Role of catheter ablation in patients with heart failure and atrial fibrillation
Article information
Abstract
Atrial fibrillation (AF) and heart failure (HF) frequently coexist with other cardiovascular conditions and adversely affect each other. Over the past few decades, there have been therapeutic advances in AF and HF; however, whether rate-control or rhythm-control is the superior approach for these patients remains controversial. Additionally, there is debate regarding whether antiarrhythmic drug therapy or ablation is the optimal strategy for rhythm-control. The outcomes of AF ablation have improved, and several studies have assessed the potential benefits of AF ablation in patients with HF. The positive impact of catheter ablation in patients with AF and impaired left ventricular (LV) systolic function extends beyond rhythmic outcomes and may result in LV function improvement. This review provides a brief overview of this topic and summarizes several prospective randomized trials that have shown important clinical outcomes comparing AF ablation and non-ablation treatment options in patients with AF and HF so as to provide improved treatment guidance.
PATHOPHYSIOLOGY, EPIDEMIOLOGY AND PROGNOSIS OF ATRIAL FIBRILLATION AND HEART FAILURE
Atrial fibrillation (AF) and heart failure (HF) are common cardiovascular disorders that often coexist, exacerbating each other and leading to significant structural, electrophysiological, and clinical complications [1]. AF and HF share predisposing risk factors such as age, coronary and peripheral artery disease, obesity, smoking, chronic kidney disease, hypertension, sleep apnea, diabetes, and metabolic syndrome [1-3]. The prevalence of AF is rising globally. The 2019 Global Burden of Disease study reported that > 59 million people were living with AF in 2019, and according to projection studies, the number of people with AF is expected to increase to 12.1 million in the United States by 2050 and 17.9 million in Europe by 2060 [4-6]. The prevalence of HF is increasing, with an estimated 64.3 million people affected worldwide in 2017 [7]. In Korea, the incidence of AF has increased 1.5-fold over the past 10 years, reaching 275 cases per 100,000 person-years by 2022. Additionally, the proportion of HF among patients with AF is predicted to be 27.6% in 2022 [8].
AF directly contributes to the development of HF, primarily by causing tachycardia-induced cardiomyopathy [1]. In AF, the loss of effective atrial contractility causes impaired left ventricular filling and elevated left atrial pressure, whereas an increased resting heart rate and irregular ventricular rhythm shorten the diastolic filling time [3,9,10]. AF is associated with worsening of the New York Heart Association (NYHA) functional class, and AF-induced left atrium (LA) dilatation and atrial myopathy cause functional mitral and tricuspid regurgitation [9,11-13]. Similarly, patients with HF can develop AF through various mechanisms. Chronically elevated left atrial pressure, dysregulation of intracellular calcium, and autonomic and neuroendocrine dysfunctions in HF can lead to the creation of an abnormal atrial substrate for AF [9,14-16].
Among patients with HF, the coexistence of AF worsens symptoms, increases hospitalization rates, and increases the risk of poor cardiovascular outcomes [17-19]. Some studies have shown that AF predicts worse outcomes in patients with HF with preserved ejection fraction (HFpEF, left ventricular ejection fraction [LVEF] ≥ 50%) and HF with mid-range ejection fraction (HFmrEF, LVEF 41–49%) [20-22]. Additionally, other studies have demonstrated that AF increases the risk of mortality and HF hospitalization across the entire spectrum of ejection fractions, including HF with reduced ejection fraction (HFrEF, LVEF ≤ 40%) [17,23]. In a retrospective analysis of the Studies of Left Ventricular Dysfunction (SOLVD) trial, AF, compared with sinus rhythm, was associated with a significantly increased risk of all-cause mortality, progressive pump-failure death, and the composite endpoint of death or hospitalization for HF in patients with asymptomatic and symptomatic left ventricular systolic dysfunction (mean LVEF 26–27%) [24]. Furthermore, data from the Effective Anticoagulation with Factor Xa Next Generation in Atrial Fibrillation-Thrombolysis in Myocardial Infarction 48 (ENGAGE-AF 48) trial found that patients with AF and HF, regardless of the HF phenotype involved, are at a higher risk of HF hospitalization and death [23]. The presence of AF has also been found to increase the risk of HF. In a study of 39,710 patients with cardiac implantable electronic devices, the device-based AF burden was associated with an increased risk of new-onset HF and all-cause mortality in patients without pre-existing HF [25]. Among patients with HF, a higher AF burden is associated with more frequent HF hospitalization and increased all-cause mortality [25]. AF can both precede and follow HFrEF and HFpEF, and the combination of AF and HF is associated with poor prognosis, with an especially high risk in patients with HFrEF [26].
