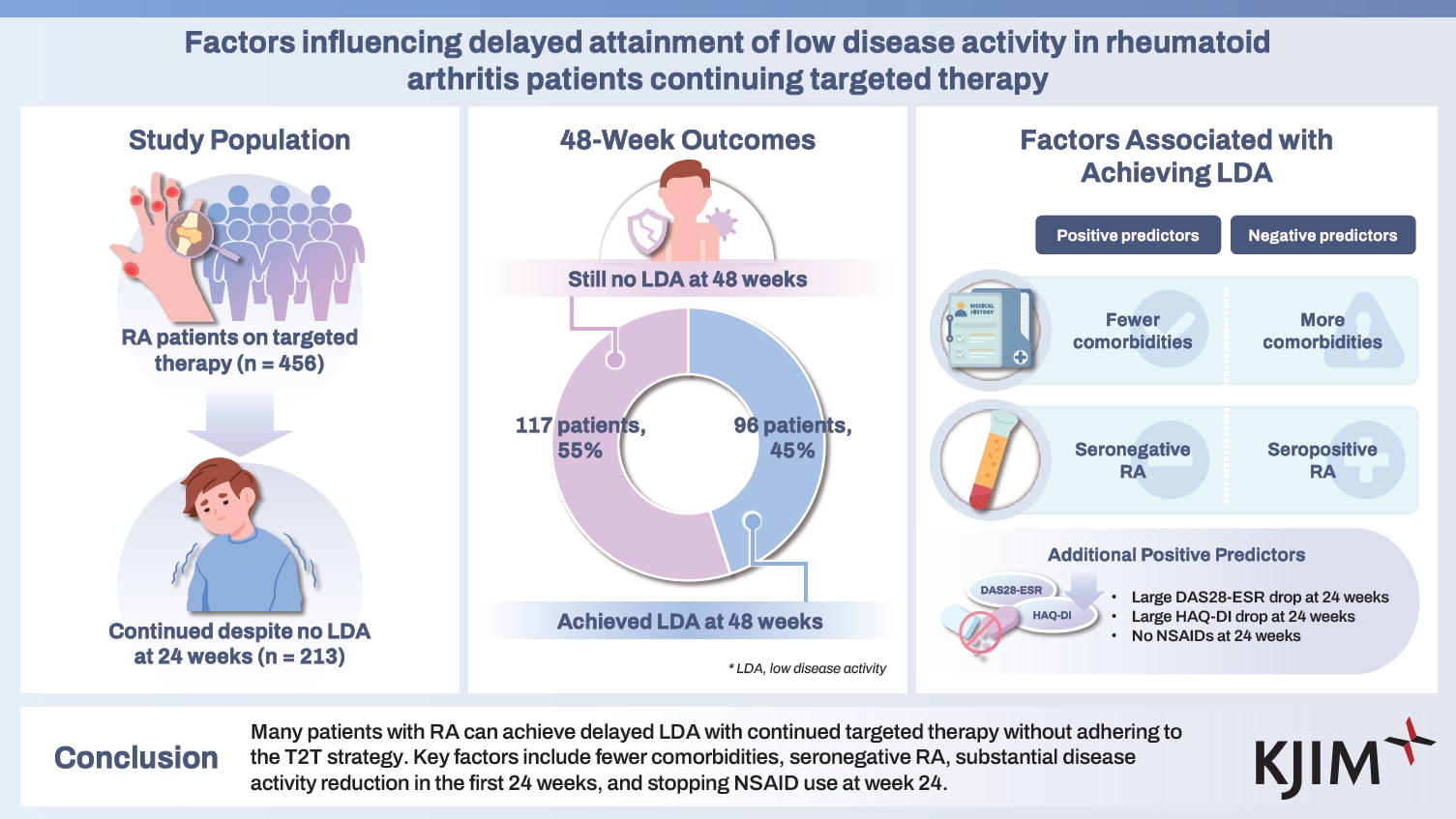
Factors influencing delayed attainment of low disease activity in rheumatoid arthritis patients continuing targeted therapy
Article information
Abstract
Background/Aims
To identify factors associated with achieving low disease activity (LDA) after 48 weeks of targeted therapy in patients with rheumatoid arthritis (RA) despite not meeting treat-to-target (T2T) criteria at week 24.
