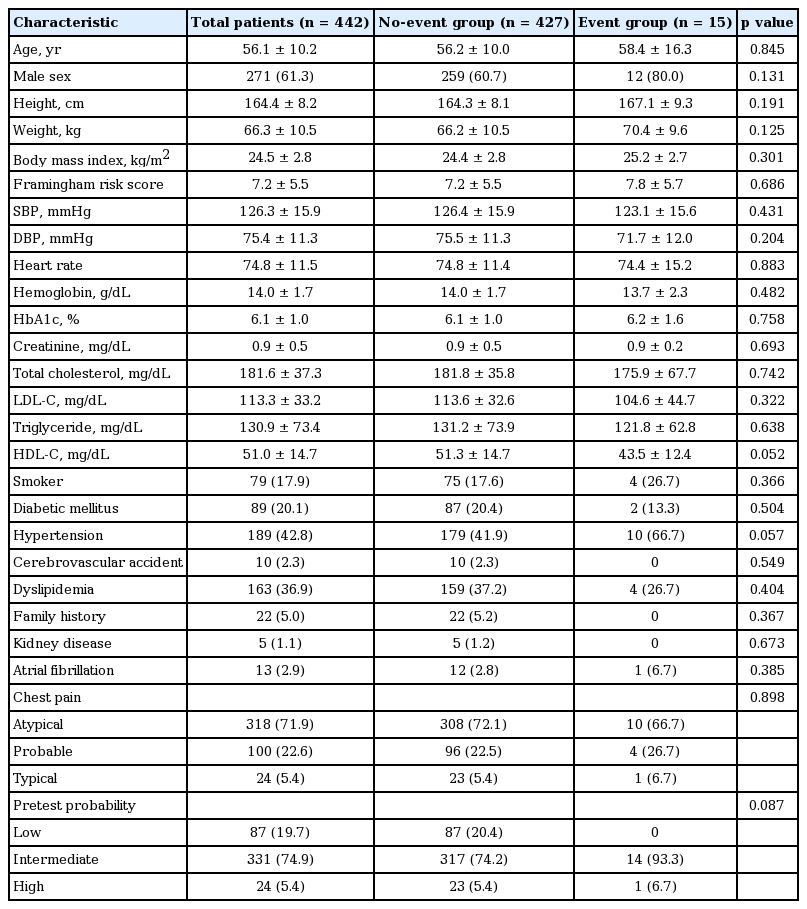
In the group of patients with cardiac events (event group), men were predominant, but no significant difference was observed compared to the group of patients without cardiac event (no-event group) (Table 1). No significant difference in baseline characteristics was observed between the two groups, as well as in chest pain profile (p = 0.898). The overall PTP composition did not differ between the groups. Of note, most of the patients were in the low and intermediate pretest probabilities (19.7% and 74.9%, respectively) (Table 1).
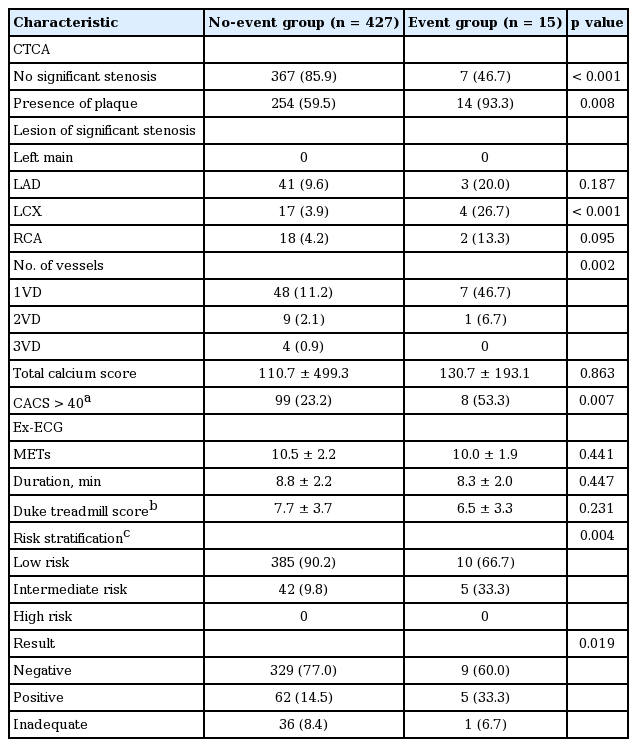
Computed tomographic coronary angiography as parameters of clinical outcome
As shown in Table 2, among 15 patients, seven cardiac events (46.7%) were observed, although the patients did not have significant stenosis. However, almost all the patients (93.3%) in the event group had coronary artery plaque. According to lesions of significant coronary artery stenosis, in the event group, three lesions (20.0%) were found in the left anterior descending coronary artery; four (26.7%) in the left circumflex coronary artery; and two (13.3%) in the right coronary artery. In the event group, seven patients (46.7%) had 1VD and one patient (6.7%) had 2VD. The mean total calcium score did not differ between the two groups (110.7 ± 499.3 in the no-event group and 130.7 ± 193.1 in the event group; p = 0.863). As a result, the number of patients with CACS > 40 statistically differed between the no-event (99/427, 23.2%) and event groups (8/15, 53.3%).
