Herpes zoster infection in patients with inflammatory bowel disease
Article information
Abstract
Patients with inflammatory bowel disease (IBD) are at increased risk of herpes zoster (HZ), particularly those receiving immunosuppressive treatments such as corticosteroids, thiopurines, and biologics, which elevate the likelihood of varicella-zoster virus reactivation. Despite this, vaccination rates among patients with IBD remain low. Shingrix, a recombinant zoster vaccine, is generally preferred because of its high efficacy (> 90%) and safety profile in immunocompromised individuals, unlike the live attenuated zoster vaccine (Zostavax). This review underscores the importance of HZ vaccination for patients aged ≥ 50 years, as well as for younger patients receiving high-risk therapies such as JAK inhibitors. Tailored vaccination strategies based on individual risk factors, including disease severity, medication use, and ethnicity, may enhance prevention. Given the higher incidence of HZ in certain populations, such as those in Korea, vaccination recommendations should be adapted accordingly. Further research is needed to evaluate the long-term effectiveness of Shingrix in younger patients with IBD to ensure sustained protection and prevent complications, such as postherpetic neuralgia.
INTRODUCTION
Inflammatory bowel disease (IBD), comprising Crohn’s disease (CD) and ulcerative colitis (UC), is a chronic inflammatory condition affecting the gastrointestinal tract. Its pathogenesis involves genetic predisposition, environmental factors, and immune dysregulation [1].
Herpes zoster (HZ), also termed shingles, results from reactivation of the latent varicella-zoster virus (VZV). It typically presents as a painful vesicular rash in a dermatomal distribution. The most common complication of HZ is postherpetic neuralgia, which manifests as chronic neuropathic pain and significantly impairs daily activities [2].
The incidence of HZ increases with age and is higher in individuals with predisposing conditions [3,4]. Patients with IBD, particularly those with high disease activity or using certain medications, have a higher prevalence of HZ than the general population [5,6]. The occurrence of HZ significantly reduces quality of life and causes substantial distress [7]. Vaccines developed to prevent HZ provide preemptive protection, reducing its incidence [8].
There are two types of HZ vaccines. Conventional live attenuated vaccines must be administered either 1 month before or 3 months after the cessation of immunosuppressive IBD medications and are recommended only for individuals aged ≥ 50 years [9]. A recombinant adjuvant zoster vaccine (RZV) has been developed to overcome these limitations, allowing vaccination regardless of ongoing IBD medication use [10].
This review examines the epidemiology of HZ in patients with IBD, the associated risk factors, and the role of vaccination in reducing HZ risk. We also discuss current evidence on the use of HZ vaccines, particularly RZV, in immunocompromised individuals and provide updated vaccination recommendations for patients with IBD, considering age, immunosuppressive therapies, and other risk factors.
EPIDEMIOLOGY AND RISK FACTORS
The incidence of HZ among adults in the general population is 2.4 to 10.6 cases per 1,000 person-years [11–14]. Analyses using South Korea’s Health Insurance Review and Assessment database revealed that the incidence of HZ in the general population of South Korea is relatively high compared with other countries, ranging from 7.9 to 18.5 cases per 1,000 person-years [15–17].
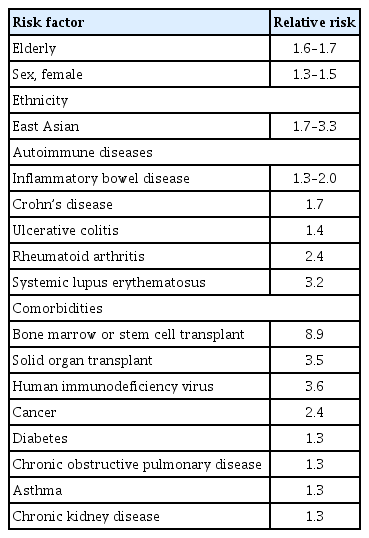
The incidence of HZ is 1.3 to 3.2 times higher in patients with autoimmune diseases, such as rheumatoid arthritis, systemic lupus erythematosus, IBD, psoriasis, psoriatic arthritis, ankylosing spondylitis, and multiple sclerosis, than in the general population [13,14,18]. Furthermore, the incidence of HZ is higher in patients who have undergone bone marrow, stem cell, or solid organ transplantation, as well as in individuals with human immunodeficiency virus infection or solid tumors, than in the general population [13]. Additionally, people with underlying conditions such as diabetes, chronic obstructive pulmonary disease, asthma, and chronic kidney disease have an approximately 1.3-fold higher incidence of HZ than people without these conditions [18].