Methods
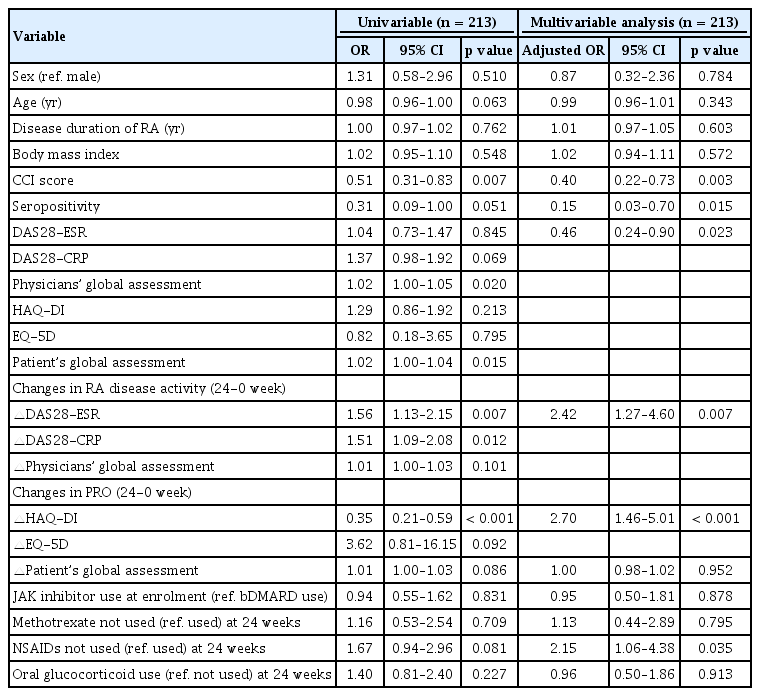
Data were collected from a multicenter, prospective observational cohort of Korea patients with RA receiving targeted therapy between April 2020 and July 2023. Patients who continued their initial targeted therapy despite not achieving LDA at week 24 were assigned to the LDA and non-LDA groups at week 48. Multivariable logistic regression was employed to identify factors associated with achieving delayed LDA at week 48.
Results
Among 456 patients with RA receiving targeted therapy, 213 were included in the analysis: 96 and 117 in the LDA and non-LDA groups, respectively. Patients with more comorbidities (HR 0.40, 95% CI 0.22–0.73) and those with seropositive RA (HR 0.15, 95% CI 0.03–0.70) were less likely to achieve LDA at week 48. Conversely, significant reductions in DAS28-ESR (HR 2.42, 95% CI 1.27–4.60) and HAQ-DI (HR 2.70, 95% CI 1.46–5.01) from enrolment to week 24, along with the absence of non-steroidal anti-inflammatory drug (NSAID) use at week 24 (HR 2.15, 95% CI 1.06–4.38), were associated with a greater likelihood of achieving delayed LDA at week 48.
Conclusions
Many patients with RA can achieve delayed LDA with continued targeted therapy without adhering to the T2T strategy. Key factors include fewer comorbidities, seronegative RA, substantial disease activity reduction in the first 24 weeks, and stopping NSAID at week 24.
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic inflammatory disorder that causes joint pain and damage [1]. Targeted therapies have transformed RA treatment, providing more effective options tailored to individual patient needs [2]. These therapies, including tumour necrosis factor (TNF), non-TNF, and Janus kinase (JAK) inhibitors, act on specific immune components, offering more precise mechanisms than conventional disease-modifying antirheumatic drugs (DMARDs) [2]. The introduction of targeted therapies in RA management has necessitated updates in clinical guidelines.
