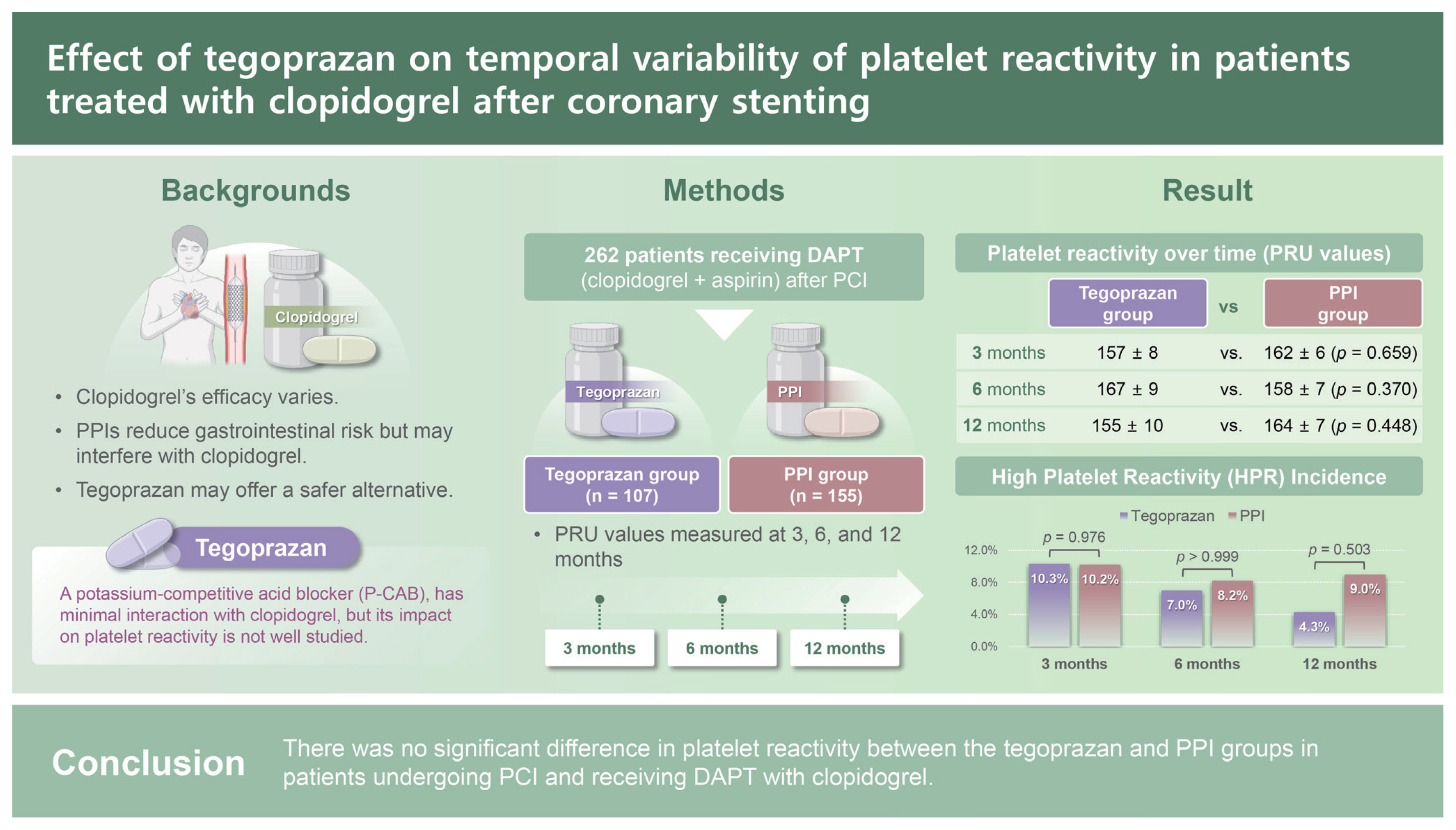
Effect of tegoprazan on temporal variability of platelet reactivity in patients treated with clopidogrel after coronary stenting
Article information
Abstract
Background/Aims
Data on the interactions between clopidogrel and tegoprazan are limited. We compared the effects of tegoprazan and proton-pump inhibitors (PPIs) on platelet reactivity.