Exercise electrocardiography as parameters of clinical outcome
The results of the ex-ECG revealed no differences in mean values of metabolic equivalents, exercise duration, and DTS between the event and no-event groups (Table 2). Risk based on the DTS differed between the groups. The rate of intermediate risk (defined as −10 ≤ DTS ≤ +4) in the event group (33.3%) was higher than that in the no-event group (16.4%). None of the patients were at high risk (DTS ≤ −11). More patients in the event group than in the no-event group had positive results (5/15, 33.3% and 62/427, 15.5%, respectively; p = 0.019).
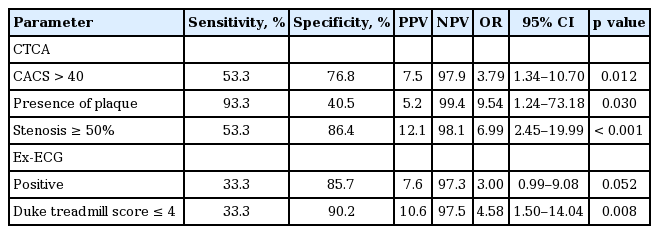
Clinical predictive values of exercise electrocardiography and computed tomographic coronary angiography
Among the CTCA parameters, CACS > 40, presence of plaque, and coronary artery stenosis ≥ 50% statistically differed between the no-event and event groups (Table 2). The three CTCA parameters had significant predictive values (Table 3). Presence of plaque showed high sensitivity, and negative predictive value as 93.3% and 99.4%. However, it had low specificity and positive predictive value. In addition, multivessel disease did not predict the occurrence of cardiovascular disease (data was not shown). A Kaplan-Meier survival curve showed that the rate of event-free survival was lower in the patients with than in those without coronary stenosis ≥ 50% on CTCA (Fig. 2). The cardiovascular event-free survival of the patients showed significant difference in terms of whether plaque and CACS > 40 were present (Fig. 2).

Kaplan-Meier plots for event-free survival for (A) coronary tomographic coronary angiography (CTCA) stenosis ≥ 50%, (B) presence of plaques, (C) coronary artery calcium score (CACS) > 40, and (D) Duke treadmill score (DTS) ≤ 4.
The ex-ECG parameters predicted cardiac events only in the subgroup of patients with DTS ≤ 4 (p = 0.008), whereas the ex-ECG parameters divided according to positive or negative results did not show any significant difference in odds ratio to predict the occurrence of cardiac events (Table 3). Event-free survival curves were divided significantly according a DTS ≤ 4 (Fig. 2).
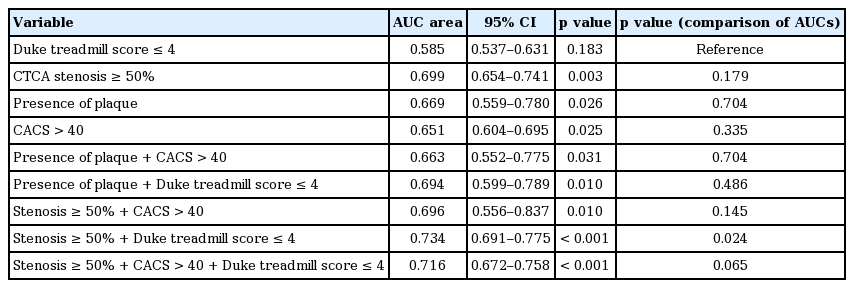
Comparison of predictive value between exercise electrocardiography and computed tomographic coronary angiography
For the comparison of predictive values between the CTCA and ex-ECG parameters, a ROC curve analysis of each parameter was performed (Table 4). The area under the curve (AUC) of the single or combined parameters of CTCA and ex-ECG were obtained and compared with DTS ≤ 4 as a reference value. Stenosis ≥ 50%, presence of plaque and CACS > 40 among CTCA findings were significant predictive values of clinical outcome in the comparison of ROC curve analysis. In the ROC curve analysis, stenosis ≥ 50% had the largest AUC in single parameters (AUC area, 0.699; 95% confidence interval [CI], 0.654 to 0.741; p = 0.003). However DTS ≤ 4 did not show statistical significance in the ROC curve analysis. When adding stenosis ≥ 50% to DTS ≤ 4, the combination predictor showed the maximal AUC area and significant difference compared to DTS ≤ 4 (p = 0.024). However, a combination of three parameters (including stenosis ≥ 50%, CACS > 40, and DTS ≤ 4) did not show significant difference in comparison of ROC curve analysis (Table 4, Fig. 3).

