Effects of aspirin resistance and mean platelet volume on vascular access failure in hemodialysis patients
Article information
Abstract
Background/Aims
Maintaining the patency of vascular access (VA) in hemodialysis (HD) patients is important and can be life-saving. We investigated the effects of aspirin resistance and mean platelet volume (MPV) on VA failure in HD patients.
Methods
We enrolled 163 patients on maintenance HD. VA failure was defined as thrombosis or a decrease of > 50% of the normal vessel diameter, as revealed by angiography.
Results
Aspirin resistance was observed in 17 of 109 patients in whom this parameter was measured, and was not significantly associated with VA failure (p = 0.051). The mean MPV was 9.15 ± 0.05 fL. The 163 patients were grouped by the median MPV value (9.08 fL) at baseline; patients with higher MPVs (n = 82) had lower platelet counts (p = 0.002) and albumin levels (p = 0.009). During 34 months of follow-up, 65 VA failures (39.9%) occurred. The Kaplan-Meier curve revealed significant differences between the two groups in terms of cumulative VA failure (54.1% vs. 35.3%, p = 0.018). On multivariate analysis, the MPV (hazard ratio [HR], 1.794; 95% confidence interval [CI], 1.066 to 3.020; p = 0.028), platelet count (HR, 1.003; 95% CI, 1.001 to 1.006; p = 0.01), and smoking status (HR, 1.894; 95% CI, 1.019 to 3.519; p = 0.043) independently predicted VA failure.
Conclusions
A high MPV was associated with an increased risk of VA failure, whereas aspirin resistance showed only a weak association. The MPV may predict VA survival in HD patients.
INTRODUCTION
Vascular access (VA) failure is a major problem in dialysis patients and maintenance of vascular patency can be life-saving. Recently, both the costs of, and morbidity associated with, management of VA failure in hemodialysis (HD) patients has increased [1]. The main cause of VA failure is outflow venous stenosis caused by vascular intimal hyperplasia and thrombosis, in turn triggered by platelet activation, endothelial cell injury, and vascular smooth muscle cell proliferation [2,3]. Antiplatelet therapy has been suggested to prevent VA failure [4]. However, the effectiveness of aspirin remains controversial [5-7]. Aspirin resistance is a well-known feature of patients with chronic renal failure, especially those requiring dialysis [8]. Thus, aspirin ineffectiveness may reflect aspirin resistance.
The mean platelet volume (MPV) is a known marker of atherosclerotic disease, as revealed in several epidemiological studies [9-12]. The MPV is an independent risk factor for myocardial infarction [13]. Atherosclerosis and coronary heart disease are very common in patients with end-stage renal disease (ESRD) [14,15]. Therefore, the MPV may be associated with cardiovascular disease in HD patients; in such patients, the MPV may be more affected by changes in extracellular fluid volume and composition than is the case in the general population. A relationship between the MPV and platelet aggregability may explain the association of MPV with coronary heart disease [16,17]. Previous studies showed that large platelets were more reactive than small platelets [18]; thus, a high MPV may be associated with VA failure. However, few studies on the effect of MPV on VA patency in HD patients have appeared. We thus investigated the effects of aspirin resistance (where aspirin serves as an antiplatelet agent) and the MVP (an indicator of platelet activation) on VA failure in HD patients.
METHODS
Study population
A total of 163 patients, with ESRD undergoing HD at Chuncheon and Kangnam Sacred Heart Hospital during January 2011, were included. All patients were ≥ 18 years of age, and had undergone HD two or three times weekly for > 3 months via an arteriovenous fistula (AVF) or arteriovenous graft (AVG). The exclusion criteria were: active bleeding or bleeding requiring transfusion within the prior 4 weeks, disseminated intravascular coagulation, any cardiovascular or cerebrovascular event within the past 4 weeks, any critical illness requiring an intensive care unit stay, and the use of permanent or temporary HD catheters. The study complied with all relevant tenets of the Declaration of Helsinki and was approved by our Institutional Ethics Committee (Institutional Review Board, IRB approval no. 2009-10-74). Written informed consent was obtained from all patients.