Methods
Using database data from March 2020 to January 2023, we retrospectively evaluated 262 patients who were taking either tegoprazan (n = 107) or PPIs (n = 155) combined with dual antiplatelet therapy, including aspirin and clopidogrel, after percutaneous coronary intervention. Platelet reactivity was assessed using VerifyNow P2Y12 assays.
Results
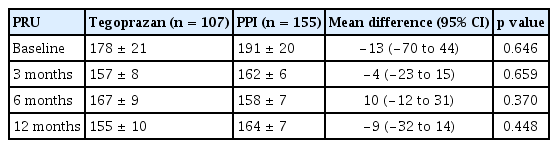
Platelet reaction unit (PRU) values at 3 (157 ± 8 vs. 162 ± 6, p = 0.659), 6 (167 ± 9 vs. 158 ± 7, p = 0.370), and 12 months (155 ± 10 vs. 164 ± 7, p = 0.448) were similar between groups. The prevalence of high on-treatment platelet reactivity, defined as ≥ 253 PRU, was also similar between the groups at 3 (10.3% vs. 10.2%, p = 0.976), 6 (7.0% vs. 8.2%, p = 1.000), and 12 months (4.3% vs. 9.0%, p = 0.503).
Conclusions
There was no significant difference in platelet reactivity between the tegoprazan and PPI groups in patients undergoing PCI and receiving dual antiplatelet therapy with clopidogrel.
INTRODUCTION
Dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 receptor inhibitor is essential for preventing further cardiovascular events in patients undergoing percutaneous coronary intervention (PCI) [1]. Clopidogrel has shown modest antiplatelet effects with significant interpatient variability in levels of on-treatment platelet reactivity [2]. In addition, genetic polymorphisms have been identified that contribute to the observed variability in the clopidogrel response [3]. Subsequent studies have shown that patients with impaired clopidogrel-induced platelet inhibition are at increased risk for ischemic events, in particular, stent thrombosis [4–6].
Current guidelines recommend that patients at a high risk of bleeding should receive proton-pump inhibitors (PPIs) in combination with DAPT to reduce bleeding events [9–11]. However, PPIs have limited use owing to safety issues related to drug–drug interactions with P2Y12 inhibitors, as well as a slow onset of action, short half-life, and patient discomfort when taking medication before meals. Potassium-competitive acid blockers (P-CABs) have emerged as a new class of acid-suppressing drugs. The efficacy of tegoprazan, a new P-CAB, for treating upper gastrointestinal (GI) diseases, including erosive gastroesophageal reflux disease and gastric ulcers, has been demonstrated to be non-inferior to that of PPIs [12,13]. Furthermore, P-CABs are mainly metabolized by CYP3A4, exhibit reduced drug–drug interactions with P2Y12 inhibitors, and are less susceptible to the effects of known genetic polymorphisms than are PPIs [14]. However, the relationship between tegoprazan and antiplatelet agents has not yet been fully investigated.
Therefore, the objective of this study was to determine whether tegoprazan affects platelet reactivity to clopidogrel.
METHODS
Study population and data collection
From March 2020 to January 2023, 1,466 consecutive patients who underwent PCI with drug-eluting stent (DES) implantation at a single center were screened in this retrospective study. We excluded patients who did not receive tegoprazan (HK inno.N Corp., Gyeonggi-do, Korea) or PPIs, those with an absent platelet reaction unit (PRU) value and those treated with potent P2Y12 inhibitors, such as prasugrel or ticagrelor. A total of 262 patients with PRU values after PCI were included in the final analysis and were classified as those who received tegoprazan (n = 107) or PPIs (n = 155) with DAPT after PCI (Fig. 1). Clinical information and laboratory findings were obtained at baseline and at 3 months ± 4 weeks, 6 months ± 4 weeks, and 12 months ± 4 weeks of follow-up.

