Two-year clinical outcomes in stable angina and acute coronary syndrome after percutaneous coronary intervention of left main coronary artery disease
Article information
Abstract
Background/Aims
This study appraised the long term clinical outcomes of patients treated with percutaneous coronary intervention (PCI) for unprotected left main coronary artery (ULMCA) disease. There are limited data regarding long-term clinical outcomes after PCI for ULMCA disease.
Methods
From 2001 to 2011, a total of 448 patients who underwent PCI for ULMCA disease and had 2-year clinical follow-up, were analyzed. The study patients were divided into two groups: group I (stable angina pectoris [SAP], n = 60, 48 men, 62 ± 10 years) and group II (acute coronary syndrome [ACS], n = 388, 291 men, 64 ± 10 years). We evaluated clinical and angiographic characteristics and major adverse cardiac events (MACE) during 2-year clinical follow-up.
Results
Mean age of studied patients was 64 ± 10 years with 339 male patients. Average stent diameter was 3.6 ± 0.4 mm and stent length was 19.7 ± 6.3 mm. Stent implantation techniques and use of intravascular ultrasound guidance were not different between two groups. In-hospital mortality was 0% in group I and 7% in group II (p = 0.035). One-month mortality was 0% in group I and 7.7% in group II (p = 0.968). Two-year survival rate was 93% in the group I and 88.4% in the group II (p = 0.921). Predictive factors for 2-year MACE were hypertension, Killip class ≥ 3, and use of intra-aortic balloon pump by multivariate analysis.
Conclusions
Although in-hospital mortality rate was higher in ACS than in SAP, clinical outcomes during 2-year clinical follow-up were similar between SAP and ACS after PCI of ULMCA.
INTRODUCTION
Unprotected left main coronary artery (ULMCA) disease takes place in 5% of patients undergoing coronary angiography [1-3]. Coronary artery bypass graft (CABG) has been the standard of care for the management of ULMCA [4-6]. In contemporary practice, percutaneous coronary intervention (PCI) has become an alternative strategy in patients who have ULMCA disease because of current improvements in interventional techniques and adjunctive pharmacology [7-9]. There are, however, limited and conflicting data regarding long-term outcomes of PCI for ULMCA disease, especially in patients with acute coronary syndrome (ACS).
This study evaluated the long-term clinical outcomes of patients with stable angina and ACS, who were treated with PCI for ULMCA disease.
METHODS
Patients
From 2001 to 2011, a total of 448 consecutive patients (339 men, 64 ± 10 years) were included who underwent PCI for ULMCA disease with 2-year clinical follow-up at Chonbuk National University Hospital. The patients were divided into two groups: group 1 (stable angina pectoris [SAP], n = 60, 48 men, 62 ± 10 years) and group II (ACS, n=388, 291 men, 65 ± 10 years).
PCI procedure
Before the stent was inserted, patients underwent predilation inflation of undersized balloon for immediate stent implantation. Lesion lengths and vessel reference diameter were visually evaluated by the operators [10-12]. And then, intravascular ultrasound (IVUS) was used to exactly estimate the target lesion and stent placement; 83.3% (50/60) of cases in group I and 69.3% (268/388) of cases in group II. Stenting was performed using: bare metal stents (BMS) and drug eluting stents (DES). Types of DES were paclitaxel eluting stents (PES), sirolimus eluting stents, biolimus eluting stents, zotarolimus eluting stents (ZES), and everolimus eluting stents (EES). Intra-aortic balloon pump (IABP) was used when the systolic blood pressure was below 90 mmHg despite use of inotropic agents.
Definitions
Target lesion revascularization (TLR) was defined as a repeat intervention to manage luminal stenosis anywhere within the stent. Target vessel revascularization (TVR) was defined as any reintervention driven by lesions located in the treated vessel within and beyond the target lesion limits. Non-TVR was defined as any reintervention in vessels other than the target vessel [13]. Major cardiovascular adverse event (MACE) were defined as a case including TLR, TVR, Non-TVR, CABG, myocardial infarction (MI), and death after PCI procedure.
Statistical analysis
Data processing and statistical analysis was performed using the IBM SPSS version 21 (IBM Co., Armonk, NY, USA). A p < 0.05 was considered to indicate statistical significance. The confidence intervals (CIs) for our rates are 95%. Variables were compared using either the chi-square test. The variables that were found to be significant by univariate analysis were entered into multivariate analysis using Cox regression model.