Data collection
We recorded age, sex, body mass index, smoking status, duration of dialysis, comorbidities, any previous history of cardiovascular disease and/or VA failure, and current medication use, including antiplatelet agents. We collected dialysis records and the following biochemical data: complete blood cell count; blood urea nitrogen level; and the levels of serum creatinine, albumin, calcium, phosphorus, uric acid, intact parathyroid hormone, calcidiol, lipids, hemoglobin A1c, and C-reactive protein. Predialysis arterial blood samples were also obtained. Complete blood cell counts were measured using an ADVIA 2120 instrument (Bayer Health Care Diagnostic, Tarrytown, NY, USA). To evaluate aspirin resistance, antiplatelet effects were assessed using a VerifyNow device (Accumetrics, San Diego, CA, USA). Aspirin resistance was defined as an aspirin resistance unit (ARU) score > 550. VA failure was defined as thrombosis or a decrease > 50% in the normal vessel diameter and ≥ 50% in the luminal diameter on angiography, accompanied by abnormal clinical findings.
Statistics
Continuous variables are presented as means with standard deviations and categorical variables as numbers with percentages. Continuous variables were compared using the independent samples t test or the Wilcoxon rank-sum test. Categorical variables were compared using the Pearson chi-square test. Survival curves were plotted using the Kaplan-Meier method. Univariate and multivariate Cox’s proportional hazard models were employed to determine the relationships between clinical and biochemical variables, and VA failure. All calculations were performed using SPSS software version 18.0 (SPSS Inc., Chicago, IL, USA) and a p < 0.05 was considered significant.
RESULTS
Baseline characteristics
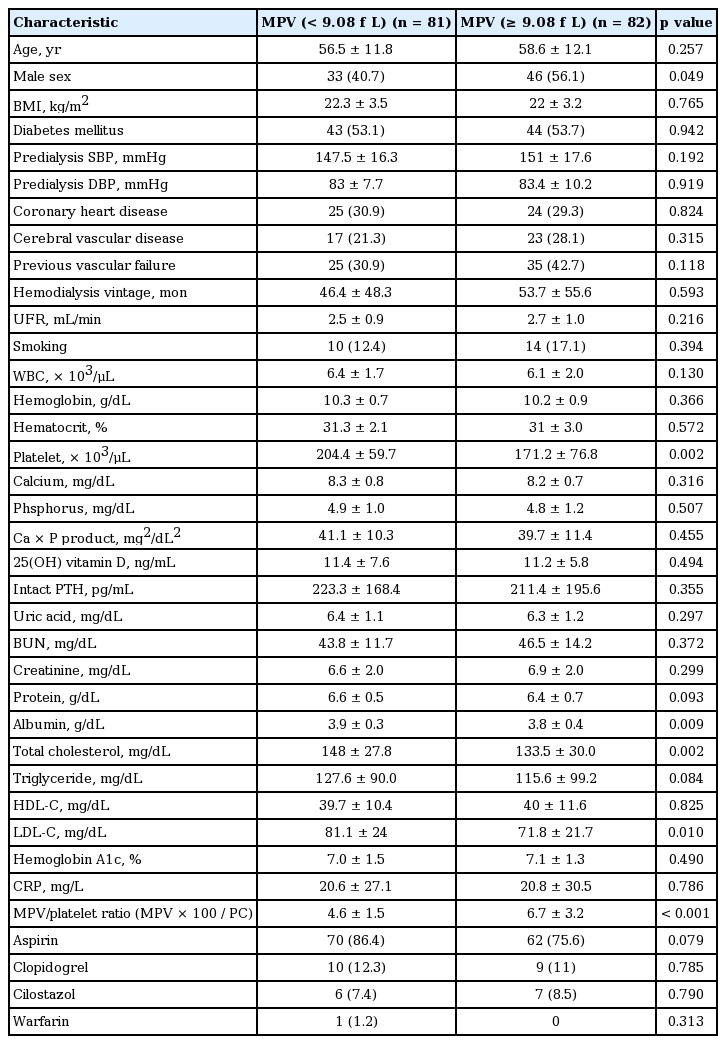
The 163 subjects were divided into two groups by the median MPV (9.08 fL). Demographic, clinical, and biochemical characteristics are listed in Table 1. The mean patient age was 57.6 ± 12.0 years and 79 (48.5%) were male; 87 (53.4%) had diabetes mellitus and the mean dialysis duration was 50.1 ± 52.1 months. Higher MPVs were more common in males with lower platelet counts (PCs). Lower albumin, total cholesterol, and low density lipoprotein cholesterol levels were seen in those with higher versus lower MPVs. The MPV/platelet ratio was higher in the higher MPV group (4.6 ± 1.5 vs. 6.7 ± 3.2, p < 0.001).