Study flowchart. PCI, percutaneous coronary intervention; PPI, proton-pump inhibitor; DAPT, dual antiplatelet therapy; PRU, platelet reaction unit.
We used an integrated clinical data server analysis system that incorporated data from our university’s health system, the Severance Clinical Research Analysis Portal, to enroll potential participants and collect anonymized clinical data.
The study protocol was approved by the Institutional Review Board of the Yongin Severance Hospital (approval number: 9-2023-0029), which waived the requirement for informed consent because of the retrospective nature of the study.
Procedures
All patients were administered a loading dose of aspirin (300 mg), 300–600 mg of clopidogrel, and 5,000 units of unfractionated heparin prior to the PCI procedure, unless they had already been taking these medications. The choice of the appropriate medication was at the discretion of the attending physician. Coronary angiography and PCI were performed in accordance with the established standard techniques and current guidelines [15,16]. Additional unfractionated heparin (50–70 IU/kg) was administered during the procedure to maintain the activated clotting time between 250 and 300 seconds. The detailed treatment strategies, including balloon angioplasty or stenting, use of intravascular modalities, use of glycoprotein IIb/IIIa inhibitors, and use of additional devices, including microcatheters and guide extension catheters, were determined at the operator’s discretion.
Measurement of platelet reactivity and study endpoints
Platelet function tests for measuring platelet reactivity were conducted after an adequate period to ensure a full antiplatelet effect using the VerifyNow assay (Instrumentation Laboratory, Bedford, MA, USA). Baseline platelet function testing was performed prior to the administration of antiplatelet agents. Blood sampling was performed within 8 hours of administration of the last dose [17]. The PRU values measured at 3 ± 1 months, 6 ± 1 months, and 12 ± 1 months post-PCI were defined as those measured at 3, 6, and 12 months, respectively, for the analysis.
The primary endpoint was the PRU value at 3, 6, and 12 months after PCI in the tegoprazan and PPI groups. The secondary endpoint was the rate of high platelet reactivity (HPR) in both groups after PCI. HPR was defined by ≥ 253 PRU, according to previous investigations [18,19]. In addition, we evaluated the clinical outcomes, including death, myocardial infarction (MI), revascularization, stent thrombosis, stroke, or GI bleeding. Detailed definition for the clinical outcomes were described in Supplementary Table 1.
Statistical analysis
Data are reported as mean ± standard deviation for continuous variables and as frequency (percentage) for categorical variables. We compared the two groups using an independent-samples t-test for continuous variables and the chi-square test or Fisher exact test for categorical variables. The primary outcomes were analyzed using a linear mixed model with repeated measures, with the treatment group, time points, and interaction between the treatment group and time points as fixed effects, and patients as a random effect. Clinical outcomes between the treatment groups were compared using hazard ratio estimates and 95% confidence intervals were obtained from a Cox proportional hazard model. Inverse probability of treatment weighting (IPTW) was used to adjust for confounding factors. The propensity score was estimated using a multiple logistic regression analysis with all covariates. Twi-sided statistical tests were performed, with p values below 0.05 indicating statistical significance. All statistical analyses were performed using SAS software (version 9.4; SAS Institute, Inc., Cary, NC, USA).
RESULTS
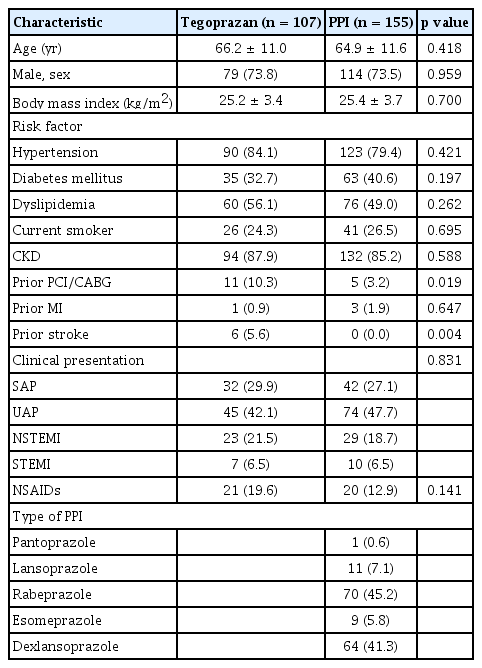
Baseline characteristics
The baseline characteristics of patients in the tegoprazan and PPI groups are shown in Table 1. The average age of the patients overall was 65.4 ± 11.4 years, and males accounted for 73.7% of the total cohort. The tegoprazan group had a higher frequency of prior PCI/CABG and prior stroke; however, the demographics, other risk factors, and clinical presentation were similar between the two groups. Baseline platelet reactivity was similar between two groups (tegoprazan vs. PPI, 178 ± 21 vs. 191 ± 20, p = 0.646). The distribution of propensity scores before and after weighting is presented in Supplementrary Fig. 1.