RESULTS
Clinical characteristics
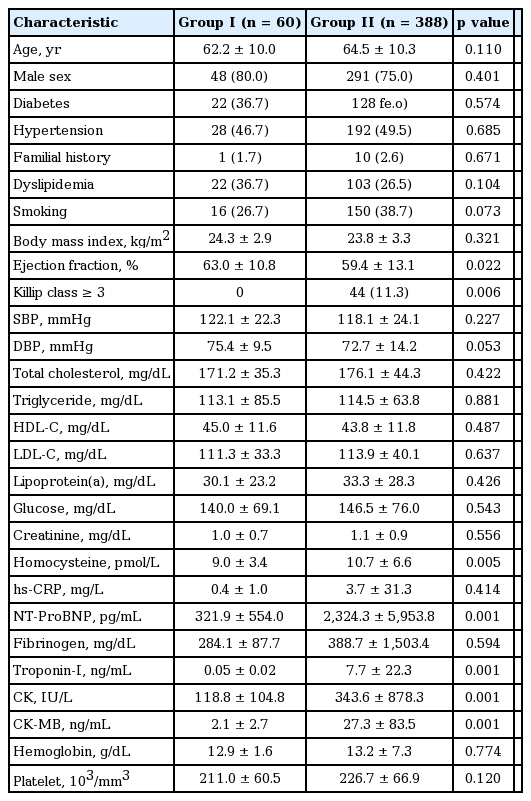
Baseline clinical characteristics of the patients are summarized in Table 1. Mean age was 64 ± 10 years with 339 male patients. Significant differences were found between two groups for ejection fraction, Killip class ≥ 3, homocysteine and the levels of N-terminal prohormone brain natriuretic peptide.
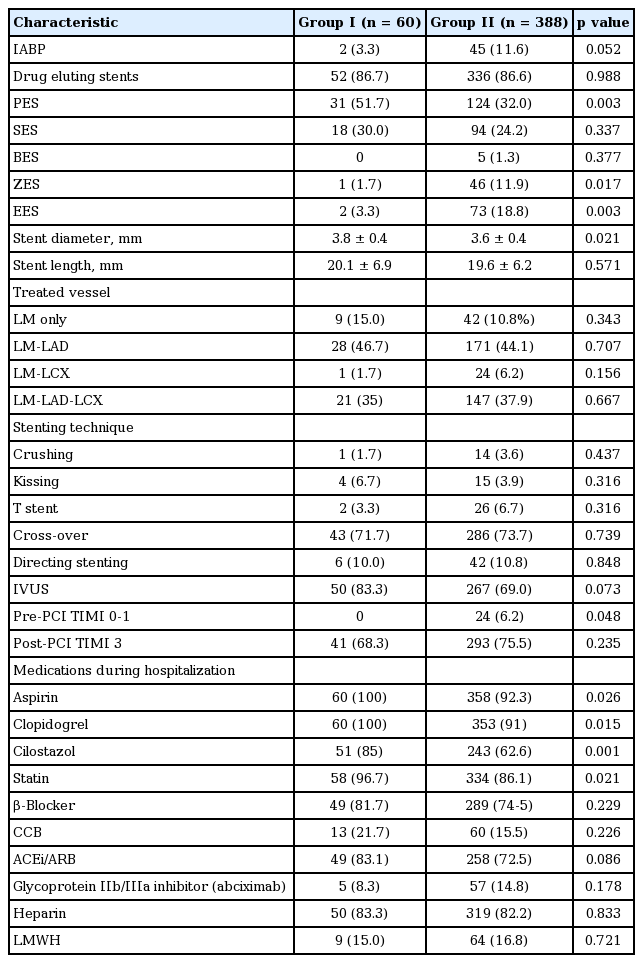
Coronary angiographic and procedural findings
Baseline angiographic and procedural data are represented in Table 2. Average stent diameter was 3.6 ± 0.4 mm and stent length was 19.7 ± 6.3 mm. Stent diameter in group I was longer than that in group II (3.8 ± 0.4 mm vs. 3.6 ± 0.4 mm, p = 0.021). Group I more often received PES (51.7% vs. 32.0%, p = 0.003) whereas group II more often received ZES (1.7% vs. 11.9%, p = 0.017) and EES (3.3% vs. 18.8%, p = 0.003). IABP was used in two patients in group I (3.3% vs. 11.6%, p = 0.052) while 45 patients in group II. Fifty patients in group I used IVUS (83.3% vs. 69.0%, p = 0.073). On the other hand 267 patients in group II used IVUS.
Medical treatment during hospitalization
Patients in group I received more often aspirin (100% vs. 92.3%, p = 0.026), clopidogrel (100% vs. 91%, p = 0.015), cilostazol (85% vs. 62.6%, p = 0.001), and statin (96.7% vs. 86.1%, p = 0.021) compared with patients in group II. Five patients in group I received abciximab whereas 57 in group II received abciximab (8.3% vs. 14.8%, p = 0.178).
