Hematologic malignancy detected on sacroiliac magnetic resonance imaging in a patient with inflammatory back pain
Article information
A 33-year-old male presented with back pain and fever persisting for 3–4 weeks. Initial evaluation showed normal white blood cell, hemoglobin, and platelet levels, but elevated erythrocyte sedimentation rate (34 mm/h), C-reactive protein (2.48 mg/dL), lactate dehydrogenase (370 IU/mL), and ferritin (719 ng/mL). Infection was not found in the serial diagnostic investigations, including influenza/COVID-19 test, blood/urine culture, interferon-γ releasing assay, and computed tomography.
The patient reported worsening low back and pelvic pain over 3 weeks, unalleviated by rest and relieved by walking, particularly intensifying at night. Back pain hindered the Schober test, but sacroiliac tenderness was noted. Based on previous research indicating axial spondyloarthritis with unexplained fever [1], features of inflammatory back pain prompted diagnostic evaluation for axial spondyloarthritis. With a negative result for human leukocyte antigen (HLA)-B27 and absence of sacroiliitis on X-ray, magnetic resonance imaging (MRI) of the sacroiliac joint was conducted, revealing a myriad of small foci exhibiting low signal on T1-weighted images (Fig. 1A) and high signal on T2-weighted images (Fig. 1B), with nodular enhancement by gadolinium contrast (Fig. 1C). An 18F-fluorodeoxyglucose positron emission tomography scan also demonstrated hypermetabolic activity in the bone marrow of axial skeleton (Fig. 1D). Despite a normal peripheral blood smear, a bone marrow biopsy was performed, ultimately confirming B-lymphoblastic leukemia (Fig. 2).
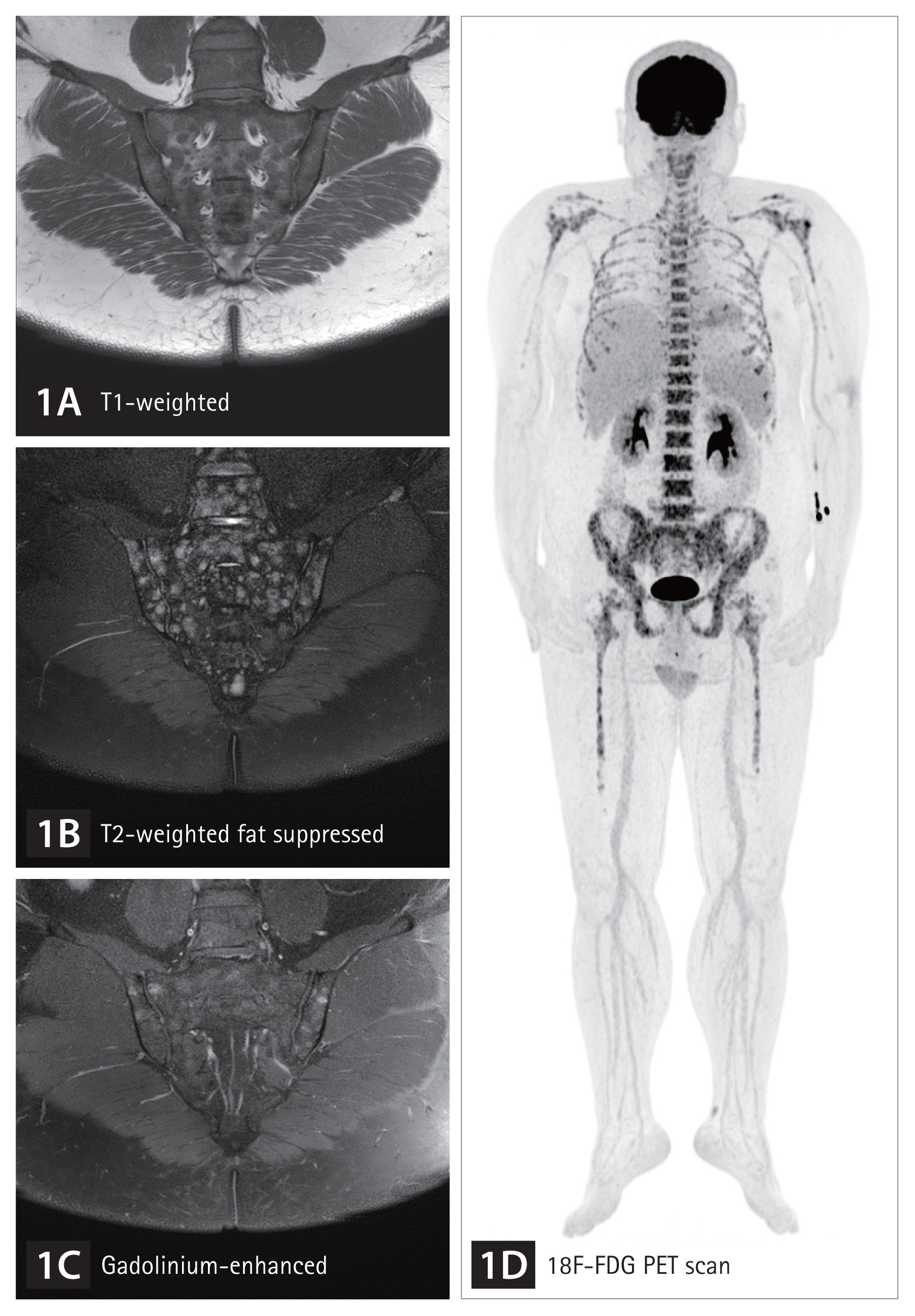
Sacroiliac magnetic resonance imaging (MRI) and 18F-fluorodeoxyglucose positron emission tomography (PET) scan were conducted to assess inflammatory back pain in a 33-year-old male with unexplained fever. Unlike sacroiliitis, which is characterized by bone marrow edema in the subchondral bone, the MRI showed numerous small foci with a low T1-weighted signal (A) and high T2-weighted signal (B), along with nodular enhancement by gadolinium contrast (C). The PET scan also revealed hypermetabolic activity in the bone marrow of axial skeleton (D).