RHYTHM-CONTROL VERSUS RATE-CONTROL IN AF WITH HF
The Danish Investigations of Arrhythmia and Mortality on Dofetilide in Congestive Heart Failure (DIAMOND-CHF) trial is a randomized controlled trial comparing pharmacological rhythm-control with dofetilide versus placebo in patients with HFrEF and AF. Treatment with dofetilide significantly reduced hospitalization for worsening HF compared with placebo (hazard ratio [HR], 0.75; 95% confidence interval [CI], 0.63–0.89) and was effective in converting AF to sinus rhythm, but had no effect on mortality (HR, 0.95; 95% CI, 0.81–1.11) [27]. The Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFRIM) trial, a randomized, multicenter trial conducted two decades ago that compared a rhythm-control strategy with cardioversion and antiarrhythmic drugs to a rate-control strategy in patients with AF, found no difference in overall and cardiovascular mortality between the two groups [28,29]. In the Strategies of Treatment of Atrial Fibrillation (STAF) trial, an early study comparing a rhythm control strategy to a rate-control strategy in persistent AF, there was no difference in the primary outcomes of mortality, cardiovascular events, stroke, and systemic embolism between the two groups [30]. In a randomized controlled trial published in 2008 which compared a rhythm control group using amiodarone with a rate-control group in 1,376 patients with LVEF ≤ 35%, symptoms of congestive heart failure, and a history of AF, there was no difference between the two groups in terms of death from cardiovascular causes, stroke, and worsening HF [31]. These earlier studies had several limitations, including high crossover rates, lack of information concerning how underlying comorbidities were treated, HF, and the absence of catheter ablation for AF as a rhythm-control option [32]. Amiodarone remains the preferred agent for rhythm-control in patients with HF. In contrast, dronedrone is contraindicated in patients with symptomatic HF, as it has been associated with an increased risk of mortality due to worsening HF, as shown in the ANDROMEDA trial [33]. Furthermore, Class IC antiarrhythmic drugs are avoided in patients with prior myocardial infarction or left ventricular dysfunction because of their proarrhythmic potential, as seen in the Cardiac Arrhythmia Suppression Trial (CAST) [34].
Substudies of the AFFIRM trial demonstrated that the presence of current AF was associated with a worse NYHA functional class [35]. Patients in the rhythm-control group experienced fewer HF symptoms than those in the rate-control group, and stable sinus rhythm was associated with the best functional status [36]. A recent study, a prespecified sub-analysis, included patients with signs or symptoms of HF at enrollment into the Early Treatment of Atrial Fibrillation for Stroke Prevention Trial (EAST-AFNET4) [37] and compared an early rhythm-control (ERC) strategy consisting of antiarrhythmic drug therapy or catheter ablation to maintain sinus rhythm with usual care (rate-control was the initial strategy and rhythm-control was allowed to improve symptoms) over a median follow-up period of 5.1 years. This sub-analysis of the EAST-AFNET4 focused on 798 patients with stable HF, the majority of whom had HFpEF (56.3%), whereas the others had HFmrEF (26.9%) or HFrEF (16.8%). The results demonstrated that ERC therapy reduced the composite outcome of cardiovascular death, stroke, or hospitalization for worsening of HF or for acute coronary syndrome compared with usual care (univariable HR, 0.74; 95% CI, 0.56–0.97; p = 0.03). A statistically significant difference was observed in terms of cardiovascular mortality. There was no significant interaction between treatment effects and the presence of HF compared to that in patients with normal LVEF and no signs of HF (HR, 0.71; 95% CI, 0.66–1.01; p = 0.06; interaction p value between treatment and HF = 0.63). In terms of LVEF categories, patients with preserved LVEF and those with midrange LVEF had similar risks for the primary outcome (HR for midrange versus preserved LVEF, 1.01 [0.68–0.50]), while patients with preserved LVEF had a lower risk for the first primary outcome compared to those with reduced LVEF (HR for reduced versus preserved LVEF, 1.76 [1.19–2.59]). Additionally, the prespecified sub-analyses of EAST-AFNET4 [38] categorized patients based on their comorbidities and age into higher CHA2DS2-VASc scores (≥ 4) or lower CHA2DS2-VASc scores (< 4). Compared with usual care, ERC therapy reduced the composite primary efficacy outcome of cardiovascular death, stroke, or hospitalization for worsening of HF or acute coronary syndrome in patients with recently diagnosed AF and a high comorbidity burden, defined by a CHA2DS2-VASc score ≥ 4 (HR, 0.64 [0.51–0.81]; p < 0.001), but not in patients with CHA2DS2-VASc score < 4 (HR, 0.93 [0.73–1.19]; p = 0.56) [38]. In a post hoc analysis of the Catheter Ablation for Atrial Firbillation With Heart Failure (CASTLE-AF) trial, an AF burden of < 50% at 6 months following catheter ablation was associated with a significant decrease in the primary composite outcome of mortality and HF hospitalization in patients with AF and HFrEF (HR, 0.33; 95% CI, 0.15–0.71; p = 0.014) [39]. Based on these findings, the 2023 ACC/AHA/ACCP/HRS guidelines for the diagnosis and management of AF state that in patients with a new diagnosis of HFrEF and AF, arrhythmia-induced cardiomyopathy should be suspected, and an early and aggressive approach to AF rhythm-control is recommended [2].