In-hospital clinical outcomes
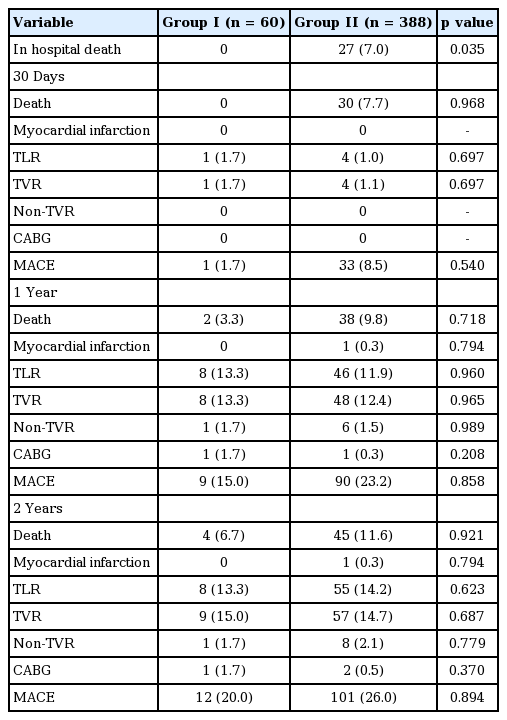
During hospitalization, group I more often received aspirin (100% vs. 92.3%, p = 0.026), clopidogrel (100% vs. 91%, p = 0.015), cilostazol (85% vs. 62.6%, p = 0.001), and statin (96.7% vs. 86.1%, p = 0.021) compared to group II. In-hospital death occurred more frequently inpatients in group II than in group I (0% vs. 7%, p = 0.035) (Table 3).
One-month clinical outcome
In group I there was no death. On the other hand, in group II there were 30 deaths (0% vs. 7%, p = 0.968). Other adverse events in group I consisted of TLR in one patient [10]. Four TLR also occurred in group II (1.7% vs. 1.0%, p = 0.697).
One-year clinical outcome
One-year survival rate was 96.7% (58/60) in the group I and 90.2% (350/388) in the group II (p = 0.718). CABG was carried out in two patients. One patient in group I was expired on the following day, right after operation. The other patient in group II still alive and follow-up regularly. The clinical outcomes of 12-month MACE between stable angina and ACS were similar (p = 0.858) (Fig. 1)
Two-year clinical outcome
Two-year survival rate was 93.3% (56/60) in the group I patients and 88.4% (343/388) in the group II patients (p = 0.921). On multivariate analysis, independent predictors of 2-year mortality were hypertension (hazard ratio [HR], 2.63; 95% CI, 1.38 to 5.00; p = 0.003), Killips class ≥ 3 (HR, 6.56; 95% CI, 2.94 to 14.67; p = 0.001), and use of IABP (HR, 6.564; 95% CI, 1.60 to 7.70; p = 0.002) (Table 4).
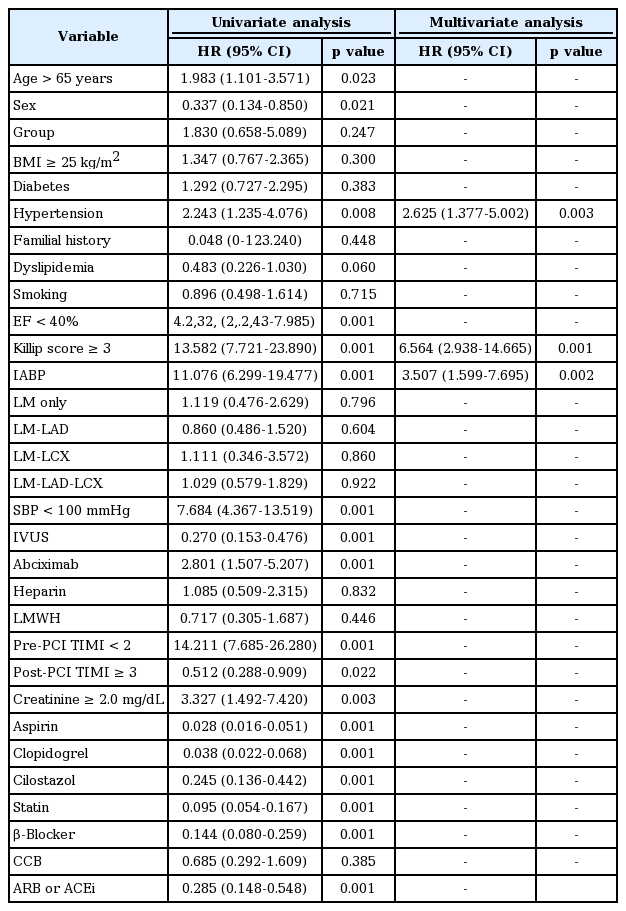
Univariate and multivariate analysis for predictors of 2-year mortality in patients with unprotected left main coronary artery disease
When we reanalyzed the data by including clinical diagnoses of ACS, 2-year MACE-free survival rate was not different among SAP, unstable angina pectoris (UAP), ST elevation myocardial infarction (STEMI), non-STEMI in patients with ULMCA disease (Fig. 2). Among ACS patients, however, 2-year MACE-free survival was significantly lower in STEMI compared to UAP (p = 0.012) (Fig. 3).