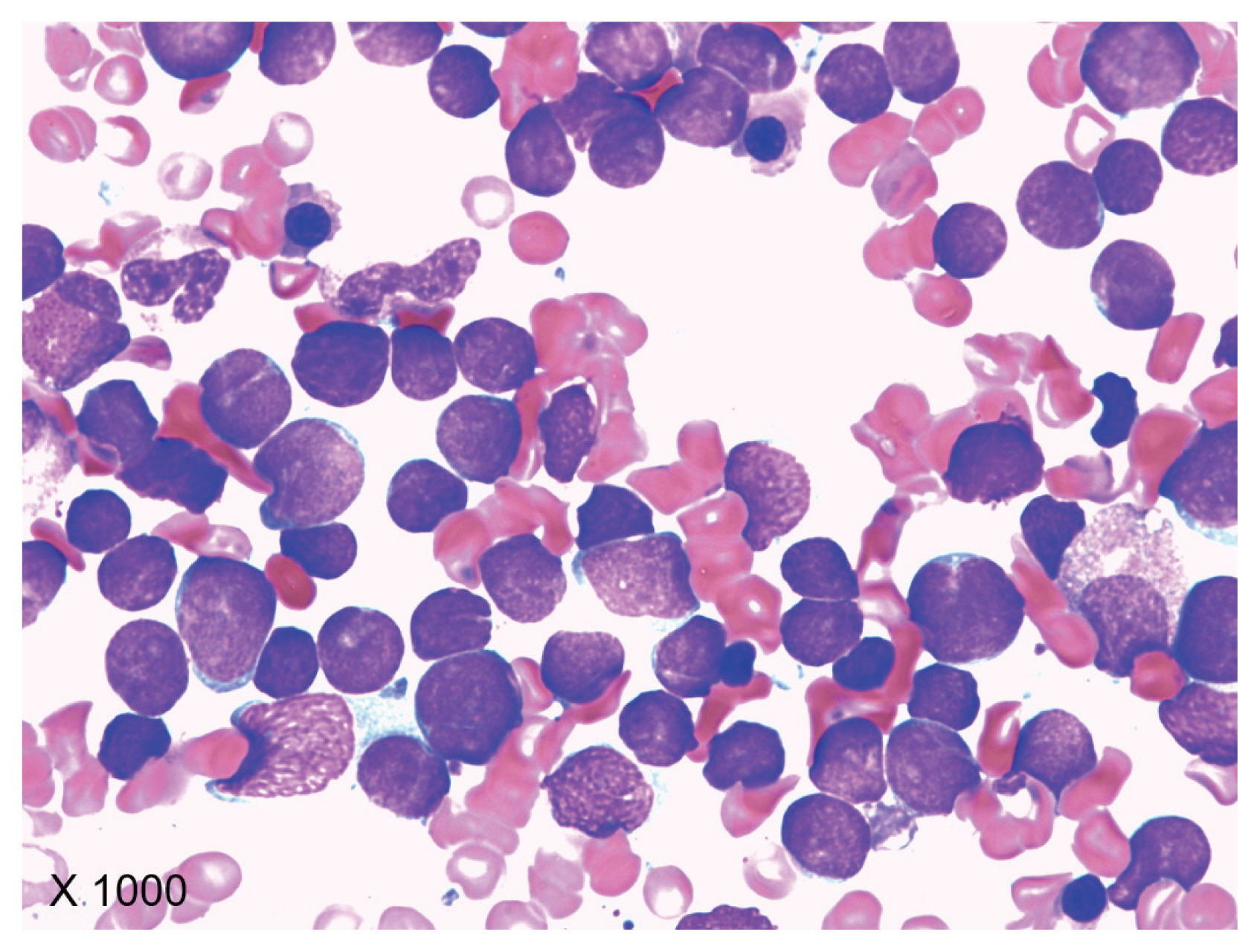
Based on the hypercellular bone marrow finding on sacroiliac magnetic resonance imaging (MRI), the patient underwent a bone marrow biopsy, despite having a normal peripheral blood smear. Wright-Giemsa staining of the bone marrow aspirate revealed leukemic lymphoblasts (× 1,000), confirming the diagnosis of B-lymphoblastic leukemia.
In contrast to inflammatory sacroiliitis, characterized by bone marrow edema typically involving the subchondral bone, hematopoietic malignancies demonstrate red marrow reconversion variably affecting the hematopoietic bone marrow, mainly within the axial skeleton in adults [2]. While bone pain is common in pediatric acute leukemia, musculoskeletal manifestations in adults with acute leukemia are rare [3]. Since peripheral blood tests typically reveal abnormalities in acute leukemia, detection via musculoskeletal MRI is uncommon.
This case highlights the challenges in diagnosing febrile adults with inflammatory back pain, especially in the absence of HLA-B27 and radiographic sacroiliitis.
Notes
CRedit authorship contributions
Jiwon Yang: resources, investigation, writing - original draft, writing - review & editing, visualization; Hyoo Jeong Lim: investigation, writing - review & editing; Seul Ki Lee: resources, investigation, writing - review & editing, visualization; Seung Min Jung: conceptualization, resources, investigation, writing - original draft, writing - review & editing, visualization, supervision, project administration
Conflicts of interest
The authors disclose no conflicts.
Funding
None