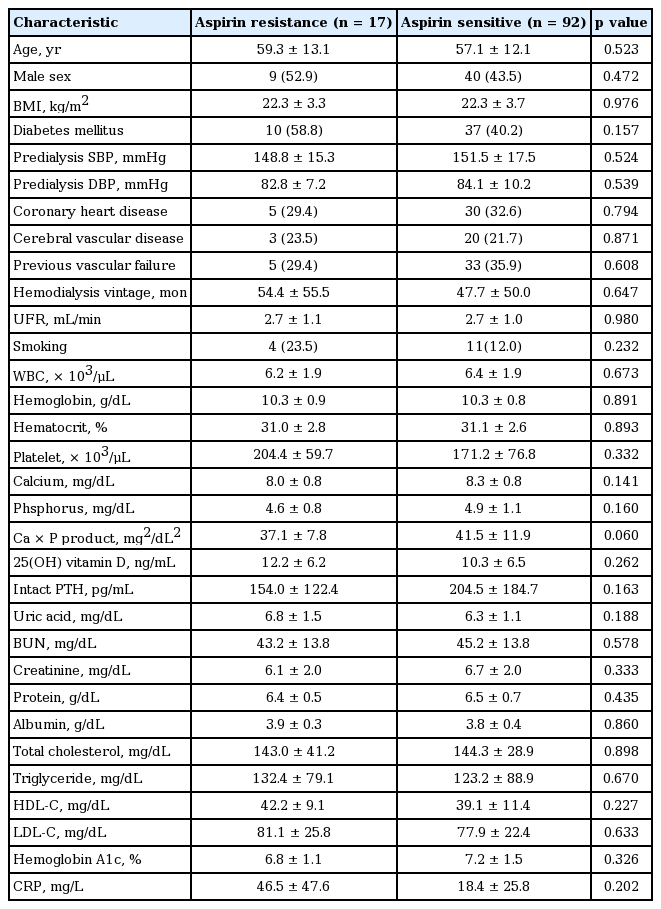
Aspirin resistance was observed in 17 of 109 patients (15.6%) for whom these data were available. We divided all patients into two groups by aspirin resistance status (Table 2); the groups did not differ significantly in demographic characteristics.
Clinical outcomes
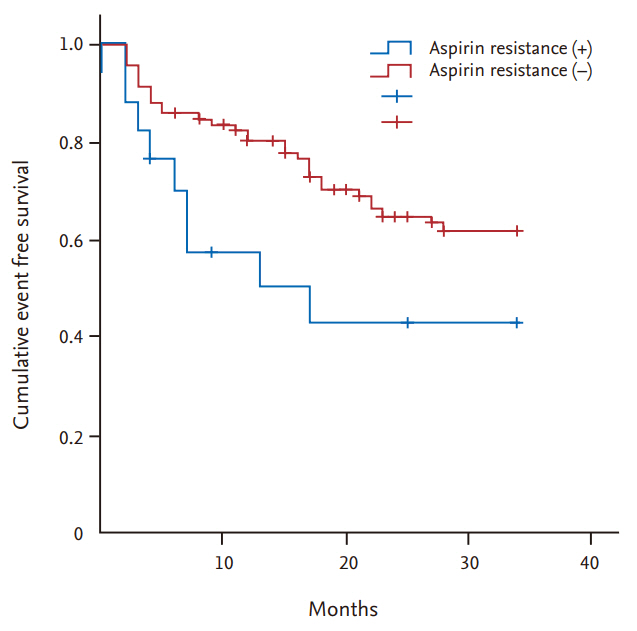
Ove a follow-up period of 34 months, 65 VA failures occurred, of which 41 were in aspirin-resistant patients. Fig. 1 shows the Kaplan-Meier curves for VA failures by aspirin-resistance status. The two groups did not differ significantly in terms of the cumulative VA failure rate (57% vs. 38.2%, log-rank test, p = 0.051). Fig. 2 shows Kaplan-Meier curves for VA failure by MPV status. A high MPV was associated with a high cumulative VA failure rate (54.1% vs. 35.3%, p = 0.018).
