Clinical significance of rituximab infusion-related reaction in diffuse large B-cell lymphoma patients receiving R-CHOP
Article information
Abstract
Background/Aims
This study was to evaluate the clinical significance of infusion-related reaction (IRR) of rituximab in diffuse large B-cell lymphoma (DLBCL) patients who received R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone) as a first-line chemotherapy.
Methods
The medical records of 326 patients diagnosed with DLBCL were re trospectively analyzed. Both doctor’s progress records and nursing records were reviewed. IRR was graded according to the National Cancer Institute Common Terminology Criteria.
Results
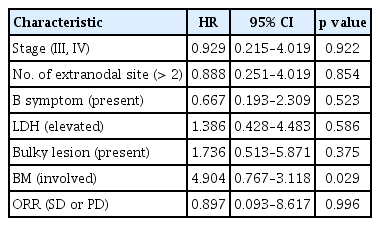
IRR was not associated with overall survival (OS) or progression-free survival (PFS) of DLBCL patients as compared to those who did not have IRR (OS: median 78.0 months vs. 69.0 months, p = 0.700; PFS: median 65.4 months vs. 64.0 months, p = 0.901). IRR grade did not affect OS or PFS. B symptoms was independently associated with IRR (hazard ratio [HR], 1.850; 95% confidence interval [CI], 1.041 to 3.290; p = 0.036). Further, bone marrow involvement was independently associated with re-IRR (HR, 4.904; 95% CI, 0.767 to 3.118; p = 0.029).
Conclusions
Our study shows that IRR of rituximab is not associated with OS or PFS of DLBCL patients who received R-CHOP. Furthermore, our study suggests a need for more careful observation for IRR in patients with B symptoms or bone marrow involvement.
INTRODUCTION
Diffuse large B-cell lymphoma (DLBCL) is the most common histologic subtype of non-Hodgkin lymphoma (NHL), accounting for approximately 30% of patients with NHL [1-3]. R-CHOP (comprising rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone) is the standard treatment for DLBCL [4-8]. Rituximab targets the CD20 protein, which is primarily found on the surface of B-cells and is present on many lymphoma cells [9].
Antibody-dependent cellular cytotoxicity (ADCC) is the main mechanism of action of rituximab. ADCC is thought to induce lysis of lymphoma cells via release of cytotoxic mediators in natural killer (NK) cells and macrophages or by direct phagocytosis in macrophages [10]. Further, rituximab has been shown to activate NK cells, macrophages, and neutrophils that eliminate B-cells in vitro [11-13]. The T-cell, macrophage, and stromal microenvironments in B-NHL have been extensively investigated, with many studies indicating that patients with enhanced host immune responses may have better clinical outcomes [14].
The infusion-related reaction (IRR) induced by rituximab is one of the most frequently encountered adverse reactions in clinical practice [15]. Most reactions to chemotherapeutic agents are consistent with type 1 hypersensitivity caused by the immunoglobulin E-mediated release of histamines, also which is known decrease of cancer risk by expelling carcinogens. However, IRR induced by rituximab is related to cytokine release [16,17]. Recently, small numbered studies suggested that IRR of rituximab is related to its therapeutic effect, with better tumor destruction seen in patients who experienced IRR [16,18]. Based on previous reports, we hypothesized that IRR of rituximab may be associated with ADCC, which improves the therapeutic efficacy of rituximab. As previous reports were based on small numbers of patients, the clinical significance of IRR of rituximab in DLBCL patients is not yet fully evaluated. Thus, we investigated the clinical significance of IRR of rituximab in DLBCL patients who received R-CHOP as a first-line chemotherapy.