Two-year major adverser cardiac event (MACE)-free survivals was not different among stable angina pectoris (SAP), unstable angina pectoris (UAP), ST elevation myocardial infarction (STEMI), non-ST elevation myocardial infarction (NSTEMI) in patients with unprotected left main coronary artery disease. PCI, percutanouse coronary intervention.

In patients with acute coronary syndrome (unstable angina pectoris [UAP], ST elevation myocardial infarction [STEMI], and non-ST elevation myocardial infarction [NSTEMI]), 2-year major adverser cardiac event (MACE)-free survival rate was significantly lower in STEMI compared to UAP. PCI, percutanouse coronary intervention.
DISCUSSION
Significant ULMCA disease is a high-risk lesion that compromises blood flow to approximately 75% of the heart. Its incidence rate in undergoing PCI is 2.5% to 10%, and typically it exists with other significant narrowing of the coronary tree. The author compared of 2-year clinical outcomes in patients with stable angina and ACS after PCI of ULMCA disease. In general, ACS would show poorer prognosis compared with stable angina after PCI. In the present study, patients were divided into SAP and ACS groups. Interestingly 2-year clinical outcome of ULMCA disease after PCI was similar between the two groups.
The result of the present study is in general consistent with the previous studies on outcome of ULMCA disease with comparable 1-year mortality. In our study, major cardiovascular events developed 3.3% in patients with stable angina and 7.7% in patients with ACS. Ferrante et al. [14] reported major cardiac events developed in patients with ULMCA disease were 19.6% after DES implantation and 29.1% after BMS implantation. Sim et al. [15] reported major cardiac events developed 18% in patients with culprit left main coronary artery (LMCA) and 13.8% with non-culprit LMCA.
Ferrante et al. [14] study, out of 227 patients undergoing PCI for ULMCA. One hundred and forty-eight patients were treated with DES and 79 patients were treated with BMS. At 12 months follow-up, 29 patients (19.6%) with DES versus 23 patients (29.1%) with BMS died. Fajadet and Chieffo [16] revealed no distinction in the result of MACE and cerebrovascular events between PCI and CABG in ULMCA at 5-year clinical follow-up.
Naik et al. [17] recently presented a meta-analysis of PCI versus CABG in patients with ULMCA disease. This study also identified no difference in death or MACE or cerebrovascular events.
Sim et al. [15] compared outcome of culprit ULMCA (n = 256) and non-culprit ULMCA (n = 331) in patients with acute MI. Patients with culprit LMCA were younger and more likely to have Killip class ≥ 3, cardiopulmonary resuscitation at admission, low blood pressure, and increased heart rate. Patients with culprit LMCA had less complex lesions, more isolated LMCA disease, a lower rate of post-PCI thrombolysis in MI flow 3, and were more likely to receive DES. In both groups, PCI was more frequently used than CABG. Among patients receiving revascularization therapy, early and 12-month clinical outcomes were similar between PCI and CABG. Patients with culprit LMCA had significantly higher in-hospital mortality. However, clinical outcomes at 30 days and 12 months were similar between the two groups. On the contrary, Palmerini et al. [18] showed 2-year survival rate free from cardiac mortality and MI in patients with ACS was lower than that in patients with SAP (86% vs. 96%, p < 0.00001).
Regarding the choice between PCI and CABG for ULMCA disease, this study suggested that the ideal patient for PCI would have no hypertension, Killip score ≤ 2. The use of PCI for these select patients can improve cardiovascular outcomes and is a reasonable revascularization strategy.
The limitations of this study are that we did not show data on clinical follow-up beyond 2 years to document longer-term safety. The study is retrospective and is therefore subject to the limitations pertinent to this type of clinical investigation.
KEY MESSAGE
1. In patients with unprotected left main coronary artery (ULMCA) disease undergoing percutaneous coronary intervention (PCI), in-hospital mortality rate was higher in acute coronary syndrome (ACS) than in stable angina pectoris (SAP).
2. Two-year clinical outcome was similar between SAP and ACS. Therefore, PCI of ULMCA can be performed in patients with ACS effectively and safely.
3. Predictive factors of 2-year mortality were hypertension, Killip class ≥ 3 and use of intra-aortic balloon pump.
Notes
No potential conflict of interest relevant to this article was reported.