Physical activity for prevention of cardiovascular disease: consensus statement of Korean Society of Cardio-cerebrovascular Disease Prevention
Article information
Abstract
Cardiovascular disease (CVD) remains the leading cause of mortality worldwide, highlighting the need for effective preventive strategies. This consensus statement emphasizes the critical role of regular physical activity, including aerobic and muscle-strengthening exercises, in reducing key CVD risk factors such as hypertension, dyslipidemia, obesity, and insulin resistance. Recommendations are provided for the general adult population as well as specific subgroups, including older adults, pregnant and postpartum women, individuals with CVD, and those with physical limitations. The importance of reducing sedentary behavior and integrating physical activity into daily life is also addressed. Recommendations should focus on tailored interventions, supportive environments, and evidence-based policies that encourage active lifestyles. Further research specific to the Korean population will enhance the development of evidence-based, population-tailored guidelines for more effective CVD prevention in Korea.
INTRODUCTION
Cardiovascular disease (CVD) is a critical public health issue worldwide and was responsible for approximately 20.5 million deaths from a cardiovascular condition in 2021, accounting for approximately one-third of all global deaths [1]. Physical inactivity is a significant modifiable risk factor for non-communicable diseases, including CVD [2], alongside other factors such as hypertension, obesity, and smoking. Regular physical activity has been shown to mitigate these risks significantly and offers protective benefits against the development and progression of CVD. In Korea, a large-scale cohort study using the National Health Screening data demonstrated that individuals meeting recommended physical activity levels had significantly lower all-cause mortality and cardiovascular mortality over a 7-year follow-up, compared with those insufficiently active [3]. These findings underscore the importance of promoting adequate physical activity within the Korean population.
Physical activity is defined as any bodily movement produced by skeletal muscles that requires energy expenditure [4]. Conversely, exercise, a subset of physical activity, is planned, structured, repetitive, and designed to improve or maintain physical fitness, performance, or health. Previously, the focus was primarily on exercise; however, there is a growing recognition that unstructured physical activity also confers health benefits. This shift reflects increasing concern over the harmful effects of prolonged sedentary behavior, which is becoming more prevalent. Consequently, the emphasis has been expanded to include general physical activity to counteract the risks of a sedentary lifestyle. Physical inactivity refers to not meeting the recommended levels of physical activity. Sedentary behavior is any waking behavior characterized by an energy expenditure of 1.5 metabolic equivalents of tasks (METs) or lower while sitting, reclining, or lying. Desk-based office work, driving a car, and watching television are examples of sedentary behavior, which can also apply to those unable to stand, such as wheelchair users (definitions of terms in Table 1).
This consensus statement aimed to consolidate the current evidence and provide clear, actionable guidelines on the role of physical activity in preventing CVD. This consensus also aimed to guide healthcare practitioners and policymakers on implementing effective physical activity interventions tailored to the Korean context. It was developed by the Clinical Practice Guidelines Committee of the Korean Society of Cardio-cerebrovascular Disease Prevention over the years 2023–2024 through two dedicated sessions at international academic meetings involving expert panel discussions and open forums with society members, followed by iterative evidence reviews and multiple rounds of internal revisions to achieve final agreement among committee members.
EPIDEMIOLOGY OF CVD
CVD is the leading cause of death globally [1]. Although the absolute number of CVD-related deaths has increased over the past 30 years, largely because of an aging and expanding population, the age-standardized death rate has declined [5]. However, this decline is uneven across regions, with the most significant reductions observed in high-income countries, whereas low-income regions experience a slower decline, reflecting disparities in healthcare access and the management of CVD risk factors [5].
In Korea, CVD accounts for a substantial proportion of morbidity and mortality; heart disease is the second leading cause of death after cancer, and cerebrovascular disease was the fifth leading cause of death in 2022 [6]. According to recent data, the prevalence of CVD-related conditions such as hypertension, diabetes, obesity, and dyslipidemia has been steadily increasing [7-10].