Comparison of the receiver operating characteristic curves with the computed tomographic coronary angiography and exercise electrocardiography results. DTS, Duke treadmill score; CACS, coronary artery calcium score.
Next, IDI and NRI as reclassification analysis, were performed to calculate the capacity of prediction of CTCA with ex-ECG compared to CTCA alone. The results indicated that a predictive value of combined stenosis ≥ 50% and DTS ≤ 4 trends toward better than that of stenosis ≥ 50% alone, but not significant (IDI, 1.10%, p = 0.369). Whereas the total NRI was −16.25%, these finding indicated that the prediction power of additional ex-ECG trends toward decreasing rather than increasing, albeit insignificant (p = 0.360).
To identify an independent predictor of cardiac event, the Cox regression analysis of variables was calculated and corrected with CTCA, ex-ECG findings, risk factors, and baseline characteristics (age, sex, smoking, diabetes, hypertension, cerebral infarction, dyslipidemia, and chronic kidney disease). Finally, only stenosis ≥ 50% was an independent predictive value among all parameters in the cox regression analysis (hazard ratio, 7.426; 95% CI, 2.686 to 20.525; p < 0.001) and was not influenced by the others (CACS > 40, p = 0.432, and DTS ≤ 4, p = 0.210).
Although DTS ≤ 4 was not significant in ROC curve analysis, it became significant and larger AUC area when adding stenosis ≥ 50% to DTS ≤ 4 in the analysis of comparison of ROC curves. On the other hand, in the analysis of NRI and IDI, those analyses did seem to improve prediction of outcome or have no adding impact of ex-ECG (DTS ≤ 4) on stenosis ≥ 50%. Therefore, stenosis ≥ 50% was the most valuable parameter of all the others from CTCA and ex-ECG parameters and may have sufficient ability to predict cardiac outcome.
DISCUSSION
The results of this study showed that (1) cardiac events were predictable when the patients had DTS ≤ 4, CACS > 40, presence of plaque, or coronary artery stenosis ≥ 50%; (2) the accuracy of the prognostic prediction of CTCA was better than that of ex-ECG; and (3) the predictive value of the combination of CTCA and ex-ECG was not superior to that of CTCA alone.
In the current study, the sensitivity and specificity of ex-ECG were slightly lower than those reported in previous studies [1,18-20]. These results may be related with the study population, which composed mostly of patients with low-to-intermediate PTP (94.6%). In clinical practice, ex-ECG and CTCA have been recommended in the intermediate PTP subgroup. Therefore, a subgroup analysis was performed for the intermediate PTP group. The number of patients in the intermediate PTP group was 331. In the intermediate PTP group, the subgroup with positive ex-ECG and DTS ≤ 4 revealed a statistically significant prediction of cardiac events. However, overall results of comparison between ex-ECG and CTCA were not different (data not shown).
In this study, the specificity and negative predictive value of CTCA were similar to those in the other studies that included patients with significant coronary artery luminal stenosis ≥ 50% [5]. Currently, based on functional study through conventional angiography, the definition of significant stenosis is shifting toward 75% luminal stenosis. Therefore, we analyzed cardiovascular outcome by using stenosis ≥ 75% as a CTCA parameter. Coronary artery stenosis ≥ 75% had higher specificity than stenosis ≥ 50% but showed low sensitivity (sensitivity, 13.3%; specificity, 96.3%). As the results, odds ratio of coronary artery stenosis ≥ 75% was not significant. Low population with high risk patients and low incidence of cardiac event might contribute to underestimate statistic power. On the other side, this analysis for coronary artery stenosis ≥ 75% supported that the test based on function, including ex-ECG, was inadequate to predict long term outcome because of low sensitivity, especially low- to intermediate-risk patients.
Maffei et al. [3] showed that ex-ECG had poor diagnostic accuracy in atypical chest pain and low- to intermediate-risk group, whereas CTCA was a suitable diagnostic tool. Similar with the previous study [3], our study composited patient with low- to intermediate-risk PTP, mostly, was showed that a combination of stenosis ≥ 50% and DTS ≤ 4 was more predictable than DTS ≤ 4 and had the largest AUC area in the analysis of comparison of ROC curve; however, stenosis ≥ 50% remained only a significant variable in Cox regression analysis and had no impact on the others variables.