CATHETER ABLATION OF AF IN PATIENTS WITH HFrEF
Several studies have assessed the potential benefits of AF ablation in patients with HFrEF. In a multicenter randomized Ablation vs. Amiodarone for Treatment of Atrial Fibrillation in Patients With Congestive Heart Failure and an Implanted implantable cardioverter defibrillator (ICD)/cardiac resynchronization therapy defibrillator (CRT-D) [AATAC] trial [40], catheter ablation was compared with amiodarone in patients with persistent AF who had a dual-chamber ICD or CRT-D, NYHA class II to III, and a LVEF of 40% or less within the past 6 months. This study demonstrated that catheter ablation for AF is superior to amiodarone in achieving long-term freedom from AF and reducing unplanned hospitalization and mortality in patients with HF and persistent AF. Additionally, the ablation group exhibited significantly better outcomes in terms of quality of life (QoL) and exercise capacity. In the Catheter Ablation Versus Medical Rate Control in Atrial Fibrillation and Systolic Dysfunction (CAMERA-MRI) trial [41], patients with persistent AF, NYHA functional class II or greater, LVEF of 45% or less, and no significant coronary artery disease were enrolled. The 68 patients were randomized to either a catheter ablation group or a medical rate-control group, and LVEF was assessed using cardiac MRI at 6 months. The catheter ablation group showed a significant improvement in LVEF, with 58% of this cohort having normalized systolic function compared to 9% in the medical group (p = 0.0002). In addition, the secondary endpoints showed a reduction in LA and LV chamber dimensions, BNP levels, and NYHA functional class in the catheter ablation group. The 4-year long-term outcomes of this study revealed that catheter ablation for AF is superior to medical rate-control in improving LVEF [42]. There was an increase in LVEF of 16.4 ± 13.3% in the ablation group compared to 8.6 ± 7.6% in the medical group (p < 0.001), and within the catheter ablation group, the absence of ventricular late gadolinium enhancement was linked to a greater improvement in LVEF [42]. These findings indicate that LV dysfunction is related to arrhythmia-mediated cardiomyopathy and could potentially be reversed by maintaining the sinus rhythm through catheter ablation.
The CASTLE-AF study [43] included patients with symptomatic paroxysmal or persistent AF and HF of NYHA class II or above, with LVEF of 35% or less and ICD who were unresponsive or intolerant to antiarrhythmic drugs. In this study, 363 patients were randomly assigned to receive either catheter ablation or medical therapy (rate or rhythm-control) for AF, in addition to guideline-based therapy for HF. At 3.2 years follow-up, the catheter ablation group was associated with significantly lower rates of the primary endpoint, which included death from any cause or hospitalization for worsening HF (28.5% vs. 44.6%; HR, 0.62; 95% CI, 0.43–0.87; p = 0.007). Mortality was also significantly lower in the catheter ablation group (13.4% vs. 25.0%; HR, 0.53; 95% CI, 0.32–0.86; p = 0.01), as was hospitalization for worsening HF (20.7% vs. 35.9%; HR, 0.56; 95% CI, 0.37–0.83; p = 0.004) and death from cardiovascular disease (11.2% vs. 22.3%; HR, 0.49; 95% CI, 0.29–0.84; p = 0.009). These findings suggest that catheter ablation has a significant positive impact on patient prognosis.