Current status in sedentary behavior or physical activity
A comprehensive meta-analysis by Ekelund et al. [11] reported a dose-response association between the risk of all-cause mortality and increased sitting time in combination with lower levels of activity. High levels of moderate-intensity physical activity (i.e., approximately 60–75 minutes per day) attenuate but do not eliminate the increased risk associated with high TV viewing time. The Korea National Health and Nutrition Examination Survey (KNHANES) revealed a concerning trend: a significant proportion of the adult population fails to meet the recommended levels of physical activity. In 2021, Korean adults aged 19 years and older spent an average of 8.9 hours per day on sedentary behavior, with 63.7% spending more than 8 hours per day on sedentary behavior [12]. The overall prevalence of adults in Korea meeting the World Health Organization (WHO) physical activity recommendations [4] was 44.9%. This included 18.8% who engaged in at least 150 minutes of moderate-intensity aerobic physical activity per week and an additional 26.1% who achieved higher levels of activity for additional health benefits–300 minutes or more of moderate-intensity or vigorous-intensity aerobic physical activity in a week, or 150 minutes or more of vigorous-intensity aerobic physical activity, or an equivalent combination of both [12]. A total of 24.8% of adults in Korea performed muscle-strengthening activities at least 2 days a week. The decline in physical activity levels was accentuated during the coronavirus disease 2019 pandemic, with the prevalence of adequate physical activity decreasing significantly from 36.0% in 2017–2019 to 30.0% in 2020, and further to 29.7% in 2021, according to data from the Korea Community Health Survey, which was conducted by the Korea Disease Control Agency [13]. This decrease underscores the impact of pandemic-related restrictions and lifestyle changes on physical activity habits.
Similarly, in the United States, 46.9% of adults met the guidelines for aerobic physical activity, and 24.2% adhered to the guidelines for both aerobic and muscle-strengthening activities [14]. Among European adults, 33.2% attain the recommended level of physical activity [15]. These worldwide trends highlight the critical need for public health strategies to promote physical activity and reduce sedentary behavior as preventive measures against CVD. In 2018, the World Health Assembly approved the Global Action Plan on Physical Activity 2018–2030 [16], setting a voluntary global target to reduce physical inactivity by 15% by 2030. The WHO urges all countries to establish national guidelines and set targets for physical activity. To support populations in achieving these goals and maintaining healthy physical activity levels, countries are encouraged to develop and implement policies and programs at both national and subnational levels.
MECHANISMS BY WHICH PHYSICAL ACTIVITY PREVENTS CVD
Physiological benefits of physical activity
Regular physical activity, particularly aerobic exercise, enhances cardiorespiratory fitness (CRF) by increasing oxygen consumption and cardiac output, leading to beneficial exercise-induced cardiac remodeling such as increased left ventricular mass, improved diastolic filling, and augmented stroke volume [17-19]. Aerobic exercise also improves vascular health by increasing capillary density and nitric oxide availability, enhancing endothelial function and blood flow [20,21]. It may protect against life-threatening arrhythmias by enhancing the cardiac autonomic balance, increasing the parasympathetic tone, and reducing sympathetic activity [22-24]. Resistance exercise complements these effects by improving muscle strength, bone density, and left ventricular hypertrophy, while lowering blood pressure [25-27].
Physical activity exerts anti-inflammatory effects by reducing systemic markers such as C-reactive protein and interleukin-6 [28-31]. Skeletal muscle also acts as an endocrine organ, releasing myokines during contractions, which help reduce inflammation and insulin resistance, protecting against atherosclerosis progression and promoting plaque stability [21,32,33].
A recent 18 F-fluorodeoxyglucose positron emission tomography/computed tomography study showed that regular physical activity reduces CVD risk by lowering stress-related brain activity, particularly in the amygdala, with notable benefits in individuals with depression [34]. This finding indicates both the direct cardiovascular and indirect psychological benefits of physical activity.
