 |
 |
| Korean J Intern Med > Volume 25(2); 2010 > Article |
|
Abstract
Background/Aims
Metabolic syndrome is an emerging risk factor for cardiovascular disease. This study investigated the prevalence of metabolic syndrome among psychiatric patients in order to identify the dominant factors of metabolic syndrome.
Methods
We enrolled 225 patients who had been admitted to a chronic psychiatric hospital from October 2005 to February 2006. The prevalence of metabolic syndrome was assessed based on the Adult Treatment Panel (ATP)-III with the new criterion of waist circumference in the Asia-Pacific Region.
Results
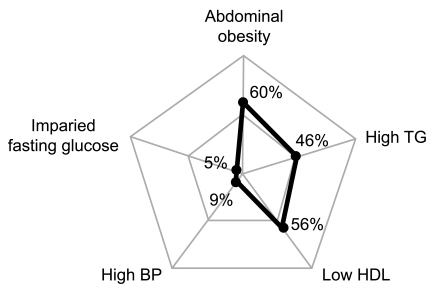
The study population was relatively young (41.1 ┬▒ 8.8 years) and obese (waist in men, 91.3 ┬▒ 9.2 cm; waist in women, 84.1 ┬▒ 8.8 cm). Sixty percent of patients met the waist criterion of metabolic syndrome and 56% met the low high density lipoprotein (HDL) criterion. The mean serum triglycerides were high (170.0 ┬▒ 119.7 mg/dL) and 46% of patients met the triglyceride criterion. In contrast, less than 10% of patients showed impaired fasting glucose or high blood pressure (5%, 9%, respectively). The overall prevalence of metabolic syndrome was 34.2% by applying ATP-III criteria (40% in men and 20% in women, respectively). No specific anti-psychotic drugs were related to significant increase in the incidence of metabolic syndrome.
Conclusions
Abdominal obesity and dyslipidemia (low HDL and high triglycerides) were dominant contributing factors of metabolic syndrome among psychiatric patients, and the affected age groups were relatively young. These findings indicate that active and early screening, including triglycerides, HDL, and waist measurement, are absolutely essential to managing metabolic syndrome in psychiatric patients.
The prevalence of metabolic syndrome has increased among general populations due to the increasing tendency of less physical activity, high caloric diet and resultant obesity. Such metabolic issues are also of importance for psychiatric patients. Metabolic syndrome is a composition of several metabolic derangements that originate from insulin resistance [1]. It is well known that metabolic syndrome increases cardiovascular morbidity and mortality. Medical conditions in psychiatric patients are often underestimated, which can lead psychiatric patients to be more susceptible to medical morbidity [2]. In fact, cardiovascular disease is one of the most important medical conditions among psychiatric patients [3]. There are several explanations as to why psychiatric patients are susceptible to cardiovascular disease. An inactive lifestyle and poor dietary choices make psychiatric patients obese, and the side effects of antipsychotic agents have received attention [4-6]. Several reports on the prevalence of metabolic syndrome among psychiatric patients have been published [7-11]. However, there is little information on non-caucasian patients or on the characteristics of their metabolic syndrome. We therefore investigated the metabolic profiles that contribute to the development of metabolic syndrome in Korean patients.
We identified 249 consecutive patients who had been admitted to a chronic psychiatric hospital from October 2005 to February 2006. Basic physical measurements, such as weight, height and abdominal circumference were checked in all patients upon admission. Routine medical tests were also performed, such as complete blood cell count, chemistry, urinalysis, chest X-ray, and electrocardiogram. We included 225 patients diagnosed as having psychiatric disease, and who were on antipsychotic agents, and conducted examinations for metabolic syndrome components. The Institutional Review Board of the National Cancer Center of Korea approved this study. Written informed consent was not required for this retrospective study.