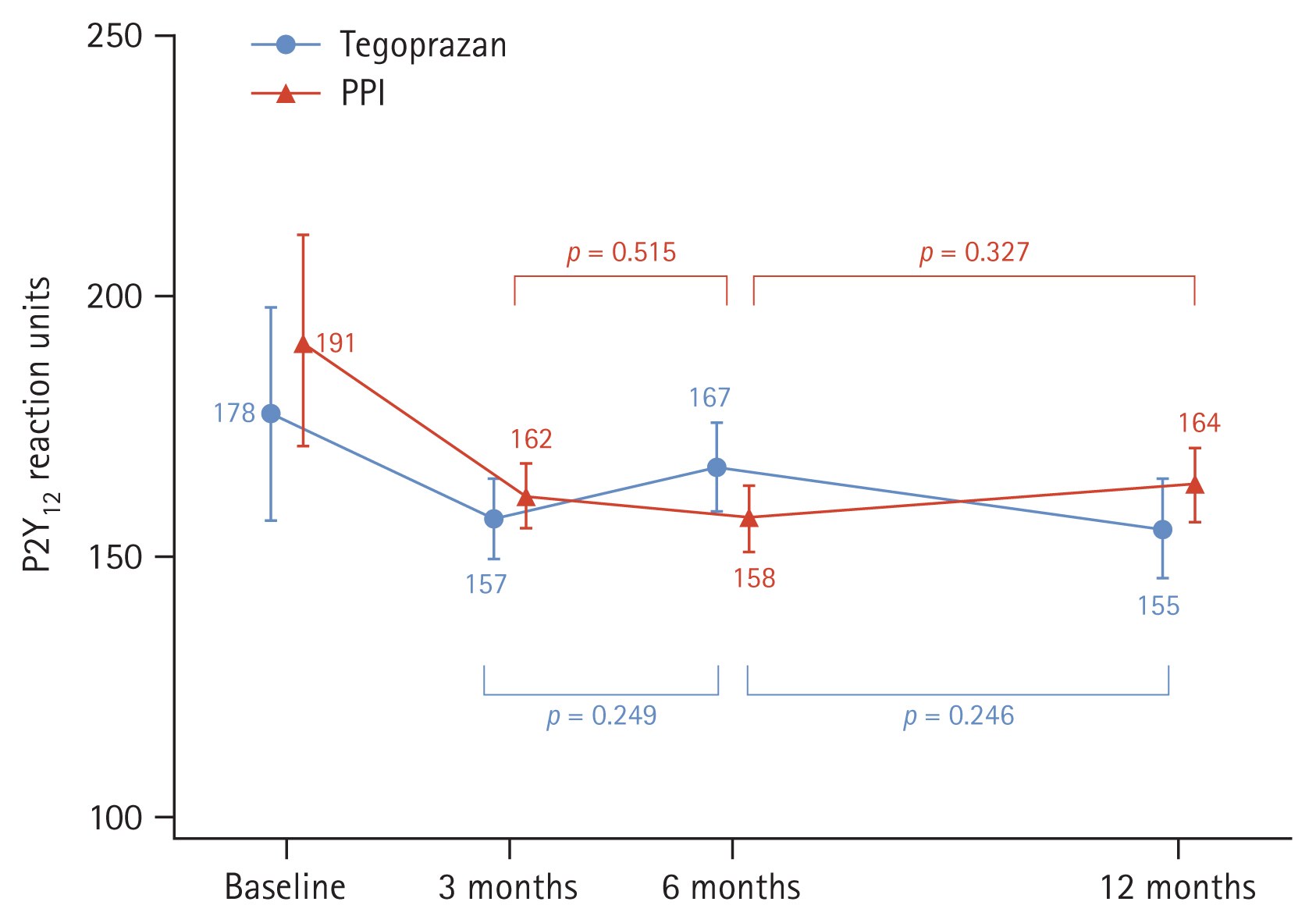
Platelet reactivity
Platelet reactivity at 3 months was not significantly different between the tegoprazan and the PPI group (157 ± 8 vs. 162 ± 6, p = 0.659) (Fig. 2). Platelet reactivity at 6 months and 12 months were also comparable between two groups (6 months, 167 ± 9 vs. 158 ± 7, p = 0.370; 12 months, 155 ± 10 vs. 164 ± 7, p = 0.448). There was no significant change in platelet reactivity over time in the tegoprazan group (3–6 months, p = 0.249; 6–12 months, p = 0.246). Similarly, no significant change in platelet reactivity was observed in the PPI group (3–6 months, p = 0.515; 6–12 months, p = 0.327) (Supplementary Table 2).
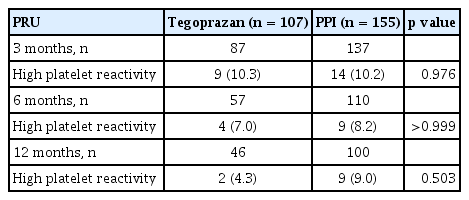
Responder status over time
We investigated the proportion of patients with HPR, defined as a value ≥ 253 PRU, in both tegoprazan and PPI groups. The incidence of HPR was comparable between patients treated with tegoprazan and those treated with PPI (Fig. 3). The incidences of HPR at 3, 6, and 12 months were similar between the two groups (tegoprazan vs. PPI: 3 months, 10.3% vs. 10.2%, p = 0.976; 6 months, 7.0% vs. 8.2%, p > 0.999; 12 months, 4.3% vs. 9.0%, p = 0.503) (Table 3).

Prevalence of high platelet reactivity (PRU ≥ 253). PPI, proton-pump inhibitor; PRU, platelet reaction unit.
Clinical outcomes
During the follow-up period (median, 344 days), 8 cases of major adverse cardiac events (two all-cause deaths, four revascularization of any type and one stroke) and one bleeding events (one GI bleeding and one major bleeding) after PCI with DES implantation. No significant difference was found between the tegoprazan and PPI groups in both crude analyses (Supplementary Table 3). One major bleeding episode in the PPI group involved