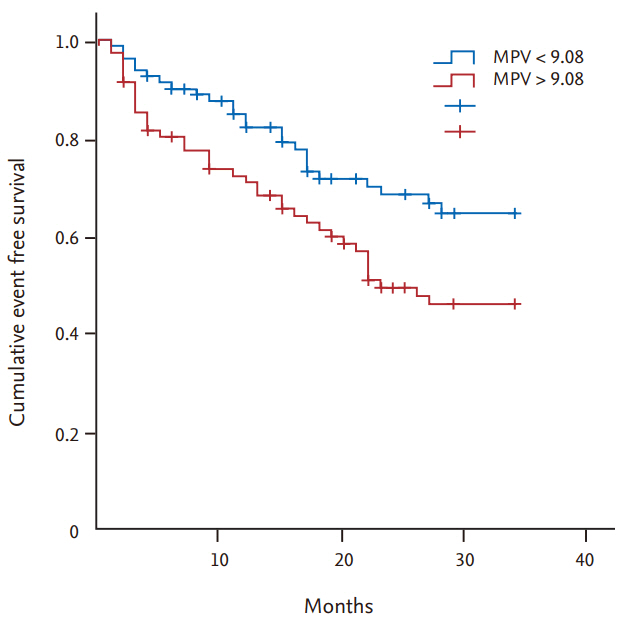
Kaplan-Meier curves for vascular access failure according to mean platelet volume (MPV) (p = 0.018).
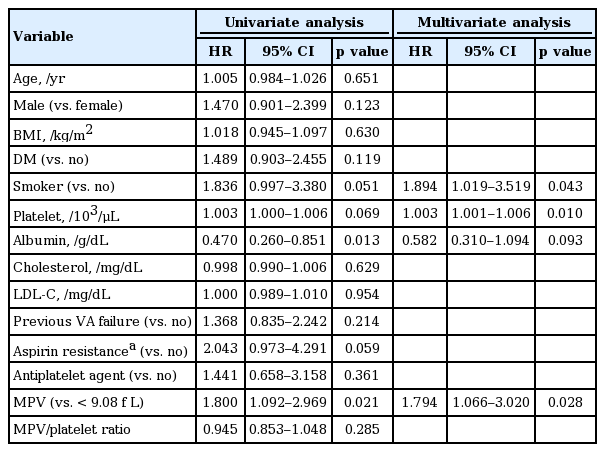
Cox’s proportional hazard models were used to define factors predictive of VA failure (Table 3). On univariate analysis, the serum albumin level (hazard ratio [HR], 0.470; 95% confidence interval [CI], 0.260 to 0.851; p = 0.013) and the MPV (HR, 1.800; 95% CI, 1.092 to 2.969; p = 0.021) were significantly associated with VA failure. PC (HR, 1.003; 95% CI, 1.001 to 1.006; p = 0.069) and smoking status (HR, 1.836; 95% CI, 0.903 to 3.380; p = 0.051) were weakly and non-significantly associated. The use of antiplatelet agents was not significantly associated with failure (HR, 1.441; 95% CI, 0.658 to 3.158; p = 0.361). Aspirin resistance (measured in only 109 patients) was weakly associated with VA failure (HR, 2.043; 95% CI, 0.973 to 4.291; p = 0.059). On multivariate analysis, the MPV (HR, 1.794; 95% CI, 1.066 to 3.020; p = 0.028), PC (HR, 1.003; 95% CI, 1.001 to 1.006; p = 0.01), and smoking (HR, 1.894; 95% CI, 1.019 to 3.519; p = 0.043) independently predicted VA failure. When the data were re-analyzed by access type, MVP was not associated with VA failure in the AVG group (HR, 2.245; 95% CI, 0.689 to 7.312; p =0.180). However, this group contained only 22 patients.