METHODS
Patients
We analyzed DLBCL patients who were diagnosed at Seoul National University Hospital (SNUH) between January 2005 and May 2012 from our consecutive database. The patients who had met the following criteria were enrolled: (1) histologically confirmed DLBCL according to World Health Organization criteria [19] (histologic examination was done by specialized hematopathologists (Y.K. Jeon and C.W. Kim); (2) received R-CHOP as first-line chemotherapy; (3) staging work-up included computed tomography (CT) scans, 18F-2-fluoro- 2-deoxyglucose-positron emission tomography/CT, and bone marrow (BM) examination; and (4) We exclude the patients with initial central nervous system involvement, human immunodeficiency virus-associated DLBCL, and intravascular large B-cell lymphoma histology.
The medical record of each patient was reviewed with respect to age at diagnosis, sex, bulky lesion (defined as a longest diameter of nodal mass is more than 10 cm in size or a widening of the mediastinum by more than one-thirds), Eastern Cooperative Oncology Group (ECOG) performance status, lactate dehydrogenase (LDH) levels, Ann Arbor stage, number of extra-nodal sites, and International Prognostic Index [20].
Rituximab infusion
All patients received 375 mg/m2 rituximab as an intravenous infusion on day 1 of each chemotherapy cycle, followed by combination chemotherapy. Thirty minutes before rituximab infusion, patients were given 650 mg acetaminophen and 4 mg of the antihistamine pheniramine via intravenous infusion. We did not use steroid premedication due to medication prednisolone.
Rituximab mixed with 500 mL normal saline was administered at an initial rate of 50 mg/hr, and the rate was increased by 50 mg/hr every 30 minutes until it reached 400 mg/hr. If no IRR occurred during the first cycle, rituximab infusion during the second and all subsequent cycles started at a rate of 100 mg/hr followed by increases of 100 mg/hr every 30 minutes up to 400 mg/hr for up to 6 to 8 cycles.
Medical records and grading of infusion-related reactions
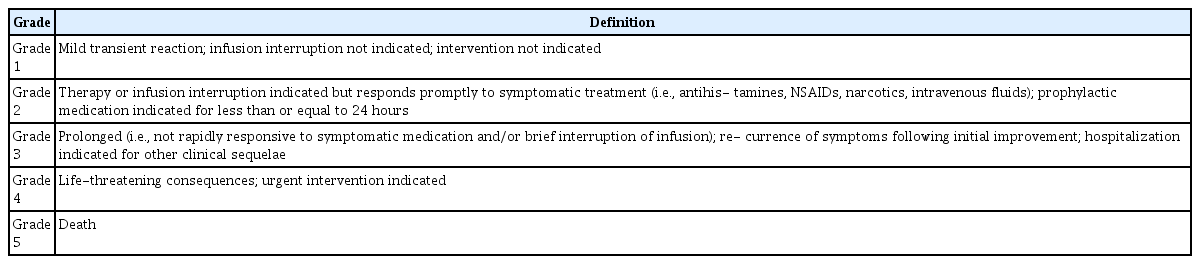
The IRR during first rituximab infusion was included. For each rituximab infusion, both doctor’s progress records and nursing records were reviewed. Any change of infusion rate, development of IRR, characteristics of IRR, the exact time and infusion rate of rituximab, and vital signs were recorded in detail. Furthermore, in our hospital there is system which monitoring of adverse drug reaction, which we used. IRR was graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events version 4.0. Definitions of each grade are shown in Table 1. We reviewed IRR relapse rates, the total number of IRR episodes in each patient, and symptoms.
Statistical analysis
Statistical analyses of categorical variables were performed using Pearson’s chi-square tests. Progression- free survival (PFS) was defined as the interval between the date of R-CHOP to the date of disease progression, any cause of death, or the last follow-up visit. Overall survival (OS) was measured from the initiation date of R-CHOP to the date of any cause of death or the last follow-up visit. The median duration of PFS and OS was calculated using the Kaplan-Meier method. Survival comparisons between groups were performed using log-rank tests. The Cox proportional hazards regression model was used for multivariate analyses to assess the effect of patient characteristics and other prognostic factors. Two-sided p values less than 0.05 were considered statistically significant. All analyses were performed using SPSS software for Windows version 19 (IBM Co., Armonk, NY, USA). The Institutional Review Board (IRB) of SNUH approved the study protocol (IRB approval number H-1308-030-510). We also adhered to the Declaration of Helsinki regarding biomedical research involving human subjects. Informed consents were waived because of retrospective study.