The incidence of HZ is approximately 1.3 to 2.0 times higher in patients with IBD than in healthy individuals [13,14,19,20]. A meta-analysis revealed that the incidence of HZ increased by approximately 1.7 times in patients with CD and 1.4 times in patients with UC [21]. An analysis of United States insurance claims data found that the incidence of HZ in individuals with IBD was 1.7 times higher than in those without IBD. The incidence was 7.3 cases per 1,000 person-years for IBD overall, 8.1 cases per 1,000 person-years for CD, and 6.7 cases per 1,000 person-years for UC, showing a higher incidence in patients with CD than in those with UC [19]. A study of data obtained from the South Korean Health Insurance Review and Assessment Service showed that the incidence of HZ in individuals with IBD was 18.3 cases per 1,000 person-years, which was 1.5 times higher than that in healthy individuals. HZ showed a stronger association with CD than UC, with a 1.9-times higher incidence in patients with CD and a 1.4-times higher incidence in those with UC compared with the general population [20].
One major risk factor for developing HZ is age [3,14,22]. A meta-analysis revealed that increasing age raises the relative risk of HZ by 1.7 times [3]. Studies conducted in various countries have shown that the incidence of HZ tends to increase with age [22]. Research in Korea showed that the incidence of HZ gradually increases starting in people’s 20s, rises rapidly from ages 45 to 49 years, and peaks in their 70s [17]. Among patients with IBD, the incidence of HZ is higher in those aged ≥ 50 years than in those aged 20 to 49 years [19,23]. A study of Korean patients with IBD showed similar results, with the incidence of HZ gradually increasing with age in both patients with CD and those with UC, doubling in individuals aged > 50 years compared with those aged 20 to 49 years [20].
However, younger patients with IBD have a higher incidence of HZ than healthy controls, while the difference in the incidence of HZ between patients with IBD and healthy controls decreases in older age groups. Yun et al. [14] found that patients with IBD in their 20s had a 4.3-times higher incidence of HZ than healthy controls, and this decreased to 2.2 times in those aged > 70 years. A Canadian study showed that patients with IBD aged 18 to 29 years had a 3.0-times higher incidence of HZ than healthy controls, while those aged > 60 years had a 0.4-times lower incidence [23]. Studies of Korean individuals demonstrated that patients with IBD in their 20s had an approximately 1.8-fold higher incidence of HZ than healthy controls, and this decreased to approximately 1.3-fold in individuals aged ≥ 70 years [20,24].
Female sex is also a risk factor for HZ. In a meta-analysis by Kawai and Yawn [18], women had an approximately 1.3-times higher incidence of HZ than men. Similarly, a meta-analysis by Marra et al. [3] showed that women had a 1.2-times higher incidence of HZ than men. A study of Korean individuals showed that women had an HZ incidence of approximately 12.6 cases per 1,000 person-years, compared with 8.3 cases per 1,000 person-years in men [15]. Furthermore, a study of patients with IBD also showed a higher incidence of HZ in women. In the above-mentioned Korean study, men had an incidence of 16.1 cases per 1,000 person-years, while women had an incidence of 21.8 cases per 1,000 person-years (Table 1) [20].