In this study, we tried to determine the best parameter by using combining both tests. Pontone et al. [5] evaluated 681 patients with suspected CAD and demonstrated that the presence of significant coronary artery stenosis ≥ 50% was predictive of suspected CAD, but ex-ECG was only useful to predict outcome in positive CTCA results. Cho et al. [12] demonstrated that CTCA independently plays an important role in predicting major adverse cardiac events (MACEs) regardless of ex-ECG and that ex-ECG only predicted MACE in the moderate to severe coronary artery stenosis subgroup. Versteylen et al. [21] showed that the combination of CTCA and ex-ECG provided a high diagnostic yield to predict outcome in the intermediate risk group (10 years risk of cardiovascular events; range, 5% to 20%) according to Framingham risk score. However, the authors did not perform statistical analysis to compare ROC curves between CTCA and ex-ECG findings. Our study revealed that the AUC of the combined models was larger than that of the single model; especially the combination of stenosis ≥ 50% and DTS ≤ 4 had the largest AUC. However, the comparison analysis of AUC and reclassification analysis as NRI and IDI did not show any significant difference in the combined and single parameters except combination of stenosis ≥ 50% and DTS ≤ 4 compared to AUC of the reference. In the Cox regression analysis, stenosis ≥ 50% was only an independent predictor among all variables, these result indicates CTCA alone, especially coronary artery stenosis ≥ 50%, was enough to predict outcome rather than the combination of ex-ECG and CTCA in the low- to intermediate-risk population.
Firstly, the most important limitation was selection bias. This study is retrospective study. Therefore, all patients was not underwent ex-ECG and CTCA simultaneously. According to result of one exam, following test was performed selectively. To eliminate selection bias, we tried to analysis for 296 patients who undertaken both exams at the same day. Because only five patients with cardiac events were observed, the statistical analysis could not perform. We limited the interval of ex-ECG and CTCA within 60 days for reduce selection bias. As the result, a number of patients had undergone ex-ECG first and CTCA first were similar (68 [15.4%] vs. 78 [17.6%]) and those results were also not different. Second limitation was small cardiac event. These might be caused by population characteristics and relatively short follow-up duration. Only 5.4% of the patients in the current study had high-risk PTP. Because almost patients had low- to intermediate-risk, the low event rate and small sample size contributed to the limitation of this study. As a retrospective study, patients with highly suspicious CAD or a family history of CAD underwent PCI according to the physicians’ decision and only few events occurred. Therefore, the low event rate contributed to the low statistical power, especially in NRI and IDI analysis. It is well-known that the anti-platelet drugs and lipid-lowering drugs play a role on prevention of cardiovascular event. Next limitation is that we could not collect information on medicine of patients because of depending medical record in retrospective study. Forth limitation was several novel parameters of ex-ECG and CTCA were not assessed. Small and soft plaque rupture often contributes to acute coronary syndrome. Several reports demonstrated that plaque characteristic (soft, fibrous, calcified, or mixed type), location, extent, and distribution on CTCA was associated with poor cardiovascular outcome [8,22]. We only evaluated whether plaque was present or not. In the ex-ECG, after the introduction of the Duke score, blood pressure response, ischemic ST segment response, Athens QRS score, and M score showed improvement in clinical value [23]. However, the DTS, which is based on clinical symptoms, ECG findings, and exercise duration, is still the simplest and most popular parameter [23]. In future study, comparison of new parameters of ex-ECG and CTCA will be needed for precise prediction of clinical outcome.
In conclusion, DTS ≤ 4, CACS > 40, and coronary artery stenosis ≥ 50% were useful to predict cardiac outcome in the patients with low- to intermediate-risk who presented with chest pain. In particular, CTCA was better than ex-ECG in terms of predicting long-term outcomes. The combination of CTCA and ex-ECG was not superior to CTCA in terms of the predictive value. Thus, CTCA may be considered more valuable as a single test to predict cardiac outcome in low- to intermediate-risk populations.
KEY MESSAGE
1. Computed tomography coronary angiography (CTCA) was better than exercise electrocardiography (ex-ECG) for prediction of cardiovascular long-term outcome.
2. No evidence that combination of CTCA and ex-ECG was superior to CTCA was seen.
3. CTCA alone may be a valuable test to predict cardiovascular event in low to intermediate risk population.
Notes
No potential conflict of interest relevant to this article was reported.