melena caused by a rectal ulcer at 6 months after PCI in a patient with a history of hemodialysis-dependent end-stage renal disease. The rates of all-cause death, revascularization, target-vessel revascularization were also not significantly different between the two groups in the crude and IPTW analyses. Liver enzyme levels were comparable between the two groups at baseline and after tegoprazan and PPI treatment (Supplementary Table 4).
DISCUSSION
The main findings of the present study were the following. First, platelet reactivity at 3, 6, and 12 months following PCI was comparable between the tegoprazan and PPI groups. Second, the incidence of HPR at 3, 6, and 12 months was comparable between the two groups. To the best of our knowledge, this is the first clinical study evaluating the platelet reactivity to clopidogrel after PCI in relation to the use of tegoprazan compared to PPIs.
These findings highlight a critical issue in the management of patients undergoing PCI who require DAPT. The risk of upper GI bleeding is over three times higher in patients taking DAPT than in non-users [20]. Concurrent administration of gastroprotective therapy is often beneficial, particularly for patients at a high risk of GI bleeding, as this can mitigate the bleeding risk [9–11]. However, traditional PPIs inhibit the CYP2C19 enzyme, which is essential for the activation of clopidogrel. This interaction potentially compromises the antiplatelet efficacy of clopidogrel, increasing the risk of thrombotic events, as highlighted by previous research on PPI and clopidogrel interactions [21]. In contrast, tegoprazan, a P-CAB, which is metabolized independently of CYP2C19, is expected to reduce this interaction risk, thereby potentially enhancing patient safety.