MEDICATION-RELATED RISKS
IBD alternates between periods of exacerbation and remission, and the severity of inflammation and affected areas vary among individuals. Several different medications, including 5-aminosalicylic acid (5-ASA), steroids, immunomodulators, biologics, and small molecules, are used depending on the patient’s condition [25,26]. 5-ASA, steroids, and immunomodulators are categorized as conventional therapy, while biologics and small molecules are classified as advanced therapy.
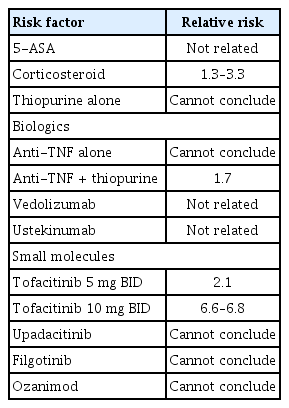
Two cohort studies revealed that 5-ASA does not increase the incidence of HZ in patients with IBD [5,19]. The results showed no increase in incidence in patients with CD or in those with UC. This finding was consistent when analyzed separately for new and persistent users, as well as for current and previous users. By contrast, corticosteroid use increased the incidence of HZ by approximately 1.3 to 3.3 times, while thiopurine use in patients with IBD increased the incidence of HZ by 1.0 to 4.2 times [5,12,19,27]. A nationwide study of Korean patients with IBD showed that corticosteroid use increased the incidence of HZ by approximately 2.4 times in patients with UC and 2.7 times in those with CD. By contrast, thiopurine use was not associated with an increased incidence of HZ in patients with either condition [20].
A large cohort study in the United States showed that anti-tumor necrosis factor (anti-TNF) agents increased the incidence of HZ by approximately 1.8 times. Similarly, nationwide data from Korea indicated that anti-TNF agents increased the incidence of HZ by approximately 2.1 times in patients with UC, but not in those with CD [19,20]. Data from the US National Veterans Affairs Healthcare System (VAHS) showed that although anti-TNF agents alone did not increase the incidence of HZ, they increased the incidence by approximately 1.7 times when combined with thiopurine [12]. Data on adalimumab are less extensive than on other anti-TNF agents; however, an analysis of 6 clinical trials involving 3,160 patients with CD showed that 46 patients (1.5%) developed HZ [28]. In the VARSITY trial, which compared adalimumab and vedolizumab in patients with UC, the incidence rate was higher in the adalimumab group (42 cases per 1,000 person-years) than in the vedolizumab group (5 cases per 1,000 person-years) [29]. Among patients using anti-TNF agents, the incidence of severe forms of HZ did not significantly increase, although HZ may still occur in such patients [30].
A large-scale analysis combining six clinical studies compared vedolizumab with placebo in patients with IBD, revealing no significant difference in the incidence of HZ (9 cases per 1,000 person-years in the placebo group and 7 cases per 1,000 person-years in the vedolizumab group) [31]. In another cohort study, no cases of HZ were reported among 167 patients with IBD treated with vedolizumab [12].
In major randomized controlled trials, including studies involving patients with moderate to severe CD and UC, ustekinumab was not associated with an increased risk of HZ. Specifically, these trials, which included patients with refractory CD and UC, revealed no significant cases of HZ among participants treated with ustekinumab. This consistent finding across different IBD populations suggests that ustekinumab does not substantially elevate the risk of developing HZ and is relatively safe in terms of HZ occurrence, even in patients at higher risk due to their underlying conditions and immunosuppressive treatments [32–34].
Tofacitinib, a non-selective Janus kinase inhibitor, is the first small molecule available for the treatment of UC [26,35]. According to one study, the incidence of HZ was 9.7 cases per 1,000 person-years in the placebo group, compared with 20.1 cases per 1,000 person-years in the group using tofacitinib 5 mg twice daily (BID) and 66.4 cases per 1,000 person-years in the group using tofacitinib 10 mg BID [36]. In a long-term data analysis combining multiple global clinical studies, the incidence of HZ was 2.1 times higher in the group using tofacitinib 5 mg BID and 6.6 times higher in the group using tofacitinib 10 mg BID compared with the placebo group [37]. However, the incidence of severe forms of HZ did not significantly increase compared with the placebo group. In the tofacitinib group, risk factors for the occurrence of HZ included age (hazard ratio [HR], 1.6), prior failure of TNF inhibitor therapy (HR, 1.9), and Asian ethnicity (HR, 1.8) [36].