Current guidelines recommend a treat-to-target (T2T) strategy to achieve sustained remission or low disease activity (LDA) as the main goal in RA management [3,4]. The T2T approach focuses on meeting specific disease activity targets to optimize long-term outcomes [5]. This strategy improves clinical outcomes and quality of life for patients with RA by guiding treatment adjustments based on regular disease activity assessments [6,7]. However, one study found that T2T care did not increase the likelihood of treatment acceleration or achieving LDA [8].
Achieving remission or LDA within the recommended timeframe can be challenging in clinical practice. Monthly disease activity assessments are recommended for patients with high/moderate disease activity, while patients with sustained LDA or remission should be assessed less frequently, such as every 6 months [9]. The recent guidelines recommend adjusting therapy if the target is not reached within 6 months of treatment initiation [3]. The T2T strategy offers a structured approach; however, not all patients achieve LDA within this timeframe. Some patients continue their initial targeted therapy despite not meeting the LDA criteria at 6 months [10]. Understanding their long-term outcomes is crucial for optimizing treatment strategies.
Therefore, this study aims to evaluate the proportion of patients with RA who continue their initial targeted therapy after 24 weeks without achieving LDA and the factors contributing to late attainment of LDA at 48 weeks. Identifying these factors will provide insights into the effectiveness of sustained therapy and inform potential adjustments necessary for better patient outcomes.
METHODS
Data source
Data were collected from a multicenter prospective observational cohort of patients with RA in Korea who started targeted therapy. Rheumatologists from 17 centers (15 tertiary academic hospitals and 2 primary/secondary hospitals) recruited patients between April 2020 and August 2022. The cohort included patients aged ≥ 19 years who met the 1987 American College of Rheumatology (ACR) or 2010 ACR/European Alliance of Associations for Rheumatology (EULAR) classification criteria for RA. Only patients who had never received biologic DMARD or JAK inhibitor treatment were included. Those excluded were patients contraindicated for targeted therapy, planning for pregnancy or surgery, with a history of or current malignancy, or refused to provide written informed consent.
Data were collected from patients at enrolment and at weeks 12, 24, and 48. This included demographic and clinical information. Clinical data comprised comorbidities (Charlson Comorbidity Index score), duration of RA, seropositivity, drug use, RA activity, and patient-reported outcomes (PROs). Disease activity of RA and PROs was assessed at each visit using several measures: Disease Activity Score (DAS) 28 with erythrocyte sedimentation rate (ESR), Global Health assessment via visual analogue scale (VAS) by patients and physicians, Health Assessment Questionnaire-Disability Index (HAQ-DI), and EuroQol-5 dimension (EQ-5D).
Study population
This study included patients with RA from the cohort who were followed up until July 2023. Patients who dropped out before week 24 or had incomplete records were excluded. The analysis focused on patients who continued their initial targeted therapy despite not achieving LDA by week 24, excluding those who discontinued therapy for reasons unrelated to the T2T strategy, such as adverse event and financial problems. These patients were assigned to two groups based on their disease activity at week 48: those who achieved LDA (DAS28-ESR ≤ 3.2) as the LDA group and those with moderate or high disease activity (DAS28-ESR > 3.2) as the non-LDA group.
Statistical analyses
The proportion of patients who continued their initial targeted therapy despite not achieving LDA at week 24 was calculated. Baseline characteristics at enrolment were compared between the groups using the Mann–Whitney U test for continuous variables, while the chi-squared or Fisher’s exact tests were employed for categorical variables. Changes in RA disease activity and PROs were also compared between the two groups. A multivariable logistic regression model was used to identify factors associated with achieving LDA at week 48.
All analyses were conducted using SAS 9.4 software (SAS Institute, Cary, NC, USA). A p value of < 0.05 was considered statistically significant.
