A Case of Granular Cell Tumor of the Trachea
Article information
Abstract
A 20-year-old man presented to our outpatient clinic with hemoptysis, cough, and pleuritic chest pain. His chest radiograph and pulmonary function tests (PFT) were normal. A bronchoscopy showed a small yellowish patch with a regular surface. A direct bronchoscopic biopsy was performed. The pathologic findings showed a benign granular cell tumor. The respiratory symptoms resolved after biopsying the tumor. On follow.up, there were no signs of recurrence of the granular cell tumor after a period of 24 months.
INTRODUCTION
Granular cell tumors (GCTs) originate from Schwann cells. The majority of granular cell tumors occur in the head and neck region, with a predilection for occurrence in the tongue. Tracheal lesions are by far the least common. A confirmative diagnosis for GCTs should be made histopathologically and should be supported by immunohistochemical staining. The treatment of a granular cell tumor consists of wide local excision.
A review of the English language literature revealed 31 reported cases of tracheal granular cell tumors, with only four reported in children8). A review of the Korean ENT literature revealed several cases of laryngeal GCTs and one case of malignant GCT in the retrotracheal space1-3). There are no reports of tracheal GCT in the Korean literature
Here, we report a case of a 20.year.old man with tracheal GCT and discuss the diagnosis and management of this rare tumor.
CASE REPORT
A 20-year-old man presented to our clinic with blood.tinged sputum, cough, and left pleuritic pain of 2-weeks duration. The patient had a history of atrial fibrillation and epididymo-orchitis. He developed a small amount of blood-tinged sputum and left pleuritic pain, and had lost 4 kg of body weight in one month. Subsequently, the amount of blood-tinged sputum increased. No fever or chills were noted. The physical examination was unremarkable.
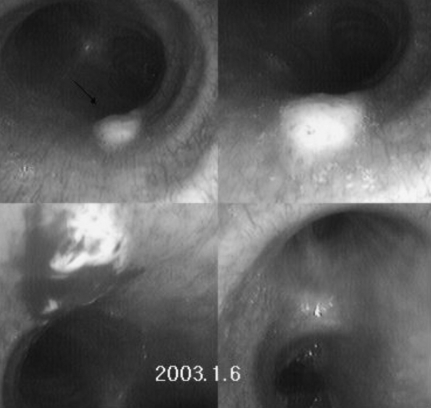
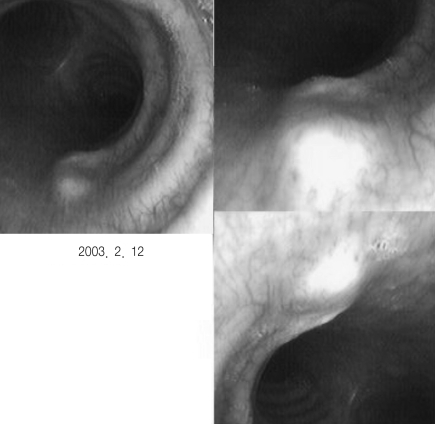
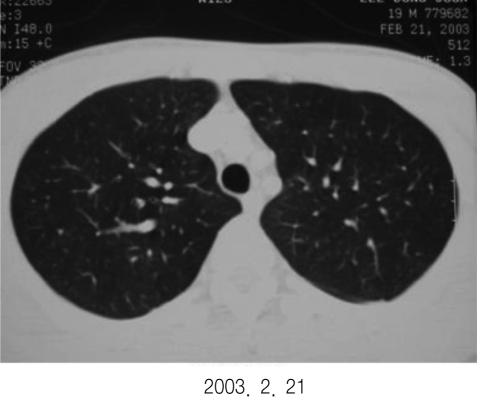
The workup of the patient included a complete blood count and blood chemistries, which were normal. A chest X-ray did not demonstrate any evidence of pulmonary disease (Figure 1). The patient underwent a pulmonary function test (PFT) and a bronchoscopy. The PFT showed a mild restrictive pattern: FVC, 4.1 (76%); FEV1, 3.2 (72%); and FEV1/FVC, 78%. A rigid bronchoscopy revealed a smooth, sessile, yellow lesion emanating from the right posterior terminal trachea wall (Figure 2). The lesion was biopsied, and the specimen was stained with hematoxylin and eosin. The sections showed a benign granular cell tumor with marked granular, eosinophilic cytoplasm and small, eccentric, round nuclei. An immunohistochemical analysis showed that the tumor cells were positive for neuron-specific enolase (NSE), s-100, and CD 68 (focally) (Figure 3).