Impact on cardiovascular risk factors
Aerobic exercise lowers both systolic and diastolic blood pressure, with effects comparable to antihypertensive medications [35,36], through improved endothelial function, greater nitric oxide bioavailability, and reduced arterial stiffness [37]. It improves lipid profiles by raising high-density lipoprotein cholesterol levels and lowering triglyceride levels, though effects on low-density lipoprotein cholesterol are less consistent [38]. Regular activity enhances insulin sensitivity, glucose uptake, and skeletal muscle capillarization, partly via GLUT4 translocation [39,40], reducing glycated hemoglobin (HbA1c) by 0.6–0.8%—a benefit similar to some oral antiglycemic agents [18,41]. These effects occur even without weight loss and are particularly beneficial in those with high baseline insulin resistance. When combined with calorie restriction, high physical activity supports weight loss, long-term weight maintenance, and the prevention of gradual weight gain, thereby lowering the risk of overweight and obesity [42-45].
CLINICAL EVIDENCE SUPPORTING PHYSICAL ACTIVITY IN CVD PREVENTION
Evidence supporting physical activity as a preventive strategy against CVD is robust and compelling. Several studies have consistently demonstrated a dose-response relationship between physical activity levels and the reduction of CVD risk factors such as blood pressure, body weight, blood glucose, or lipid profiles [46]. This relationship has been observed in disease states such as hypertension, obesity, diabetes mellitus, CVD, and mortality.
Aerobic physical activity can lower systolic and diastolic blood pressures in patients with essential hypertension by a mean of 7 and 5 mmHg, respectively [47,48]. Each 10 MET hours per week increase in leisure-time physical activity or simply meeting the recommended minimum level of moderate physical activity is associated with a 6% reduction in the risk of hypertension [49]. Furthermore, meeting physical activity guidelines can decrease the incidence of type 2 diabetes mellitus (T2DM) by 26–35%, and this benefit is observed irrespective of body weight [46,50]. Longitudinal studies have reinforced these findings, showing that sustained physical activity over time is associated with lower incidence rates of coronary heart disease, stroke, heart failure, and T2DM [50-53]. Compared with inactive adults, meeting physical activity guidelines is associated with a 14% reduced risk of developing coronary heart disease [51]. In a large-scale Korean study using the National Health Insurance Service (NHIS) cohort (2009–2012; n = 294,528 adults newly diagnosed with T2DM), individuals who increased or maintained physical activity levels after diagnosis had a 21–23% lower risk of developing heart failure during follow-up through 2017 [54]. In addition, individuals who achieve a high level of physical activity show a 75% maximal risk reduction in all-cause mortality and approximately 40% reduction in CVD mortality [52,55]. A longitudinal trajectory study of Korean adults reported that even among individuals with increasing sedentary time, engaging in physical activity at least 2–3 times per week reduced incident CVD risk by approximately 30–50% [56]. A dose-response association between physical activity and CVD risk has also been demonstrated in a large Korean NHIS cohort study (2009–2012; n = 2,745,637 adults with T2DM; follow-up to 2017), with risk reduction particularly among those aged 65 years and older [57]. Notably, these benefits in reducing mortality can be achieved not only through the recommended levels of physical activity but also with relatively low levels of activity, such as modest step counts. A recent meta-analysis found that walking as few as 3,867 steps/day significantly reduced all-cause mortality, whereas walking 2,337 steps/day lowered cardiovascular mortality [43].
GUIDELINES AND RECOMMENDATIONS FOR PHYSICAL ACTIVITY IN CVD PREVENTION
Definition of terms related to physical activities
Physical activity is categorized into four main domains (Table 1): occupation, transportation, household, and leisure time [46]. Physical activity can occur at any time of the day and provides health benefits, regardless of its purpose. This includes non-leisure activities, such as transport-related physical activities (e.g., cycling to work), which are now acknowledged as valuable ways to promote physical activity. However, in a recent meta-analysis, occupational physical activity showed a non-significant trend in reducing the risk of coronary heart disease and stroke [53].