The prevalence of metabolic syndrome was assessed based on the Adult Treatment Panel (ATP)-III. In addition, we used the new criterion of waist circumference in the Asia-Pacific Region instead of the original one [12]. The modified definition required more than three of the following: 1) increased waist circumference (> 90 cm in men and > 80 cm in women), 2) high triglycerides (Ōēź 150 mg/dL), 3) low high density lipoprotein (HDL) cholesterol (< 40 mg/dL in men and < 50 mg/dL in women), 4) high blood pressure (Ōēź 130 / 85 mmHg or currently on antihypertensive medication), and 5) high fasting glucose (Ōēź 110 mg/dL or currently on antidiabetic medication). Serum total cholesterol, HDL cholesterol and triglycerides were measured by enzymatic colorimetric assay using an autoanalyzer (Hitachi 7600, Hitachi Ltd., Tokyo, Japan). Means and standard deviations were used to present continuous variables, and frequency counts were used to present categorical variables. Any drugs taken for longer than three months were also investigated. Each patient group of antipsychotic agents was compared on the basis of metabolic syndrome prevalence. Similarly, the associations between categorical parameters were assessed using the chi-square test or Fisher's exact test. Continuous variables were presented as the mean ┬▒ standard deviation and were compared by student t test. Statistical significance was accepted at a two-tailed p < 0.05. Stata/SE for Windows (Stata Corp., College Station, TX, USA) was used for analysis.
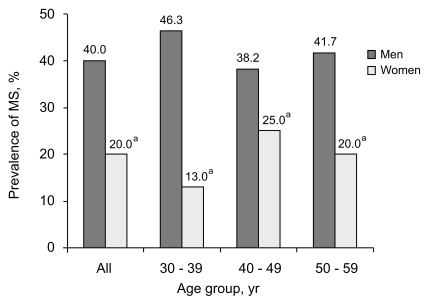
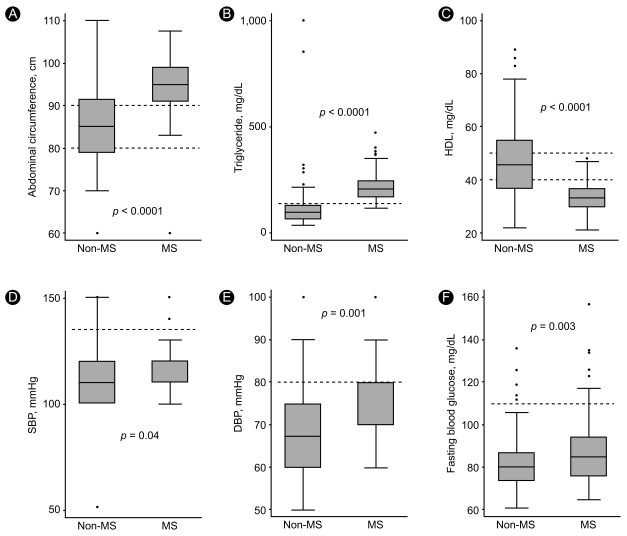
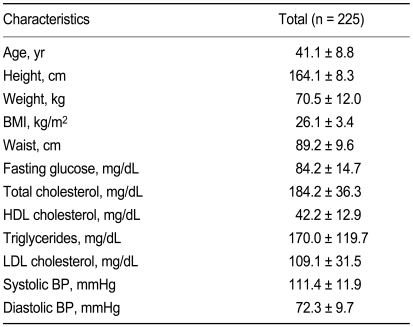
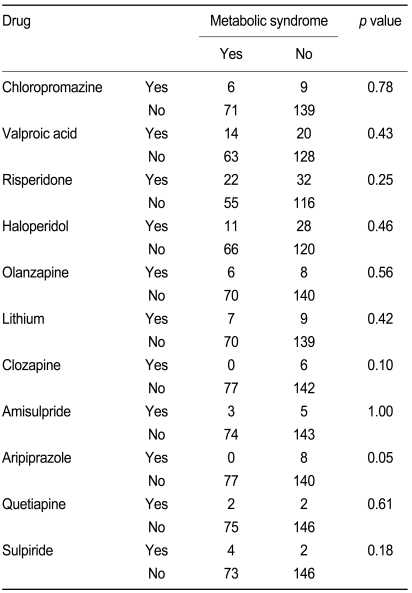
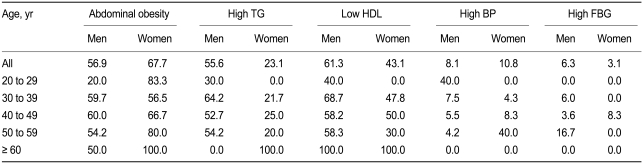
The clinical and metabolic characteristics of the subjects are given in Table 1. The mean age of the subjects was 41.4 years. The patients were relatively young compared to the mean age of those in a previous study that investigated metabolic syndrome in the same ethnic general population [13]. The subjects were obese, according to waist circumference (91.3 ┬▒ 9.1 cm in men, 84.1 ┬▒ 8.8 cm in women), weight (70.5 ┬▒ 12.0 kg), and body mass index (BMI) (26.1 ┬▒ 3.4 kg/m2). Their triglyceride levels were high (170.0 ┬▒ 119.7 mg/dL). The prevalence of diabetes and hypertension was 8.4% and 4.4%, respectively. Psychiatric diagnoses varied and schizophrenia was dominant: schizophrenia 72.0%, depression 12.9%, delusional disorder 6.7%, compulsive disorder 3.1%, personality disorder with psychotic feature 2.7%, bipolar disorder 2.7%. Overall, the distribution of antipsychotic agents taken for longer than three months was risperidone 45%, haloperidol 32.5%, chloropromazine 12.5%, olanzapine 11.7%, amisulpiride 6.7%, aripiprazole 6.7%, and clozapine 5%. More than half of the patients had been taking the same antipsychotic drugs during the last six months as a characteristic of chronic hospitalization. There were no significant differences between each group's prevalence of metabolic syndrome with Fisher's exact test (Table 2). The overall prevalence of metabolic syndrome was 34.2%. The men were more susceptible to metabolic syndrome than women (40% vs. 20%, respectively). The prevalence of metabolic syndrome in young men was much higher than the prevalence reported previously for the general population, and it was also higher than the prevalence in an older group in the Korean population (Fig. 1) [13]. The high prevalence of metabolic syndrome may be attributed to abdominal obesity and dyslipidemia characterized by high triglycerides and low HDL cholesterol (Table 3). More than half of all subjects met the criterion of abdominal obesity (60.0%) and dyslipidemia (46.2% of patients had high triglycerides and 56.0% had low HDL cholesterol). In contrast, the prevalence of high blood pressure and impaired fasting glucose in the overall population were relatively low (8.9% and 5.3%, respectively). The prevalence of each metabolic syndrome component is depicted in Fig. 2. To clarify the factors contributing to metabolic syndrome, we compared each component of metabolic syndrome between subjects who met the criterion with those who did not. Greater abdominal obesity, higher triglycerides, and lower HDL cholesterol were prominent in the metabolic syndrome group (Fig. 3). The difference in mean low density lipoprotein (LDL) cholesterol levels was not statistically significant.