Upadacitinib, a selective JAK1 inhibitor, is approved for the treatment of both CD and UC. In a phase 3 clinical trial investigating upadacitinib as a treatment for UC, 3 cases of HZ were reported among 663 patients (0.5%) receiving 45 mg/d of upadacitinib during the induction period, with no cases in the control group. During the maintenance period, the incidence of HZ was 50 cases per 1,000 person-years in patients maintained on 15 mg/d and 44 cases per 1,000 person-years in those maintained on 30 mg/d, with no cases reported in the control group [38]. In two phase 3 clinical trials for CD, HZ occurred in 15 of 674 patients (2.2%) in the upadacitinib group during the 12-week induction therapy period at 45 mg/d, while no cases were reported in the control group. During the maintenance period, the incidence of HZ was 40 cases per 1,000 person-years in patients maintained on 15 mg/d, 72 cases per 1,000 person-years in those maintained on 30 mg/d, and 47 cases per 1,000 person-years in the control group [39].
In a phase 2b/3 trial investigating filgotinib for the treatment of UC, HZ occurred in 0.2% of patients receiving 100 mg/d and 0.6% of patients receiving 200 mg/d of filgotinib during the induction period, with no cases reported in the control group. During the maintenance period, no cases of HZ were reported among 179 patients maintained on 100 mg/d. However, 1 case (0.5%) was reported among 202 patients maintained on 200 mg/d, compared with an incidence of 1.1% in the control group [40]. In a phase 2 clinical study of CD, no cases of HZ were reported in patients receiving either 100 or 200 mg/d of filgotinib.
Ozanimod is an oral small molecule that modulates sphingosine 1-phosphate (S1P) receptors, specifically targeting the S1P1 and S1P5 receptor subtypes [41]. In the True North phase 3 study evaluating ozanimod for the treatment of UC, HZ occurred in 3 of 796 patients (0.4%) during the induction period, with no cases in the control group. During the maintenance period, HZ developed in 5 of 230 patients (2.2%) compared with 1 of 227 patients (0.4%) in the control group [42]. Further data collection is needed for a more accurate analysis of the incidence of HZ (Table 2).
VACCINATION FOR HZ PREVENTION
Zostavax (Merck & Co., Inc., Kenilworth, NJ, USA), a live attenuated vaccine (zoster vaccine live, ZVL) was the first vaccine licensed by the United States Food and Drug Administration (FDA) for the prevention of HZ [43]. The vaccine is administered as a single dose via subcutaneous injection. It reduces the incidence of HZ by 51.3% and postherpetic neuralgia by 66.5% in individuals aged ≥ 60 years [44]. However, the efficacy of Zostavax decreases over time, with significant reductions observed beyond the first year and further declines by the fifth to seventh year after vaccination [45]. In patients with IBD, particularly those receiving immunosuppressive therapy, the use of Zostavax presents certain challenges. As a live vaccine, Zostavax is contraindicated in patients who are severely immunocompromised because of the risk of vaccine-induced HZ [46,47]. Despite these limitations, Zostavax has been associated with a reduced incidence of HZ in patients with IBD. A study conducted within the VAHS showed that vaccination with Zostavax reduced the risk of HZ, with an adjusted HR of 0.54 [48]. However, the study also highlighted the underutilization of the vaccine in this population, with only 17.9% of eligible patients with IBD receiving the vaccine during the study period [48].