Exercise can be categorized into aerobic and anaerobic metabolic categories. Aerobic exercise, which is well-documented to improve CRF, uses the metabolism of stored energy through aerobic glycolysis, meaning that the body needs to deliver oxygen to the muscles, which allows the muscles to perform the activity [18,58]. In contrast, anaerobic exercise uses the metabolism of stored energy to be largely processed by anaerobic glycolysis. It requires short bursts of exercise and is not dependent on oxygen delivery alone [18,58]. Research suggests that combining resistance exercise with aerobic exercise provides enhanced benefits for CRF, muscle strength, and body composition compared to aerobic exercise alone [59]. This combination approach is also more effective than aerobic exercise alone in cardiac rehabilitation, serving as both a secondary prevention and treatment strategy for coronary artery disease [59,60].
The exercises can be performed at different intensities (Table 1). Intensity can be measured in different ways but can generally be determined using a talk test, which is commonly used in clinical settings. During moderate-intensity activity, a person can talk but not sing. During a vigorous-intensity activity, a person cannot say more than a few words without pausing for a breath.
Overview of current guidelines from WHO, American College of Cardiology/American Heart Association, and other relevant organizations
Internationally, organizations such as the WHO and the American College of Cardiology/American Heart Association (ACC/AHA) have provided clear guidelines on the recommended physical activity levels (Table 2) [4,61]. The recommendations for the general adult population in these guidelines are based on a scientific report [46] of the Physical Activity Guidelines for Americans, second edition (Table 2) [62]. Both organizations advocate at least 150–300 minutes of moderate-intensity aerobic activity per week or 75–150 minutes of vigorous-intensity activity supplemented with muscle-strengthening activities of moderate or greater intensity on at least 2 days per week. For additional health benefits, especially in managing weight, it is recommended that physical activity exceed 300 minutes per week [4,62,63].
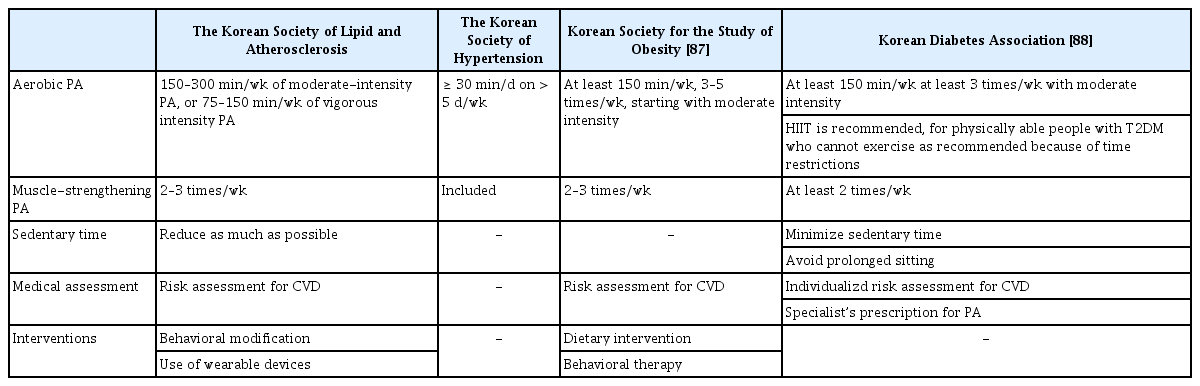
Physical activity recommendations of Korean organizations
When adapting these guidelines to the Korean context, it is crucial to consider cultural and environmental factors that may influence physical activity levels. The Korean Society of Lipid and Atherosclerosis, Korean Society of Hypertension, Korean Society for the Study of Obesity, and Korean Diabetes Association recommend physical activity based on principles similar to international guidelines, emphasizing at least 150 minutes/week of moderate-intensity aerobic activity or 75 minutes/week of vigorous activity, combined with muscle-strengthening activities on ≥ 2 days/week. However, their specific recommendations differed slightly in terms of type, duration, intensity, and frequency of physical activity, such as greater emphasis on minimizing sedentary time, the inclusion of high-intensity interval training (HIIT) for selected T2DM patients, and tailored strength or balance training for older adults (Table 3).