In another randomized controlled trial, Catheter Ablation Versus Medical Treatment of Atrial Fibrillation in Heart Failure (CAMTAF) trial [44], patients with persistent and symptomatic HF (NYHA class II–IV) with < 50% LVEF were randomized into either catheter ablation or medical rate-control groups. The baseline LVEF was 32 ± 8% in the ablation group and 34 ± 12% in the medical group. At 6 months follow-up, LVEF was 39.9% (CI, 35.2–44.7%) in the ablation group compared with 31.0% (CI, 25.5–36.6%) in the medical group (p = 0.015). The improvement in LV function in the ablation group persisted at 1 year follow up. Exercise capacity, BNP levels, NYHA class, HF symptoms, and QoL were also improved in the catheter ablation group compared to those in the medical cohort. Furthermore, a recent single-center randomized study comparing catheter ablation and guideline-directed medical therapy (GDMT) with GDMT alone in patients with symptomatic AF and end-stage HF referred for cardiac transplantation evaluation found that the composite of all-cause mortality, left ventricular assist device (LVAD) implantation, or urgent cardiac transplantation was lower in the catheter ablation and GDMT alone group after a median follow-up of 18 months (8% vs. 30%; HR, 0.24; p < 0.001) [45]. In a stratified, pooled analysis of randomized data comparing catheter ablation rhythm-control versus medical therapy in patients with AF and HF, the results showed that AF ablation was associated with significantly lower all-cause mortality, reduced rehospitalization, and greater improvement in LVEF than medical therapy [46]. A systematic review and meta-analysis of clinical trials evaluating the benefits of catheter ablation for patients with AF and HF also showed that catheter ablation reduces all-cause mortality and improves LVEF compared to medical therapy [47-49]. Table 1 summarizes randomized controlled trials comparing catheter ablation and medical therapy in patients with AF and HFrEF.
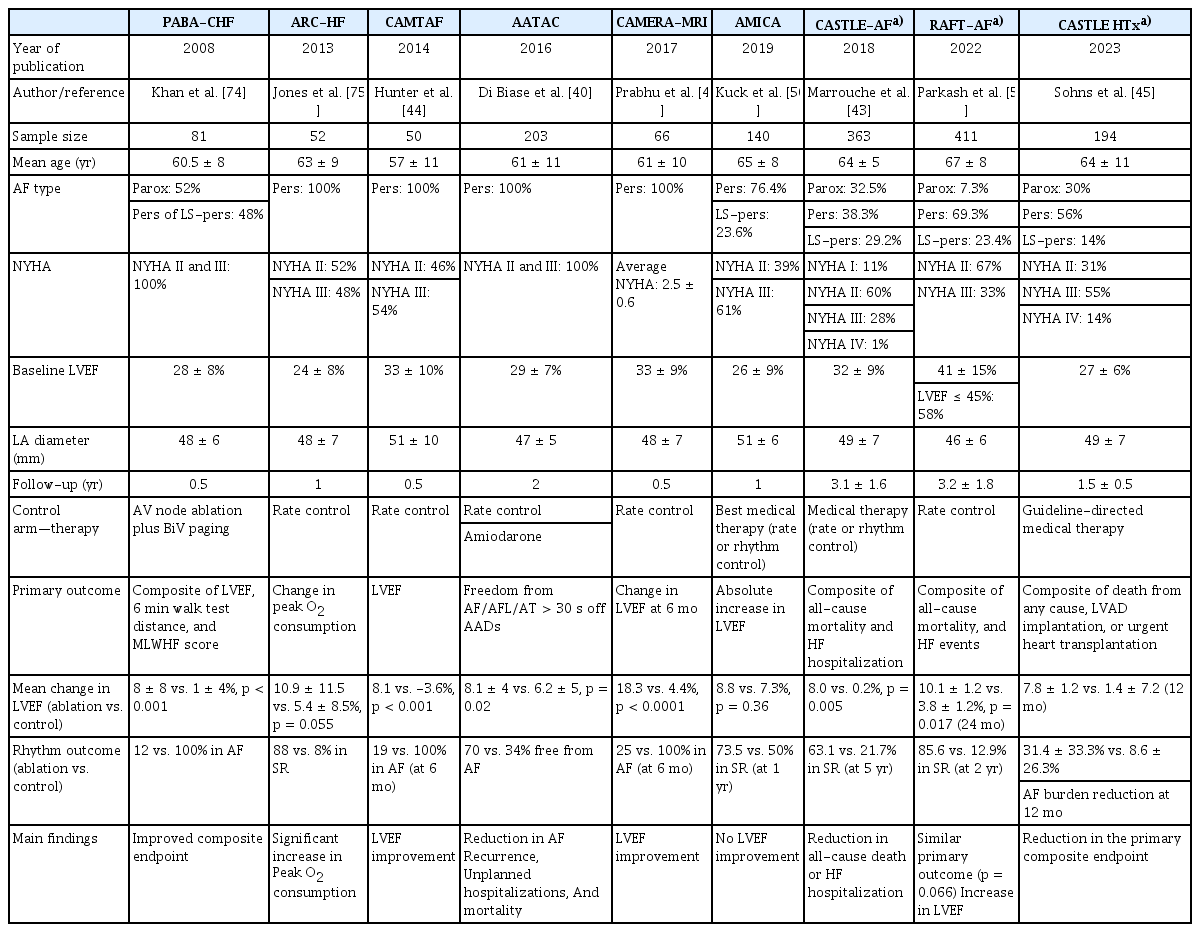
Randomized controlled clinical trials comparing catheter ablation vs. medical therapy in patients with atrial fibrillation (AF) and heart failure (HF) with reduced ejection fraction
However, it is difficult to improve patients with more advanced HF with catheter ablation because they are more likely to have myocardial dysfunction due to structural changes that are unrelated to AF. In the Atrial Fibrillation Management in Congestive Heart Failure With Ablation (AMICA) trial, a randomized trial comparing catheter ablation of AF and best medical therapy for patients with persistent or long-standing persistent AF and LVEF ≤ 35%, no benefit of catheter ablation was observed in terms of LVEF increase, QoL, BNP, and 6-min walk test results. This trial included patients with relatively lower LVEF (27.6% vs. 32.5% in CASTLE-AF), a higher prevalence of persistent