Shingrix, a non-live RZV approved by the United States FDA in 2017 [49], has become the preferred option for HZ prevention in adults aged ≥ 50 years [50,51]. The vaccine is administered in two intramuscular injections, with the first dose given at baseline and the second dose 2 to 6 months later. Because it is non-live, Shingrix is safer for patients with IBD, particularly those on immunosuppressive therapies; it avoids the risks associated with live vaccines, such as Zostavax [50]. Shingrix uses a VZV glycoprotein E antigen combined with an adjuvant system (AS01B) to elicit a strong immune response, even in immunocompromised individuals [52,53]. Clinical trials have shown that Shingrix demonstrates a 97.2% effectiveness in preventing HZ in adults aged ≥ 50 years (ZOE-50 study) and an 89.8% effectiveness in adults aged ≥ 70 years (ZOE-70 study), alongside a significant reduction in postherpetic neuralgia [50,51]. With vaccination, local injection site reactions (such as pain and redness) and general adverse events (such as fever and headache) have been reported. However, the incidence of serious adverse events was not significantly higher than that in the placebo group [51].
The long-term efficacy and safety of HZ vaccines are critical factors, particularly for patients with IBD who often require chronic immunosuppressive therapy. These patients face an increased risk of HZ because of both their underlying disease and immunosuppressive treatments, making durable and safe vaccine protection essential. Zostavax has demonstrated decreasing efficacy in preventing HZ over time. In one study, its effectiveness was approximately 33% within the first 3 years post-vaccination but declined to approximately 19% after ≥ 4 years [54]. Another study reported a significant drop in efficacy, with effectiveness decreasing from 68.7% in the first year to 4.2% after 8 years [55]. This waning immunity limits the long-term effectiveness of Zostavax, particularly for younger patients with IBD who may receive it before reaching their peak risk for HZ. Additionally, the live nature of Zostavax poses safety concerns for immunosuppressed patients because of the risk of vaccine-induced HZ [48]. Shingrix, a recombinant adjuvanted vaccine, has shown superior long-term efficacy compared with Zostavax. After vaccination with Shingrix, the vaccine maintained an average efficacy of > 90% in preventing HZ over 8 years, with data from the eighth year still demonstrating approximately 84% effectiveness (Table 3) [56].
Shingrix administration resulted in a comparable increase in humoral and cell-mediated immunity in individuals who had received ZVL 5 years earlier and those without prior ZVL vaccination, with both groups showing significant improvements from baseline [57]. Immunity remained sustained at 12 months post-vaccination, with no differences in the safety profile observed between the two groups [58]. Additionally, immune responses persisted for up to 10 years in individuals who had completed the initial two-dose course of Shingrix. Strong anamnestic immune responses were observed following an additional dose administered 10 years after the initial course [59].
In a study involving adults aged ≥ 18 years who underwent autologous stem cell transplantation, Shingrix demonstrated an efficacy of approximately 68.2% in preventing HZ compared with placebo [60]. In patients with hematologic malignancies, Shingrix showed an 87.2% efficacy in preventing HZ compared with placebo [61]. In a study analyzing humoral immunogenicity, cell-mediated immunity, and safety of RZV in individuals aged ≥ 18 years with solid tumors, both humoral and cell-mediated immune responses were sustained 1 year after vaccination without safety concerns [62]. Similarly, in immunosuppressed individuals who had undergone renal transplantation, RZV administration resulted in sustained humoral and cell-mediated immune responses 1 year post-vaccination without safety concerns [63].
RECOMMENDATION FOR PATIENTS WITH IBD
Vaccination is a critical component of care for HZ prevention in patients with IBD, particularly given the increased risk posed by immunosuppressive therapies such as thiopurines, corticosteroids, and anti-TNF agents. Patients with IBD are at a significantly higher risk of developing HZ than is the general population, and this risk is further elevated for those undergoing immunosuppressive treatment. Among newer therapies, JAK inhibitors such as tofacitinib [36] are associated with an increased risk of HZ, while other agents, such as ustekinumab and vedolizumab, do not significantly increase the risk [31,64].