Duration and intensity of physical activity
The impact of sedentary behavior on cardiovascular health has been a focus since the WHO released its recommendations on physical activity in 2020 [4]. Prolonged sedentary time, generally considered to be in the range of 8–10 hours per day, has been associated with an increased risk of CVD [64-66]. In general, all individuals should be encouraged to “move more and sit less” throughout the day, regardless of the type of physical activity, as even small movements contribute to health benefits [4]. Interrupting sedentary time every 30–60 minutes with light-intensity activity has been linked to improvements in cardiometabolic health indicators [67].
There is no lower limit to the benefits of physical activity in reducing the risk of CVD. Unlike earlier guidelines, all physical activities contribute to the total recommended weekly amount regardless of the duration of each session [4]. Therefore, the ACC/AHA and European Society of Cardiology guidelines specifically state that even if individuals cannot meet the minimum recommended physical activity levels, engaging in some moderate- or vigorous-intensity physical activity or being as active as possible can still be beneficial in reducing the risk of CVD [58,61,68]. Even a few minutes of activity, such as parking farther away from the store or walking up the stairs instead of using the elevator, contributes to overall benefits [69]. The 150-minute target was based on obtaining benefits for the greatest outcomes. On the other end of the spectrum, additional physical activity confers additional benefits, and health risks are reduced with high amounts of physical activity, even beyond three to five times the 150-minute target weekly recommendation [46]. However, it should be noted that extremely high levels of physical activity, such as exceeding 10 times the minimum recommended amount, are relevant to only a small subset of the population and may carry potential cardiac risks, including myocardial fibrosis and atrial fibrillation, especially in those who are unfit or have underlying conditions [70]. While regular physical activity is beneficial for most individuals, very high volumes should be approached with caution, particularly in older adults and those with known structural heart disease, with intensity and workload gradually increased according to individual fitness and health status. For individuals with significant functional impairment, personalized recommendations should be provided by adjusting the type, duration, and intensity of physical activity to ensure safety and maximize health benefits, beginning at low levels and progressing gradually [61].
Frequency of physical activity
The total volume of moderate-to-vigorous physical activity was more critical than the specific number of days per week it is performed [71]. However, for certain benefits such as reduced anxiety, better sleep and executive function, lower blood pressure, and improved insulin sensitivity, engaging in physical activity regularly throughout the week may provide more sustained benefits [72].
Recommendation for older adults
For older adults (65 years and above), the general adult physical activity recommendations apply, with additional emphasis on balance, muscle strength, endurance, and functional training at moderate intensity for at least 3 days per week to enhance functional capacity and reduce falls [4,73]. Evidence shows a clear inverse relationship between aerobic activity volume and the risk of functional limitations [74-76]. Balance training significantly lowers fall rates, and multi-component activities reduce the risk of fall-related injuries [73]. Such physical activities also improve bone health and prevent osteoporosis. The same sedentary behavior recommendations for adults apply to this age group, given that the evidence includes those over 65 years of age [4]. In addition to physical activity, integrating supervised exercise interventions into healthcare services for older adults is crucial as these programs have proven effective in preventing functional decline and should be more widely implemented in primary and geriatric care settings to promote healthy aging [77].