or long-standing persistent AF (100% vs. 70% in CASTLE-AF), more severe HF symptoms of NYHA class III or IV (60% vs. 31% in CASTLE-AF), and more often had a CRT-D implanted (43% vs. 27% in CASTLE-AF) [50]. Factors predicting the lack of LVEF recovery after catheter ablation in patients with impaired LV systolic function included advanced NYHA class (III/IV), ischemic HF etiology, paroxysmal AF, prolonged QRS duration (> 120 ms), severe LA dilatation (LA volume index > 50 mL/m2), and atrial and ventricular fibrosis [51-56]. In addition, patients who first develop HF tend to have worse prognosis, are less likely to exhibit AF-mediated cardiomyopathy, and experience poorer outcomes after AF ablation [57,58]. A recent study demonstrated that a score comprising four parameters (wide QRS, HF etiology, severe atrial dilatation, and paroxysmal AF) can predict improvement in LV systolic function in patients with HF undergoing AF ablation [55,56]. Therefore, identifying patients with HFrEF who may benefit from AF ablation is important.
Based on these data, the 2023 ACC/AHA/ACCP/HRS guidelines for the diagnosis and management of AF recommend catheter ablation as a Class 1 treatment for patients with AF and HFrEF who have a high probability of arrhythmia-induced cardiomyopathy or are on GDMT and are expected to benefit from the procedure. This recommendation aims to improve the symptoms, QoL, ventricular function, and cardiovascular outcomes [2].
The Catheter Ablation for Atrial Fibrillation in Patients with End-Stage Heart Failure and Eligibility for Heart Transplantation (CASTLE-HTx) trial [45] trial, a recently published single-center, open-label, randomized clinical trial, assessed the efficacy of catheter ablation combined with GDMT versus medical therapy alone in patients with end-stage HF and symptomatic AF who were evaluated for eligibility for heart transplantation or implantation of a LVAD. A total of 194 patients with a median follow-up period of 18 months were enrolled between November 2020 and May 2022. The primary end point—a composite of death from any cause, LVAD implantation, or urgent heart transplantation—occurred in eight patients (8%) in the ablation group and 29 patients (30%) in the medical-therapy group (HR, 0.24; 95% CI, 0.11–0.52; p < 0.001). In a meta-analysis of catheter ablation for AF in patients with HFrEF [59], which included data from the CASTLE-HTx trial, catheter ablation was significantly associated with reduced HF hospitalization (RR, 0.57; 95% CI, 0.45–0.72; p < 0.01), cardiovascular mortality (RR, 0.46; 95% CI, 0.31–0.70; p < 0.01), all-cause mortality (RR, 0.53; 95% CI, 0.36–0.78; p < 0.01), and AF burden (mean difference, -29.8%; 95% CI, -43.73% to -15.90%; p < 0.01) when compared to that in a medical therapy group. In addition, significant improvements in LVEF and QoL were observed in the ablation group.