DISCUSSION
VA is essential for HD patients. Vascular intimal hyperplasia and thrombosis are the main causes of VA failure, triggered by platelet activation, endothelial cell injury, and vascular smooth muscle cell proliferation [19-21]. Low-dose aspirin did not maintain AVF patency or prevent AVF failure in a previous study [22,23]. Aspirin resistance is a well-known cause of treatment failure in patients with peripheral vascular and cardiovascular disease [24-26]. Li et al. [27] found that aspirin resistance was associated with a 2.4-fold greater risk of major adverse cardiovascular events in patients with coronary heart disease who complied well with aspirin therapy. Kim et al. [28] reported increased aspirin resistance (20%) in Korean ESRD patients on both HD and peritoneal dialysis. Although the relationship between aspirin resistance and VA failure was not examined, the incidence of thrombotic cardiovascular complications was much higher in nine of 12 (75%) aspirin-resistant patients than in 18 of 47 (38%) aspirin-sensitive patients [28]; thus, aspirin resistance may explain failure of AVF patency. In this study, 15.6% of patients exhibited aspirin resistance that was only weakly associated with VA failure. This is the first report to explore this relationship and more work is needed.
The MPV is associated with cardiovascular disease risk. Sansanayudh et al. [29] reported that an increased MPV was an independent risk factor in patients with coronary heart disease. Varol and Ozaydin [30] reported that the MPV was elevated in patients with chronic renal failure. Henning et al. [31] found that the MPV was associated with coronary heart disease in HD patients. We found that the MPV independently predicted VA failure in HD patients (on both low-dose or no aspirin); as aspirin does not affect the MPV, it would have had no impact on this result [32]. We also found that a high PC was associated with VA failure. An earlier epidemiological study reported that a high PC was associated with cardiovascular disease [33]. We found that the high-MPV group had a lower PC than the low-MPV group, reflecting the inverse relationship between MPV and platelet number [34]. Smoking was independently associated with VA failure, as also found in previous studies [35,36].
MPV reduction may prevent VA failure and stenosis. Yazici et al. [37] reported that lifestyle modifications reduced the MPV in pre-hypertensive patients. As the MPV is affected by low-dose aspirin, such treatment does not reduce the MPV, in line with the findings that aspirin did not maintain AVF patency or prevent AVF failure. Lee et al. [38] found that statin/ezetimibe combination therapy reduced the MPV more so than did statin monotherapy alone. A high MVP was associated with diabetes, especially the HbA1c level, and strict blood sugar control reduced the MVP [37-39]. Both the MPV per se and the MPV/platelet ratio were associated with cardiovascular disease [40]. Recently. Shin et al. [41] found that an increase in the MPV/platelet ratio over 3 months was associated with VA failure in HD patients. As the MPV and platelet numbers are inversely related, a higher MPV/platelet ratio should independently predict VA failure. Indeed, the MPV/platelet ratio was higher in the high than the low MPV group of the present study. However, the ratio did not affect the AVF patency rate in either univariate or multivariate analysis; other factors may be involved. In the cited work, the MPV and platelet were not inversely related and neither independently predicted VA failure. Further study is needed.
Our study had several limitations. First, we measured the MPV and platelet only once, before any VA event. Longitudinal variations in these parameters may affect VA failure. Second, this was a single-center study. Third, we collected blood into ethylenediaminetetraacetic acid (EDTA) tubes, perhaps associated with platelet swelling. However, all analyses were performed within 30 minutes of sampling to minimize laboratory errors.
In conclusion, we found that an increase in the MPV independently predicted VA failure in HD patients. Aspirin resistance was only weakly associated with VA failure. MPV reduction might help prevent VA failure; further study is needed to validate this.
KEY MESSAGE
1. High mean platelet volume (MPV) was an independent risk factor for vascular access failure in hemodialysis patients.
2. Aspirin resistance showed a weak relationship with vascular access failure
3. High MVP is regarded as a potential marker for prediction of vascular access survival in hemodialysis patients.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This work was supported by a grant from Hallym University Medical Center Research fund (01-2009-12).