Recommendation for pregnant and postpartum women
Engaging in physical activity is associated with reduced gestational weight gain and a lower risk of gestational diabetes in pregnant and postpartum women, especially in those with overweight or obesity. Exercise does not increase the risk of gestational hypertension, low birth weight, or small/large for gestational-age babies [46]. Regular moderate-intensity aerobic and muscle-strengthening activity is recommended for this group, and these activities should be continued throughout pregnancy unless medically contraindicated. General adult guidelines for sedentary behavior apply to pregnant and postpartum women.
Recommendation for people with CVD
For individuals with CVD, a thorough risk assessment is essential and should include physical examination, electrocardiography, and comprehensive clinical history. Low-risk patients (e.g., those with stable heart conditions or asymptomatic valvular disease) generally require no exercise restrictions [58]. However, high-risk patients should undergo further evaluation, including echocardiography, exercise stress testing, and potentially advanced imaging before starting physical activity. Screening is especially important for detecting conditions that may lead to sudden cardiac death. High-risk patients require individualized exercise plans and more frequent counseling as recommended by the guidelines [18,58]. Muscle-strengthening activities can be included as tolerated under professional guidance.
A concise summary of physical activity recommendations for specific population groups—including older adults, pregnant and postpartum women, individuals with CVD, and those with significant functional impairment—is presented in Table 4 for practical reference.
IMPLEMENTATION STRATEGIES
Implementing physical activity guidelines requires a multilevel approach. At the individual level, healthcare providers should integrate physical activity counseling into routine care, emphasizing its importance for cardiovascular health. Behavioral interventions, such as personalized goal setting and motivational interviewing techniques, can support patient engagement and adherence [78]. Recent Korean studies have shown that mobile- and remote-based interventions, including walking promotion programs using smart health devices, can effectively increase physical activity and improve cardiometabolic indicators, suggesting their potential as scalable strategies for CVD prevention [79,80]. At the community level, evidence indicates that infrastructure development (e.g., parks, bike lanes, pedestrian-friendly streets) is associated with increased physical activity participation rates. In Korean adults, neighborhood built-environment features and access to sports facilities have been positively associated with physical activity, underscoring the importance of improving walkability, park access, and facility availability in urban planning [81]. Additionally, public health campaigns can play a vital role in raising awareness of the benefits of physical activity and encouraging lifestyle changes.
Barriers and challenges
Despite the well-documented benefits of physical activity, several barriers hinder its adoption. Perceived time constraints, motivational deficits, and functional limitations have been consistently identified as individual-level barriers in epidemiologic surveys. Societal barriers include limited access to safe and convenient spaces for exercise and socioeconomic factors that may restrict participation in physical activities [82].
Addressing these barriers requires targeted interventions; for instance, workplace wellness programs can provide opportunities for employees to engage in physical activity during their workdays. Community initiatives should focus on making physical activity accessible and inclusive, particularly for underserved populations.
FUTURE DIRECTIONS
Future studies examining the long-term sustainability of various physical activity interventions are required to inform future guidelines. For example, HIIT involves alternating short bursts of intense anaerobic exercise with less intense aerobic recovery periods. Although HIIT can increase VO2 max and improve some cardiometabolic risk factors [83], including reducing HbA1c levels in individuals with T2DM [84], current evidence is limited regarding its long-term benefits, adherence in real-world settings, and potential risks—particularly in elderly or frail individuals. There are no standardized protocols for the duration or intensity of intervals, and most studies were shorter than 12 weeks, which may not be sufficient to assess sustained health impacts. Further longitudinal and mechanistic studies are warranted to elucidate the sustained physiological adaptations and safety profile of HIIT across heterogeneous patient populations.