The results of the CASTLE-HTx trial support the consideration of catheter ablation for AF as a first-line treatment in patients with advanced HF, in contrast to the findings of the AMICA trial. The mean LVEF in AMICA and CASTLE-HTx trials were similar, at 26 ± 9% and 27 ± 6%, respectively. However, the AMICA group had a higher prevalence of persistent or long-standing persistent AF (100% vs. 71% in the CASTLE-HTx group). The AMICA was a multicenter trial that included 17 centers, whereas the CASTLE-HTx was a single-center trial. The recruitment rate in AMICA was 0.12 patients per month per center, similar to other randomized multicenter trials, whereas the enrollment rate in CASTLE-HTx was significantly higher at 10.2 patients per month per center [60]. Additionally, the 1-year mortality rate in the control group of the CASTLE-HTx trial was 15% to 20%, which is considerably lower than the expected 1-year mortality rate of 50% in patients with end-stage HF [60]. Further research, including multicenter trials focusing on patients with advanced HF, is required.
CATHETER ABLATION OF AF IN PATIENTS WITH HFpEF AND HFmrEF
Although there is a substantial amount of data regarding catheter ablation for AF in patients with HFrEF, large-scale studies in patients with HFpEF and HFmrEF are limited, and there are virtually no studies concerning AF ablation, specifically in patients with HFmrEF. In the prespecified subgroup analyses of the Catheter Ablation Versus Antiarrhythmic Drug Therapy for Atrial Fibrillation (CABANA) trial [61], 778 patients with NYHA class II or greater HF symptoms recorded at baseline were randomized to AF ablation or drug therapy, with data on index EF available for 571 patients. Catheter ablation of AF reduced all-cause mortality (HR, 0.57 [95% CI, 0.33–0.96]) and AF recurrence (HR, 0.56 [95% CI, 0.42–0.74]) compared with drug therapy alone. Patients in the ablation group also showed improvements in QoL after 5 years. In this subgroup analysis, 9.8% of patients had LVEF < 40%, 15.6% had LVEF 40–49%, and 74.6% had EF ≥ 50%, with a high proportion of HFpEF. In pooled data from two Japanese multicenter registries screening 899 AF patients with LVEF ≥ 40%, patients who underwent catheter ablation showed a significantly lower incidence of the primary endpoint (composite of cardiovascular death and hospitalization for HF) at 24.6 months follow-up compared with those who underwent medical therapy (HR, 0.32; 95% CI, 0.13–0.70; p = 0.004) [62]. A small randomized controlled trial of 31 patients in Australia compared catheter ablation with usual medical therapy in patients with clinical HFpEF with symptomatic or persistent AF [63]. At 6 months follow-up, the ablation group showed a reduction in peak pulmonary capillary wedge pressure (PCWP) from baseline (30.4 ± 4.2 to 25.4 ± 4.5 mmHg; p < 0.01) and an improvement in peak relative VO2 (20.2 ± 5.9 to 23.1 ± 7.2 mL/kg/min; p < 0.01) and a decrease in N-terminal pro-B-type natriuretic peptide levels (794 ± 698 to 141 ± 60 ng/L; p = 0.04). QoL was also improved, but no significant differences were found in the medical therapy group [63]. Evidence from registries and observational studies suggests that catheter ablation, compared with medical therapy, significantly reduces arrhythmia recurrence and risk of cardiovascular events in patients with HF across the LVEF spectrum, including those with HFpEF [64-67].
recent meta-analysis compared catheter ablation with usual medical therapy in patients with AF and HFpEF [68]. It included data from 20,257 patients across eight studies comprising three randomized controlled trials and five observational studies. Patients with HFpEF who underwent catheter ablation had significantly lower risks of cardiovascular and all-cause mortality. Catheter ablation has also been associated with a reduced risk of hospitalization for HF and all-cause hospitalization. However, no significant differences were observed in terms of stroke risk. Based on these data, the 2023 ACC/AHA/ACCP/HRS guidelines for the diagnosis and management of AF recommend catheter ablation as a Class 2a treatment for patients with symptomatic AF and HFpEF who are expected to benefit from the procedure, as it can be useful for improving symptoms and QoL [2].
CATHETER ABLATION AS FIRST TREATMENT FOR AF AND HF
The timing of AF diagnosis and rhythm-control therapy affects prognosis, with an increased risk of cardiovascular complications during the first 12 months after AF diagnosis [69-71]. ERC within the first year of AF diagnosis improves cardiovascular outcomes even in patients with signs or symptoms of HF [37].