Ethical consideration
This study adhered to the Declaration of Helsinki and received approval from the Institutional Review Board (IRB) of Hanyang University Hospital (IRB No. HYUH 2022-04-020). Written informed consent was obtained from all patients at enrolment.
RESULTS
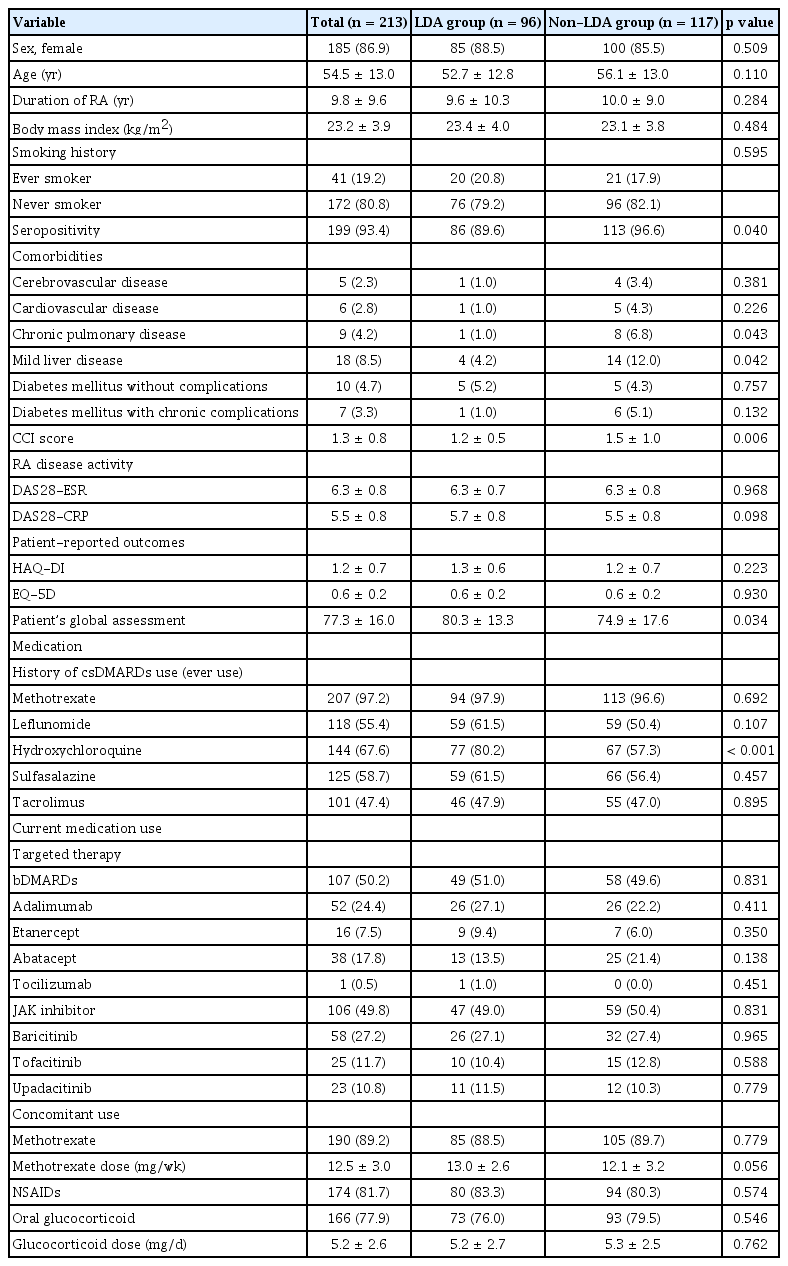
Baseline characteristics of the study population
Of the 456 patients with RA undergoing targeted therapy, 213 (46.7%) who continued their initial treatment despite not achieving LDA at 24 weeks were included in this study (Fig. 1). All 213 patients continued treatment until week 48 without any discontinuations. Based on the RA activity at week 48, the patients were categorized into two groups: 96 and 117 in the LDA and non-LDA groups, respectively. Thus, 45.1% of patients (96 of 213) who did not achieve LDA by week 24 but continued the targeted therapy until week 48 ultimately attained LDA.