Psychiatric patients showed a high prevalence of metabolic syndrome because of their high vulnerability to abdominal obesity and dyslipidemia (high triglycerides and low HDL cholesterol) as opposed to high blood pressure and impaired fasting glucose (Fig. 2). A plausible explanation is that metabolic derangement caused by physical inactivity or adverse effects of drugs may have affected abnormal fat distribution or impaired lipid metabolism rather than elevating blood pressure or increasing insulin resistance. These characteristics in psychiatric patients are different from those of other Asian populations, in which high blood pressure and abdominal obesity were dominant contributing factors to metabolic syndrome [14]. Furthermore, this unique combination of components leading to metabolic syndrome has not been observed among the general Korean population [13]. In addition, the underestimation of metabolic syndrome is problematic, considering that only total cholesterol, fasting blood glucose, blood pressure, and weight are checked in usual practice. The screening of waist circumference and the whole lipid profile, including triglycerides and HDL cholesterol, could be helpful in detecting metabolic syndrome among psychiatric patients. Furthermore, the prevalence of metabolic syndrome in younger people was not lower than that in older people (Fig. 1). This means that they are exposed to complications of metabolic syndrome, such as cardiovascular disease, over their lifetime. Therefore, careful attention should be paid to metabolic disturbances of psychiatric patients.
Our study has some limitations. There may be insufficient statistical power, due to the small sample size. In addition, the study was performed retrospectively, so it was limited in its ability to confirm the exact prevalence of metabolic syndrome. However, the present study was conducted in hospitalized patients at a chronic hospital and the patients had been hospitalized, on average, for more than 18 months; thus, their lifestyles were relatively uniform and much more regular and controlled than those of outpatients. Lifestyle, including physical activity and diet, are important compounding factors in the study of metabolic syndrome. Such a controlled lifestyle in our study population is a strong point. In spite of the controlled lifestyle, the prevalence of metabolic syndrome was high, so it can be speculated that general psychiatric outpatients are more vulnerable to metabolic syndrome than the present population, and that more active screening and management should be added to lifestyle modification.
In conclusion, we found unique characteristics of metabolic syndrome among psychiatric patients. Specifically, abdominal obesity and dyslipidemia, i.e., low HDL cholesterol and high triglycerides, are dominant contributing factors. In addition, the affected ages are younger. These findings suggest that active and early screening, including triglycerides, HDL cholesterol, and waist measurement, are absolutely essential to managing metabolic syndrome among psychiatric patients.
Acknowledgements
We express our gratitude to members of the laboratory and the nursing staff at the Institute of Forensic Psychiatry for their excellent technical assistance.
References
1. Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 1988;37:1595ŌĆō1607PMID : 3056758.