In addition, recent studies have highlighted the growing interest in the timing of physical activity and its impact on health outcomes. While physical activity at any time of the day is beneficial, emerging observational evidence suggests a potential chronobiological modulation of the health benefits of physical activity, with timing potentially influencing cardiovascular outcomes. For instance, research from the UK Biobank indicates that engaging in moderate-to-vigorous physical activity during the midday to afternoon hours or having a mixed physical activity timing pattern may reduce the risk of all-cause and CVD mortality, especially in older adults and those with pre-existing conditions [85]. Another study found that late morning physical activity was associated with a lower risk of coronary artery disease and stroke, particularly among women [86]. Despite these promising findings, the optimal timing for physical activity remains unclear, and further research is needed to deepen our understanding of how physical activity timing or 'chronoactivity' can be leveraged for better health outcomes.
Future research should focus on identifying the most effective strategies for promoting physical activity in diverse populations. This includes exploring the role of emerging technologies such as artificial intelligence, machine learning, and wearable devices in personalizing physical activity recommendations, tracking progress, and providing real-time feedback to enhance engagement and adherence.
CONCLUSION
Physical activity is a proven strategy for preventing CVD, significantly reducing key risk factors, such as hypertension, dyslipidemia, and diabetes while enhancing fitness and metabolic health. Exercise-induced adaptations such as improved cardiac function and reduced inflammation are beneficial in diverse populations, including older adults and those with CVD. Thus, promoting regular physical activity is crucial to lower the incidence of CVD and improve public health. Collective efforts are needed to prioritize physical activity in public health. Even low-volume physical activity, when sustained, confers measurable reductions in cardiovascular morbidity and mortality at the population level, reinforcing its role as a cost-effective strategy in CVD prevention. Policymakers should create supportive environments, such as safe spaces for walking and cycling, to foster an active lifestyle and reduce the burden of CVD.
CONSENSUS STATEMENT
1. Regular physical activity that meets or exceeds the recommended physical activity guidelines reduces cardiovascular risk and mortality and plays an important role in both primary and secondary prevention for individuals of all backgrounds.
2. Adults should move more and sit less throughout the day. Some physical activities performed are better than none. Adults who sit less and perform moderate to vigorous physical activity gain some health benefits.
3. Adults should engage in at least 150 minutes/week of accumulated moderate-intensity or 75 minutes/week of vigorous-intensity aerobic physical activity for substantial health benefits.
4. Adults should also do muscle-strengthening activities of moderate or greater intensity, and that involve all major muscle groups ≥ 2 days a week, as these activities provide additional health benefits.
5. For adults aged ≥ 65 years, additional participation in varied multicomponent physical activity three or more times a week is advised, focusing on functional balance and muscle-strengthening activities at moderate or greater intensity to enhance functional capacity and prevent falls.
6. Pregnant and postpartum women should engage in at least 150 minutes of moderate-intensity aerobic physical activity per week, along with muscle-strengthening physical activities, as these reduce risks such as excessive gestational weight gain and gestational diabetes.
7. For individuals with cardiovascular disease, tailored physical activity plans should be developed based on thorough risk assessments with a focus on safe, regular aerobic, and muscle-strengthening physical activities to enhance cardiovascular health.
8. Adults with disabilities should engage in physical activity aligned with the recommendations for their age group, with adjustments based on individual abilities and conditions. Physical activity should begin at low levels and progressively increase in frequency, intensity, and duration as tolerated.
9. Supportive environments that encourage physical activity are essential for promoting active lifestyles and reducing the risk of cardiovascular disease at a population level.
Notes
CRedit authorship contributions
Ye Seul Yang: conceptualization, methodology, data curation, formal analysis, validation, writing - original draft, writing - review & editing; Eu Jeong Ku: writing - review & editing; Seung-Hyun Ko: conceptualization, methodology, validation, writing - review & editing, supervision, project administration; Eun-Jung Rhee: conceptualization, methodology, validation, writing - review & editing, supervision, project administration; Sang-Hyun Ihm: writing - review & editing; Sung Hee Choi: conceptualization, methodology, validation, writing - original draft, writing - review & editing, supervision, project administration; Won-Young Lee: writing - review & editing
Conflicts of interest
The authors disclose no conflicts.
Funding
None