Two HZ vaccines are currently available: the ZVL vaccine (Zostavax) and the RZV (Shingrix). Clinical guidelines strongly recommend vaccination for patients with IBD aged ≥ 50 years because this population is particularly vulnerable to reactivation of the VZV, resulting in HZ [47,65]. Between the two vaccines, Shingrix is preferred because of its superior efficacy, exceeding 90% in preventing HZ and reducing postherpetic neuralgia, as well as its favorable safety profile in immunocompromised individuals [56].
Shingrix can be safely administered to patients receiving biologics, JAK inhibitors such as tofacitinib and upadacitinib, and immunosuppressants such as azathioprine. By contrast, Zostavax is contraindicated in these patients because of the risk of vaccine-related HZ [47]. Zostavax can be considered for patients not receiving immunosuppressive therapy, but its overall efficacy and long-term protection are inferior to those of Shingrix [66].
For patients undergoing immunosuppressive therapy, ZVL vaccines such as Zostavax should be administered at least 4 weeks before initiating immunosuppressive treatment or 3 to 6 months after discontinuing the therapy. By contrast, RZV (Shingrix), as a non-live vaccine, can be safely administered to immunocompromised patients without requiring timing adjustments related to immunosuppressive therapy [65].
In addition to patients aged ≥ 50 years, Shingrix should be considered for younger patients with IBD, particularly those aged 19 to 49 years who are at high risk of developing HZ because of factors such as repeated use of corticosteroids, combination immunosuppressant therapy, a history of HZ, or treatment with JAK inhibitors. Studies have shown that the incidence of HZ in patients with IBD aged 30 to 50 years can be comparable to, or even higher than that of the general population aged ≥ 60 years [19,20]. Therefore, early vaccination in these younger, high-risk patients is crucial for preventing HZ and its associated complications.
Ethnicity can also influence the risk of HZ. Asian populations, including those in Korea, have a higher incidence of HZ than Caucasian populations [11,15]. This elevated risk is particularly pronounced in patients with IBD receiving JAK inhibitors, such as tofacitinib, in whom HZ rates are significantly higher [67]. Therefore, adopting a proactive vaccination strategy tailored to each patient’s risk profile is essential. Taiwan’s IBD guidelines recommend HZ vaccination prior to initiating immunosuppressive therapy or for immunocompetent patients aged > 50 years [68]. Additionally, surveys indicate that many IBD physicians in East Asia are proactively administering these vaccines to their patients [69].
For patients who have previously received the ZVL (Zostavax), revaccination with Shingrix is recommended to enhance protection because Shingrix has demonstrated superior efficacy and longer-lasting protection compared with Zostavax [56,57]. Long-term data suggest that immunity from Shingrix persists for many years. Additionally, booster doses have been shown to maintain strong immune responses effectively, even in individuals previously vaccinated with Shingrix [59].
CONCLUSION
This comprehensive review highlights that HZ vaccination is a crucial preventive measure for patients with IBD, particularly those receiving immunosuppressive therapies. The RZV is preferred because of its high efficacy and favorable safety profile in immunocompromised individuals. Vaccination is recommended for patients with IBD aged ≥ 50 years, as well as for younger patients (19–49 years) with risk factors such as corticosteroid use, combination immunosuppressant therapy, or treatment with JAK inhibitors. Early vaccination is critical given the increased risk of HZ in patients with IBD, particularly those on therapies such as tofacitinib. For individuals previously vaccinated with the ZVL, revaccination with Shingrix is advised to ensure long-term protection. Special consideration should also be given to high-risk populations, such as East Asians, who exhibit a higher incidence of HZ. In summary, tailored vaccination strategies are essential for reducing the risk of HZ and ensuring optimal care for patients with IBD.
Notes
CRedit authorship contributions
Dong Hyun Kim: conceptualization, methodology, writing - original draft, writing - review & editing; Sang-Bum Kang: conceptualization, writing - review & editing, supervision
Conflicts of interest
The authors disclose no conflicts.
Funding
None