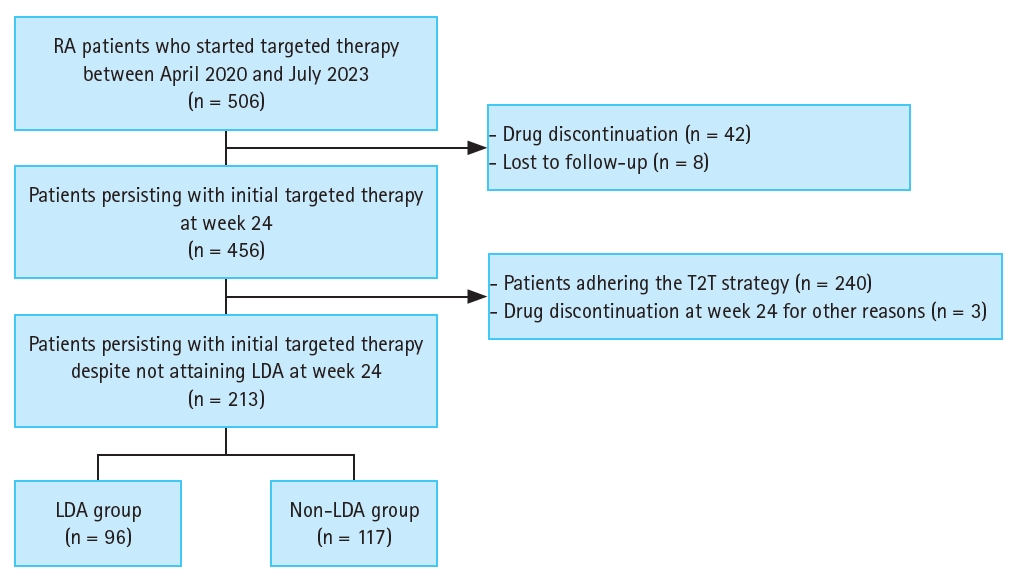
Patient selection flow chart. RA, rheumatoid arthritis; T2T, treat-to-target; LDA, low disease activity.
The mean age of the study population was 54.5 years, with 86.9% being female (Table 1). No significant demographic differences were observed at enrolment between the LDA and non-LDA groups. However, seropositive RA was more common in the non-LDA group (96.6% vs. 89.6%, p = 0.040). Patients in the non-LDA group also had higher proportions of comorbidities, including chronic pulmonary (6.8% vs. 1.0%, p = 0.043) and mild liver diseases (12.0% vs. 4.2%, p = 0.042). Additionally, no differences were observed between the two groups in RA activity measured using DAS28-ESR and CRP or in PROs such as HAQ-DI and EQ-5D. However, both physician and patient global assessments on the VAS were higher in the LDA group. No significant differences were observed in the concomitant usage of methotrexate or the type of targeted therapy between the two groups.