In a prospective trial examining the relationship between diagnosis-to-ablation times and ablation outcomes in patients with persistent AF, the study population was categorized into quartiles according to the time interval between the initial diagnosis of persistent AF and the ablation procedure (≤ 1, 1.1–3.0, 3.1–6.5, > 6.5 years). Arrhythmic recurrence rates increased significantly with longer diagnosis- to-ablation intervals, with 2-year recurrence rates of 33.6%, 52.6%, 57.1%, and 54.6% in the first, second, third, and fourth quartiles, respectively. Additionally, longer diagnosis-to-ablation times have been linked to atrial remodeling [72]. A systematic review and meta-analysis of 26 studies surrounding the safety and long-term outcomes of catheter ablation in patients with AF and LV systolic dysfunction found that outcomes improved when catheter ablation was performed early in the course of AF and HF [73]. A graphical summary of the pathophysiologic relationship between AF and HF, as well as the therapeutic effects of catheter ablation, is presented in Fig. 1.
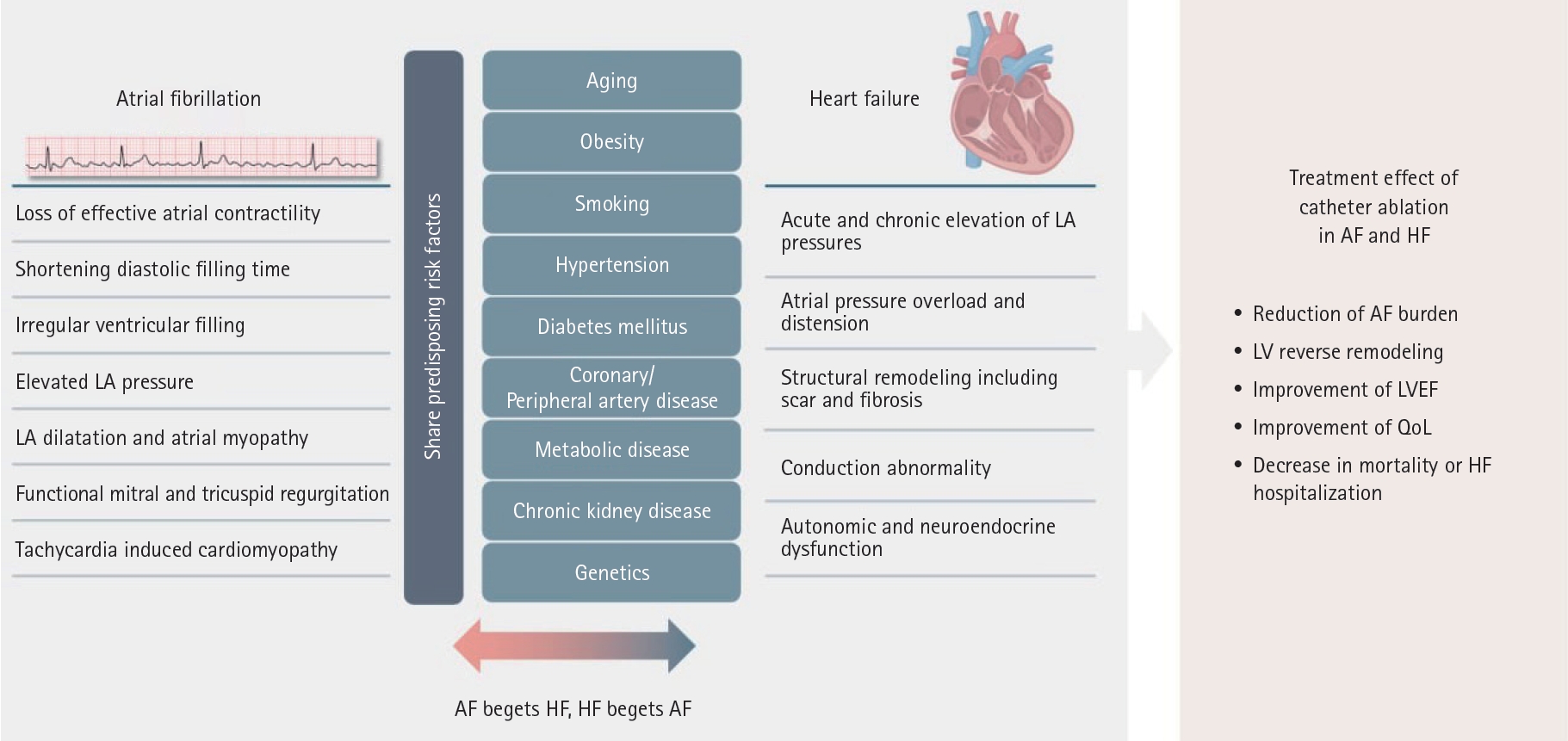
Graphical abstract: Interaction between atrial fibrillation (AF) and heart failure (HF) and the effects of catheter ablation treatment in patients with AF and HF. LA, left atrium; LV, left ventricular; LVEF, left ventricular ejection fraction, QoL, quality of life.