The results of the current study in patients on clopidogrel-based DAPT showed no significant difference in PRU values in the tegoprazan group compared to the PPI group, which mainly used agents with less effects on CYP2C19 metabolism, such as pantoprazole, lansoprazole, dexlansoprazole, and rabeprazole. These results support previous pharmacokinetic and pharmacodynamic study showing that tegoprazan had minimal interaction with cytochrome P450 enzymes and suggest that tegoprazan might be used in patients requiring GI protection without compromising antiplatelet efficacy [14].
Previous research reported that HPR ≥ 253 was significantly associated with the occurrence of major adverse cardiac and cerebrovascular events (MACCE) and net adverse clinical events, including MACCE and bleeding at 5 years after PCI [18]. In our study, tegoprazan showed a comparable incidence of HPR to that among patients treated with PPI, and the incidence of HPR over time were also similar between the two groups.
Notably, these findings may hold particular importance for populations with a high prevalence of CYP2C19 genetic polymorphisms, such as Asian patients [22]. Genetic variations in CYP2C19 can lead to reduced clopidogrel metabolism, further increasing the likelihood of adverse drug–drug interactions with traditional PPIs [23]. Therefore, our results suggest that tegoprazan could be a viable alternative for these patients, offering consistent antiplatelet efficacy without the risks associated with CYP2C19 inhibition.
Another key advantage of tegoprazan is its pharmacological properties as a P-CAB. P-CABs act through competitive potassium inhibition, achieving rapid acid suppression with a sustained effect [24]. This mechanism of action allows for effective gastric pH control and reduces variability in acid suppression, which is critical in preventing GI bleeding in patients on DAPT. Therefore, the rapid onset and durable acid suppression offered by tegoprazan could be particularly beneficial to ensure effective gastroprotection in high-risk patients and may also prevent the interruption of antiplatelet agents due to GI symptoms, including acid reflux, that may arise during treatment.
This study had some limitations. This study was a retrospective analysis with a relatively small study population derived from a single center. Therefore, caution should be exercised when interpreting the findings of this study. Second, neither medication adherence nor tolerability was evaluated. In addition, potential interactions with food or other medications were not considered. Therefore, large-scale randomized studies are warranted to validate our findings and address these limitations. Third, baseline PRU data were available for only a subset of the study population, which may introduce a potential selection bias. To mitigate this limitation, a linear mixed model with repeated measures was employed, allowing for adjustment of missing data. Nevertheless, results pertaining to baseline PRU should be interpreted with caution, considering this limitation. Fourth, the small sample sizes within each PPI subgroup precluded a detailed analysis of platelet reactivity for individual PPIs compared to tegoprazan. Fifth, genetic polymorphisms, which are known to significantly influence antiplatelet function, were not investigated in this study. Future studies should incorporate genetic data to provide a more comprehensive understanding of the observed outcomes.
In conclusion, the current study showed that there was no significant difference in platelet reactivity between the tegoprazan and PPI groups in patients undergoing PCI and receiving DAPT, suggesting that tegoprazan could be considered as a safe and alternative gastroprotective agent in these patients. Future large-scale, long-term studies are warranted to validate these findings.
KEY MESSAGE
1. We demonstrated that clopidogrel reactivity over time after PCI were similar between the tegoprazan and the PPI groups.
2. The incidence of high on-treatment platelet reactivity over time was also comparable between the tegoprazan and the PPI groups.
Notes
CRedit authorship contributions
Oh-Hyun Lee: conceptualization, methodology, investigation, data curation, formal analysis, writing - original draft, visualization; Ji Woong Roh: validation, software, writing - review & editing; Yongcheol Kim: conceptualization, methodology, investigation, writing - review & editing, visualization, supervision, project administration; Eui Im: validation, writing - review & editing, supervision; Deok-Kyu Cho: validation, writing - review & editing, supervision
Conflicts of interest
The authors disclose no conflicts.
Funding
None