2. Allebeck P. Schizophrenia: a life-shortening disease. Schizophr Bull 1989;15:81ŌĆō89PMID : 2717890.


3. Osby U, Correia N, Brandt L, Ekbom A, Sparen P. Mortality and causes of death in schizophrenia in Stockholm county, Sweden. Schizophr Res 2000;45:21ŌĆō28PMID : 10978869.


4. Meyer JM. Effects of atypical antipsychotics on weight and serum lipid levels. J Clin Psychiatry 2001;62(Suppl 27):27ŌĆō34PMID : 11806486.
5. Shirzadi AA, Ghaemi SN. Side effects of atypical antipsychotics: extrapyramidal symptoms and the metabolic syndrome. Harv Rev Psychiatry 2006;14:152ŌĆō164PMID : 16787887.


6. Wu RR, Zhao JP, Liu ZN, et al. Effects of typical and atypical antipsychotics on glucose-insulin homeostasis and lipid metabolism in first-episode schizophrenia. Psychopharmacology (Berl) 2006;186:572ŌĆō578PMID : 16601995.


7. Basu R, Brar JS, Chengappa KN, et al. The prevalence of the metabolic syndrome in patients with schizoaffective disorder: bipolar subtype. Bipolar Disord 2004;6:314ŌĆō318PMID : 15225149.


8. Cohn T, Prud'homme D, Streiner D, Kameh H, Remington G. Characterizing coronary heart disease risk in chronic schizophrenia: high prevalence of the metabolic syndrome. Can J Psychiatry 2004;49:753ŌĆō760PMID : 15633853.


9. De Hert MA, van Winkel R, Van Eyck D, et al. Prevalence of the metabolic syndrome in patients with schizophrenia treated with antipsychotic medication. Schizophr Res 2006;83:87ŌĆō93PMID : 16481149.


10. Heiskanen T, Niskanen L, Lyytik├żinen R, Saarinen PI, Hintikka J. Metabolic syndrome in patients with schizophrenia. J Clin Psychiatry 2003;64:575ŌĆō579PMID : 12755662.


11. McEvoy JP, Meyer JM, Goff DC, et al. Prevalence of the metabolic syndrome in patients with schizophrenia: baseline results from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial and comparison with national estimates from NHANES III. Schizophr Res 2005;80:19ŌĆō32PMID : 16137860.


12. Inoue S, Zimmet P, Caterson I, et al. The Asia-Pacifia perspective: redefining obesity and its treatment. Crows Nest: Health Communications Australia Pty Limited on behalf of the Steering Committee. 2000.
Figure┬Ā1
Age-specific prevalence of metabolic syndrome (MS) from 30 to 59 by sex. Data for ages 20 to 29 and over 60 are not shown due to low values (less than 10). ap < 0.05 between men and women.
Figure┬Ā2
Prevalence of each metabolic syndrome component. Values are presented as the percentage of subjects who met each criterion. TG, triglycerides; HDL, high density lipoprotein; BP, blood pressure.
Figure┬Ā3
Box plots presenting the distribution of each component of metabolic syndrome. The median of each component is represented by the horizontal line in the middle of each box. Each box represents the 25 to 75 percent quartiles. The ends of the vertical lines indicate the minimum and maximum data values except outliers, which are represented as dots outside the line. Abdominal obesity (A), high triglycerides (B), and low HDL (C) are more prominent than other components (D, E, and F) among the metabolic syndrome group. MS, metabolic syndrome group; Non-MS, no metabolic syndrome group; HDL, high density lipoprotein; SBP, systolic blood pressure; DBP, diastolic blood pressure.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