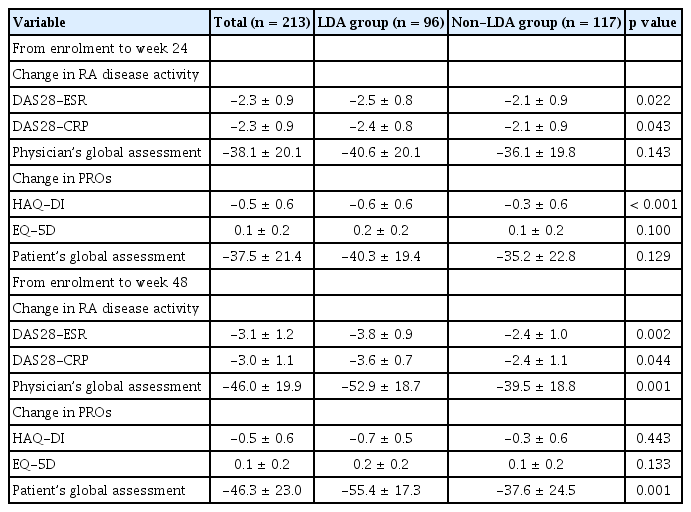
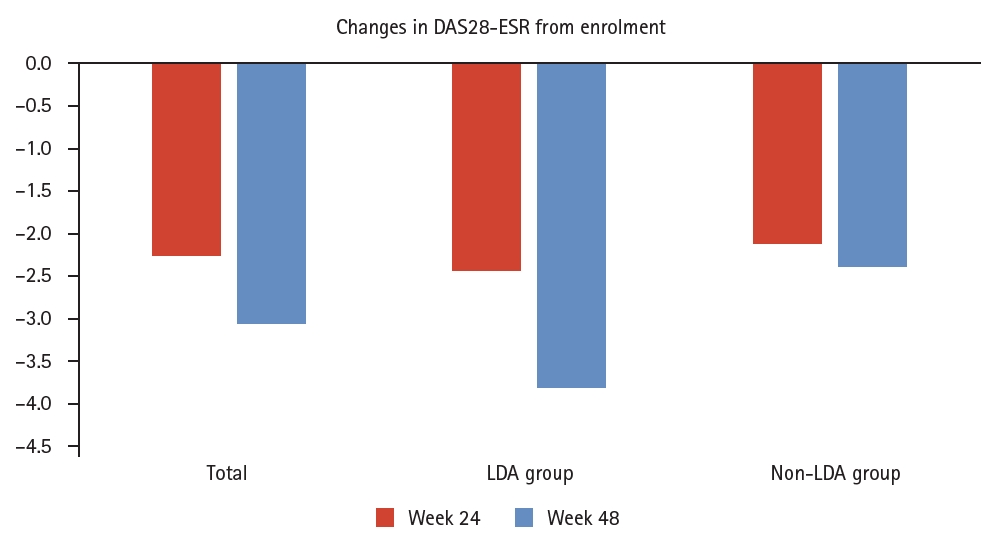
Changes in RA disease activity and PROs from enrolment to week 24
At week 24, the improvements in RA activity from enrolment, as measured using DAS28-ESR (-2.5 ± 0.8 vs. -2.1 ± 0.9, p = 0.022) and DAS28-CRP (-2.4 ± 0.8 vs. -2.1 ± 0.9, p = 0.043), were significantly greater in the LDA group than in the non-LDA group (Table 2, Fig. 2). Additionally, the reduction in HAQ-DI was more pronounced in the LDA group from enrolment to week 24 than in the non-LDA group (-0.6 ± 0.6 vs. -0.3 ± 0.6, p < 0.001).
Factors associated with the delayed attainment of LDA at week 48 in RA patients despite not achieving LDA at week 24
In the multivariable analysis, patients with more comorbidities (hazard ratio [HR] 0.40, 95% confidence interval [CI] 0.22–0.73) and those with seropositive RA (HR 0.15, 95% CI 0.03–0.70) were less likely to achieve LDA at week 48 (Table 3). Conversely, substantial reductions in DAS28-ESR (HR 2.42 per 1.0 decrease, 95% CI 1.27–4.60) and HAQ-DI (HR 2.70 per 1.0 decrease, 95% CI 1.46–5.01) from enrolment to week 24 were related to a higher likelihood of attaining LDA at week 48. Additionally, not using non-steroidal anti-inflammatory drugs (NSAIDs) at week 24 was associated with an increased chance of achieving LDA at week 48 (HR 2.15, 95% CI 1.06–4.38).