Prolonged AF leads to LA dilatation and shortens the effective refractory period of the atrium. This condition also increases LA pressure and PCWP, contributing to mitral and tricuspid regurgitation. Over time, this progression results in LA fibrosis and tachycardia-induced cardiomyopathy, which subsequently exacerbates HF and worsens the signs and symptoms of HF [11-13]. Furthermore, atrial and ventricular fibrosis and severely decreased LVEF are associated with poor outcomes following catheter ablation [41,50]. Recent randomized controlled trials have demonstrated that catheter ablation is an effective method for rhythm-control in patients with HF. With careful selection of the appropriate patient population in whom catheter ablation is likely to yield favorable outcomes, AF ablation could be considered to represent the preferred treatment strategy over antiarrhythmic drugs as a rhythm control strategy for managing AF in patients with HF.
ONGOING RESEARCH AND CLINICAL TRIALS IN AF ABLATION FOR HF
There is growing evidence supporting the use of catheter ablation for the treatment of AF in patients with HFrEF. The Randomized Ablation-Based AF Rhythm-Control Versus Rate-Control in Patients with HF and High-Burden AF Extend (RAFT-AF Extend) trial (ClinicalTrials.gov: NCT05118893) is an extended study of the original RAFT-AF, providing an additional 24 months of follow-up to assess the long-term outcomes of ablation-based rhythm-control versus rate-control in patients with HF with high-burden AF.
Data regarding AF ablation outcomes in patients with HFpEF and HFmrEF are limited compared to those in patients with HFrEF. Ongoing randomized controlled trials are being conducted to address this lack of clinical trial data on catheter ablation for AF in patients with HFpEF or HFmrEF. The Catheter-Based Ablation for AF Compared to Conventional Treatment in Patients with HFpEF (CABA-HFPEF) trial (ClinicalTrials.gov: NCT05508256) assessed the effects of catheter ablation of AF in patients with HFpEF and HFmrEF as an initial rhythm-control therapy compared to those of antiarrhythmic drug therapy. In addition, the Treatment of Atrial Fibrillation In Preserved Cardiac Function Heart Failure (TAP-CHF) trial (ClinicalTrials.gov: NCT04160000) was designed to compare catheter ablation with medical therapy in patients with AF and HFpEF with the goal of determining an optimal management strategy for this group of patients. Further studies are needed, including those on catheter ablation in patients with advanced HF, optimal patient selection and timing of ablation, and the outcomes of catheter ablation in patients with HFpEF and HFmrEF.
CONCLUSION
AF and HF are coexisting conditions that mutually worsen each other, and various studies have been conducted to explore treatment approaches. While earlier studies, which often used outdated methodologies and treatment approaches, did not show any benefit in re-establishing and maintaining sinus rhythm, recent research strongly suggests that maintaining sinus rhythm leads to better clinical outcomes in patients with HF across the LVEF spectrum, particularly in those with HFrEF. Several randomized controlled trials and observational studies have shown that using catheter ablation as a rhythm-control strategy in patients with HF and AF improves LV function, HF symptoms, AF recurrence, hospitalization rates, and mortality. Given these findings, and considering that the treatment options for patients with advanced HF are limited, catheter ablation could be beneficial for managing AF in patients with HF, particularly in selected individuals. Additional studies are needed to improve patient selection, determine the optimal timing for ablation, and assess long-term outcomes.
Notes
CRedit authorship contributions
Min-Su Jung: methodology, resources, investigation, data curation, formal analysis, validation, writing – original draft, writing – review & editing, visualization, supervision, project administration; Hyoung-Seob Park: conceptualization, methodology, resources, investigation, data curation, validation, writing – review & editing, visualization, supervision, project administration
Conflicts of interest
The authors disclose no conflicts.
Funding
None