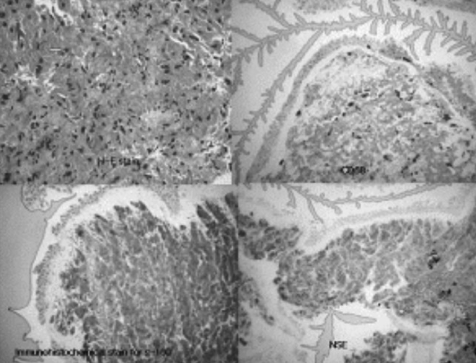
H&E staining reveal large cells with cytoplasmic granules. Immunohistochemical staining show tumor cells positive for NSE, S-100, and CD68.
A few days after admission to the clinic, the blood.tinged sputum resolved. The patient underwent a follow-up bronchoscopy one month later. The tracheal lesion had not changed (Figure 4). The biopsy specimen showed unremarkable columnar cells. A chest high-resolution computed tomography (HRCT) was normal (Figure 5).
The patient was discharged from the clinic as his hemoptysis and pleuritic pain had resolved. Two years after his initial presentation, the patient remains well.
DISCUSSION
Granular cell tumors, first reported by Abrikossoff in 1926, were initially called myoblastomas, suggesting a myogenic origin5). The histogenesis of this neoplasm remains controversial4). Currently, most pathologists believe that the cell of origin is the Schwann cell and refer to this lesion as a granular cell tumor4).
Ninety-eight percent of granular cell tumors are benign, and only 1 to 2% of all GCTs are malignant5). Although only 30 malignant lesions have been reported worldwide in the medical literature, none of these malignant lesions has been reported for the pediatric age group or in the trachea5).
More than 50% of granular cell lesions occur in the head and neck region, most commonly in the tongue. The reported rate of laryngeal GCTs is 10%. The larynx and bronchi are involved more often than the trachea. Other head and neck sites for GCTs include the central nervous system and cranial nerves, skin and subcutaneous tissues, middle and external ear, parotid glands, pharynx, palate, floor of the mouth, esophagus, and tonsils. About 10% of patients may have multiple GCTs at different anatomic sites.
A patient may remain completely asymptomatic with even 50 to 75% obstruction of the tracheal lumen. The average time from the onset of symptoms to patient presentation is 7 months. There is a history of progressive dyspnea unresponsive to bronchodilator and steroid therapy. Symptoms of wheezing, especially with exertion, are typically attributed to asthma and chronic bronchitis. There may be cough, hemoptysis, and a globus sensation, while pain is unusual6).
There are several ways to approach the initial management of tracheal tumors. Laryngoscopy and bronchoscopy can be performed to establish a safe airway, and to assess the extent of the lesion and perform a biopsy. Bronchoscopy allows examination of the tracheobronchial tree for other lesions.
A diagnosis can usually be made with hematoxylin-eosin staining, but immunohistochemistry with an S-100 protein stain and neuron.specific enolase are also helpful9). Histologically, the cells are monomorphic, often polygonal, with a granular cytoplasm. Pseudoepitheliomatous hyperplasia of the overlying epithelium can be confused with squamous cell carcinoma7).
An understanding of the differential diagnosis of subglottic and tracheal masses is important. Benign tracheal neoplasms may include a benign fibrous histiocytoma, papilloma, neurofibroma, pleomorphic adenoma, hemangioendothelioma, neurilemmoma, and benign chondrogenic tumors4). The differential diagnosis of malignant tracheal neoplasms includes a malignant fibrous histiocytoma, malignant chondrogenic neoplasia, carcinoid, rhabdomyosarcoma, fibrosarcoma, adenoid cystic carcinoma, and squamous cell carcinoma4). Neoplasms arising from the mediastinum, including esophageal tumors that erode the tracheal wall, should also be considered.
The treatment of a GCT is complete surgical excision. Neither radiation therapy nor chemotherapy has any role in the management of tracheal granular cell tumors. Bronchoscopic excision may be adequate for tumors less than 1 cm in diameter, whereas wide excision with tracheal resection is reserved for tumors with diameters greater than 1 cm. In one study, recurrence after excision occurred in approximately 8% of the cases, with all recurrence associated with the presence of a positive margin5).
Follow-up is based on appearance of symptoms rather than serial endoscopic examinations and imaging studies. Follow.up includes serial CT scans and endoscopic examinations.
GCTs are uncommon tumors with a predilection for the upper aerodigestive tract. Although respiratory symptoms caused by asthma or foreign bodies are common in children, the possibility of a tracheal tumor masquerading as recalcitrant asthma or recurrent pneumonia should not be overlooked. An unusual case of a mid.tracheal GCT presenting with obstructive sleep apnea and exercise.induced asthma illustrates this point. The diagnosis of a GCT and other tracheal masses depends on a high index of suspicion and an efficient workup. Treatment is complete surgical excision. This case outlines how a patient with tracheal GCT might present.