DISCUSSION
In this study, 213 of 456 patients (46.7%) with RA who initiated targeted therapy for moderate to high disease activity continued their initial treatment despite not achieving LDA at 24 weeks. However, this does not imply the T2T strategy was completely abandoned. Instead, it reflects cases where, after discussions between the patient and physician, the decision was made to continue the current treatment regimen despite not achieving the targeted DAS28-ESR or CRP LDA levels. Factors such as patient preferences or the clinical judgment of the physician may have influenced this decision. The same medication was maintained until week 48, by which time 45.1% (96 of the 213 patients) had attained LDA.
No significant differences were observed in demographic characteristics, medication use, and RA activity at enrolment between the LDA and non-LDA groups. However, patients in the non-LDA group had more comorbidities, and physician and patient global assessments using VAS were higher in the LDA group. The LDA group also showed greater improvements in DAS28-ESR and DAS28-CRP at week 24. Factors associated with achieving LDA by week 48 included fewer comorbidities, seronegativity for RA, greater reductions in DAS28-ESR and HAQ-DI from enrolment to week 24, and not using NSAIDs at week 24.
The first guidelines for the T2T strategy in patients with RA were introduced in 2010 by an international task force [11]. However, even before this, clinical trials had already shown that the T2T approach was superior to standard care [12,13]. Patients in the tight control group achieved higher proportions of LDA, better physical function, improved quality of life, and less radiographic progression. Several randomized controlled trials confirmed that systematic monitoring and timely treatment adjustments resulted in better clinical outcomes in RA [12-14]. However, these studies predominantly focused on patients with early RA and did not address the role of targeted therapies, which are now central to modern RA management. This distinction sets our study apart.
In Korea, a reimbursement code for measuring DAS28 in patients with RA has been in place since October 2023 [15,16]. This development highlights the growing recognition of the importance of regular quantitative disease activity assessments and the T2T strategy in managing RA. While the benefits of the T2T approach are well-documented, assessing how consistently it is followed in real-world clinical settings is equally important [17]. In this study, only 53.3% of patients adhered to the T2T strategy. Similarly, a recent study involving patients with RA from 10 countries indicates a 40.5% non-adherence rate during clinical visits, aligning with our findings [18]. Previous studies have also examined compliance with the T2T strategy, revealing that physician adherence is inconsistent, varies across different components of the strategy, tends to decline over time, and may often fall short of optimal levels [19]. However, other studies report successful implementation of the T2T strategy, with adherence rates ranging from 69.3% to 79%, depending on the specific protocols employed [20-22].
In real-world clinical practice, several factors hinder adherence to the T2T strategy, resulting in the continued use of targeted therapies even when LDA is not achieved. Previous studies have identified toxicities, comorbidities, smoking, and a high number of tender joints as key factors associated with the failure to implement the T2T strategy [18,23]. Patient preference also plays a significant role, often delaying necessary treatment escalation [8]. This reluctance to adjust medications, even when LDA is not reached, is largely driven by concerns over the potential risks and toxicities associated with new drug therapies [24]. Furthermore, patients may experience symptom relief even if their inflammatory markers improve gradually and the DAS28 score has not yet reached LDA. Our study supports this, showing that larger reductions in DAS28-ESR and HAQ-DI by week 24, along with the absence of NSAIDs use at week 24, were factors associated with achieving LDA by week 48. Fewer comorbidities and seronegativity for RA were also significant factors. However, further research is required before these can be considered as criteria for extending the waiting period for drug response rather than strictly following the T2T strategy.
Our study has several key strengths. First, it utilized data from a well-established cohort involving specialized rheumatology centers across South Korea. This cohort includes data from primary care facilities, general hospitals, and tertiary referral hospitals, offering real-world insights that improve the generalisability of our findings. Second, we employed multiple indicators to measure RA disease activity, including PROs, thereby diversifying the variables in our analysis. Third, all patients in this study were on their first targeted therapy. While numerous studies have explored the T2T strategy in the context of DMARDs for patients with RA, our focus on targeted therapies is a notable strength.