RESULTS
Patient characteristics
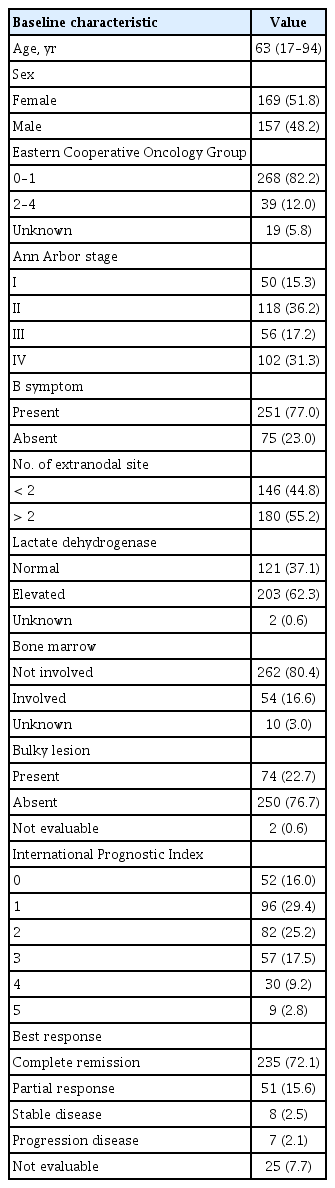
Patient characteristics are summarized in Table 2. A total of 326 DLBCL patients who received first-line R-CHOP were analyzed. The median age was 63 years (range, 17 to 94). One hundred and fifty-eight patients (48.5%) were in advanced stages of disease (stages III and IV). Two hundred and three patients (62.3%) had elevated LDH levels at the time of diagnosis. Seventy-four patients (22.7%) had bulky lesions.
Infusion-related reactions
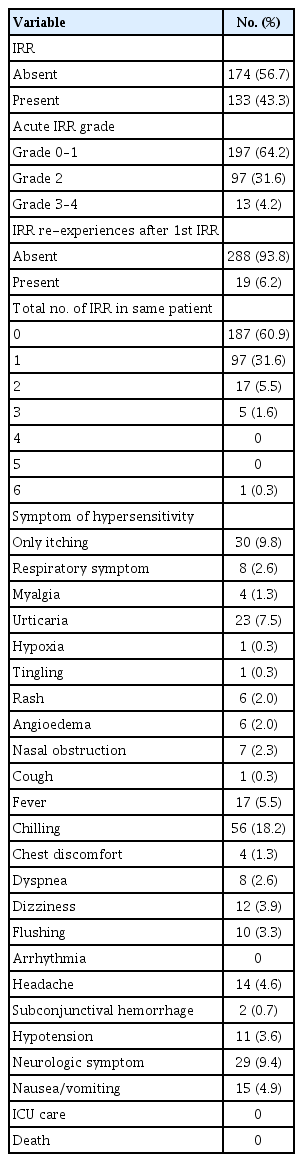
One hundred and thirty-three patients (43.3%) experienced one or more than IRR event(s) (Table 3). Twelve patients had Grade 3 IRR and one patient had Grade 4 IRR. Fifty-six patients (18.2%) experienced chills, 15 patients (4.9%) experienced nausea and vomiting, and 12 patients (3.9%) experienced hypoxia and hypotension. No patient required intensive care unit admission or died from IRR. Nineteen patients (6.2%) experienced two IRR re-experiences. Twenty-three (7.4%) experienced more than two IRR re-experiences.