Despite its strengths, this study has some limitations. First, while we identified the proportion of non-adherence to the T2T strategy, we did not analyse the factors contributing to this non-adherence. Instead, our focus was on examining the prognosis of patients who deviated from the T2T strategy and assessing whether non-adherence could still result in acceptable outcomes. Second, the 48-week observation period may be too short to fully capture the long-term effects of the T2T strategy. In clinical practice, patients often undergo multiple changes in targeted therapy over a longer period. Therefore, studies with extended observational periods would be better suited for assessing real-world treatment sequences. Third, this study lacked data on radiographic joint assessments. Fourth, patients who achieved remission were not assessed separately, which is emphasized in clinical guidelines as a key RA treatment alongside LDA.
In conclusion, our study findings revealed that many patients with RA can achieve LDA even without strict adherence to the T2T strategy. Factors contributing to this positive outcome include fewer comorbidities, seronegative RA, significant reductions in disease activity between enrolment and week 24, and discontinuation of NSAIDs by week 24. These factors significantly increase the likelihood of achieving LDA by week 48. This suggests that treatment continuation after 6 months of targeted therapy might not need to rely solely on disease activity measurements, even when applying the T2T approach. Instead, shared decision-making, which takes into account patient-specific factors and preferences, may be more appropriate. However, further research is needed to clarify if continuing the current regimen is justified in patients who do not achieve LDA despite such considerations.
KEY MESSAGE
1. Among 456 patients with RA receiving targeted therapy, 213 (46.7%) continued with their initial treatment regimen despite not achieving LDA by week 24.
2. Among patients who did not achieve LDA by week 24, achieving LDA by week 48 was linked to fewer comorbidities, seronegativity for RA, greater reductions in DAS28-ESR and HAQ-DI from enrolment to week 24, and no NSAID use at week 24.
Notes
CRedit authorship contributions
Yeo-Jin Song: conceptualization, methodology, investigation, formal analysis, writing - original draft, visualization; Soo-Kyung Cho: conceptualization, methodology, investigation, data curation, writing - review & editing, visualization; Se Rim Choi: conceptualization, methodology, investigation, writing - review & editing, visualization, project administration; Shin-Seok Lee: conceptualization, methodology, investigation, data curation, writing - review & editing; Hye-Soon Lee: conceptualization, investigation, data curation, writing - review & editing; Sung-Hoon Park: conceptualization, investigation, data curation, writing - review & editing; Yeon-Ah Lee: conceptualization, investigation, data curation, writing - review & editing; Min-Chan Park: conceptualization, investigation, data curation, writing - review & editing; Hyoun-Ah Kim: conceptualization, methodology, data curation, writing - review & editing; Soo-Bin Lee: conceptualization, writing - review & editing, visualization, project administration; Ha-Rim Park: conceptualization, methodology, formal analysis, writing - review & editing; Eunwoo Nam: conceptualization, methodology, investigation, formal analysis, validation, software, writing - review & editing; Yoon-Kyoung Sung: conceptualization, methodology, resources, investigation, data curation, formal analysis, writing - original draft, writing - review & editing, supervision, project administration, funding acquisition
Conflicts of interest
H-S.L. received research grants from JW, Samsung Bioepis, and Lilly. M-C.P. received speaking fees from Eisai and AbbVie, and research grants from Eisai and Celltrion. Y-A.L. received speaking fees and/or honoraria from Eli Lilly, Astellas, AbbVie, and Johnson and Johnson, and research grants from Celltrion. Y-K.S. received speaking fees and/or honoraria from Eisai and consultant fees from Samsung Bioepis and Amjen. Other authors declare no conflict of interest.
Funding
This research was supported by a grant of Patient-Centered Clinical Research Coordinating Center (PACEN), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HC24C RS-2024-00399540).