Risk factors for IRR and IRR re-experience
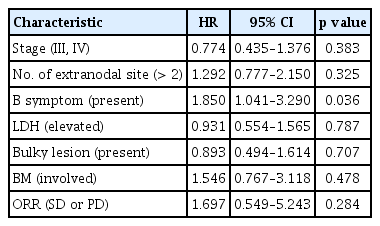
Among the clinical parameters investigated, B symptoms were significantly associated with the incidence of IRR (hazard ratio [HR], 1.850; 95% confidence interval [CI], 1.041 to 3.290; p = 0.036). However, lymphoma stage, the number of extra-nodal lesions and LDH had no relation with the incidence of IRR. Furthermore, response rate of R-CHOP was not different in IRR and non-IRR groups (HR, 1.697; 95% CI, 0.549 to 5.243; p = 0.284) (Table 4). BM involvement was significantly associated with the incidence of IRR re-experience (HR, 4.904; 95% CI, 0.767 to 3.118; p = 0.029). B symptoms, lymphoma stage, extra-nodal number, and treatment response had no relation to the incidence of IRR re-experiences (Table 5).
Clinical outcome and correlation with IRR
OS was not significantly longer in patients who experienced IRR compared to those who did not experience IRR (median, 67.5 months vs. 78.0 months, p = 0.975) (Fig. 1). PFS was also not significantly different between these two groups (median, 65.4 months vs. 63.0 months, p = 0.770) (Fig. 2). Also, IRR is not associated with the therapeutic response rate (p = 0.361). OS was not significantly different in patients with IRR grades of 0 or 1, and those with IRR grades of 2 and 3, or 4 (median, 79.2 months vs. 65.7 months vs. 61.9 months, p = 0.848) (Fig. 3). PFS was also not significantly different between these three groups (median, 65.6 months vs. 63.7 months vs. 48.0 months, p = 0.388) (Fig. 3). OS was not significantly different between patients who re-experienced IRR and those who did not (median, 78.9 months vs. 48.4 months, p = 0.255). However, PFS was significantly different between these two groups (median, 65.8 months vs. 35.4 months, p = 0.046).

Kaplan-Meier plots of progression-free survival (PFS) by infusion-related reaction (IRR) and non-IRR.

Kaplan-Meier plots of overall survival (OS) and progression-free survival (PFS) by infusion-related reaction (IRR) grades.
In IRR group analysis, there was not different between BM involvement and not BM involvement (median OS, 68.2 months vs. 61.5 months, p = 0.491). However, there was different between B symptom and not B symptom (median OS, 72.8 months vs. 53.3 months, p = 0.019).
DISCUSSION
Our study showed that there was no association between IRR of rituximab and OS or PFS. Furthermore, there was no association between IRR of rituximab and response rate to R-CHOP. B symptoms was independently associated with IRR of rituximab. Therefore, patients with B symptoms should be more intensively monitored for IRR of rituximab.
Mild-to-moderate reactions are relatively common (up to 77%) particularly during the first infusion of rituximab. The reactions are immediate, often occurring within the first few minutes of the first infusion [17]. As our results show that IRR experience is related to B symptoms, during a challenge it may help to decide which patients might benefit from a reduction in the infusion rate of rituximab by half (from 100 to 50 mg/hr) [17].
Rituximab is thought to induce lysis of lymphoma cells through complement-mediated cytolysis, ADCC, and direct induction of apoptosis. Several previous reports suggest a link between IRR of rituximab and its therapeutic efficacy. Byrd et al. [16] reported that all patients who developed a unique set of severe IRRs subsequently showed a rapid decrement in circulating tumor cell load. Also, Winkler et al. [15] reported that serum levels of interleukin 6 and tumor necrosis factor α peaked after the onset of infusion, peak levels were accompanied by maximum clinical side effects, and lymphocyte counts dropped to 50% to 75% of baseline values within 12 hours after infusion onset. Unlike above reports from small numbers of patients, our results from a larger number of DLBCL patients showed no association between IRR of rituximab and the therapeutic efficacy of rituximab. Recent reports suggest that IRR is not associated with the therapeutic efficacy of rituximab [21]. The IRR of rituximab was related only to B symptoms in our study. It is otherwise that previous report result which reported that BM involvement is associated with IRR [21].
Further, B symptoms are known for poor prognosis [22-24]. Also, our study showed that patients with B symptom had significantly poor OS in univariate analysis (p < 0.001). However, our study also showed that the patients with IRR of rituximab did not have poorer OS than the patients without IRR of rituximab. Considering the above, B symptom itself are not related to prognosis of IRR. Hong et al. [21] reported that patients with DLBCL who experienced ≥ Grade 2 IRR had reduced event-free and OS rates compared to those who did not experience IRR of rituximab. However, our study showed that IRR grade is not associated with therapeutic prognosis.
Furthermore, in the study of Hong et al. [21], they reported approximately 18% of IRR of rituximab in DLBCL. However, our study showed an unexpectedly high rate of IRR (43%). In our study, we did not use premedication steroid because our chemotherapy include prednisolon 100 mg, as a result, our study showed an unexpectedly high rate of IRR due to the non-use of premedication steroid.
Our study showed that although, OS was not significantly different between patients who re-experienced IRR and those who did not (78.9 months vs. 48.4 months, p = 0.255). However, PFS was significantly different between these two groups (p = 0.046). BM involvement was significantly associated with the incidence of IRR re-experience (p = 0.029). BM involvement is known for poor prognosis [22-24]. Our study showed that patients with BM involvement had significantly poor PFS in univariate analysis (p = 0.02). Van der Kolk et al. [25] recently reported that complement activation plays a key role in the side effects of rituximab treatment. Additionally, this study also reported that complement activation was only observed in patients with BM involvement [25]. Furthermore, Van der Kolk et al. [25] claimed that patients with BM involvement might have higher levels of circulating tumor cells than patients without BM involvement. Several other reports suggest that the incidence and severity of side effects associated with the first dose of rituximab significantly depend on higher circulating tumor lymphocyte counts at baseline in patients with a variety of other lymphoid neoplasms, such as chronic lymphocytic leukemia and B-cell chronic lymphocytic leukemia [15,16,26]. Although we could not evaluate blood lymphocytes in this study as all patients had DLBCL without leukemic manifestations, we observed that the BM involvement is associated with rituximab-related re-experience IRR. This is consistent with our observation that rituximab-related re-experience IRR by itself affect IRR-related treatment efficiency.
Although, we could not check changes in cytokine during IRR. To the best of our knowledge, our study is the largest study with enough statistical power for evaluating the clinical significance of IRR of rituximab in DLBCL patients receiving R-CHOP. Previous reports studied smaller population sizes (n = 17 and n = 5) with other B malignancies such as B-cell prolymphocytic leukemia and transformed NHL [15,16]. Moreover, all the patients in our study received rituximab infusion in the same protocol in a single center. However, there are several limitations to our study. It is important to note that all the data in our study were collected retrospectively. We reviewed IRR according to doctor’s progress records and nursing records, so there are possibility of underestimation of lower grade IRR, variation according to the investigators. Also, the levels of cytokines, neutrophils, or macrophages were not evaluated during IRR of rituximab.
In conclusion, the incidence of B symptoms were independently associated with IRR of rituximab. Our study shows that IRR of rituximab is not associated with OS or PFS in DLBCL patients who received R-CHOP. Further, BM involvement is associated with re-IRR of rituximab. Therefore, patients with B symptoms and BM involvement should be more intensively monitored for IRR of rituximab.
KEY MESSAGE
1. Infusion-related reaction (IRR) of rituximab is not associated with overall survival or progression-free survival of diffuse large B-cell lymphoma patients who received R-CHOP (comprising rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone).
2. Our study suggests a need for more careful monitoring for IRRs in patients with B symptoms or bone marrow involvement.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported by grants from the Innovative Research Institute for Cell Therapy, Republic of Korea (A062260).