 |
 |
| Korean J Intern Med > Volume 28(3); 2013 > Article |
|
Abstract
Hemorrhagic fever with renal syndrome (HFRS) is an acute viral disease characterized by fever, hemorrhage, and renal failure. Among the various hemorrhagic complications of HFRS, the spontaneous rupture of an arteriovenous malformation of the testicular vessels with a retroperitoneal hematoma is a rare finding. Here, we report a case of HFRS complicated by a massive retroperitoneal hematoma that was treated with transcatheter arterial embolization.
Hemorrhagic fever with renal syndrome (HFRS) is an acute infectious disease caused by Hantaan virus and is clinically characterized by fever, renal failure, and hemorrhage in organs such as the lung, kidney, spleen, brain, and pituitary gland [1]. The hemorrhage in HFRS varies from transient petechial lesions to fulminant and massive bleeding. Most of the hemorrhagic manifestations occur from the febrile stage to the oliguric stage, and rarely in the convalescent stage. Renal medullary hemorrhage is a well-documented complication in HFRS [2], but the spontaneous rupture of a kidney or retroperitoneal hematoma is rare [3,4]. We report a case of HFRS complicated by the spontaneous rupture of an arteriovenous malformation (AVM) of the testicular vessels at the inferior portion of the right kidney and a retroperitoneal hematoma that was treated by transcatheter arterial embolization.
A 43-year-old man visited the emergency department because of nausea, vomiting, diarrhea, and epigastric pain lasting 2 days. He had suffered from a fever, chills, and headache for 4 days prior to admission. He had no other medical problems, no history of drug use, and no family history of disease. His was employed as a lawn caretaker at a ski resort in Gyeonggi-do.
His vital signs upon admission were as follows: blood pressure, 130/90 mmHg; heart rate, 72 beats per minute; respiratory rate, 18 breaths per minute; and body temperature, 36.3Ōäā. A physical examination revealed increased bowel sounds and tenderness in the upper abdomen and at both costovertebral angles. Initial laboratory testing showed a white blood cell count of 18,550/mm3, a hemoglobin level of 17 g/dL, a platelet count of 32,000/mm3, and a serum creatinine level of 5.92 mg/dL. The prothrombin time and activated partial thromboplastin time were normal. His urinalysis showed proteinuria and microscopic hematuria.
On the second day of hospitalization, he became oliguric and started hemodialysis. One day later, he began to complain of severe right lower abdominal pain accompanied by abdominal rigidity. He subsequently became hemodynamically unstable and delirious. He was moved to an intensive care unit for close observation. Hemoglobin measurements were at 8.5 g/dL on the third day of hospitalization and further declined to 3 g/dL, resulting in continued thrombocytopenia. Thus, he received a transfusion of three units of packed red blood cells and eight pints of platelet concentrates.
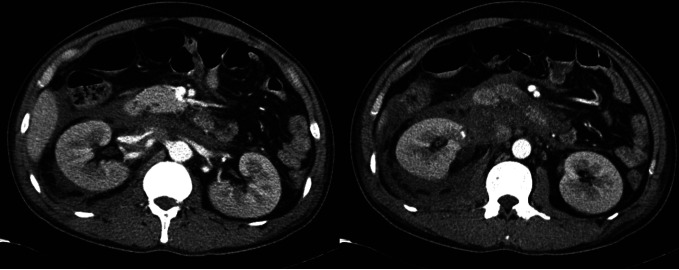
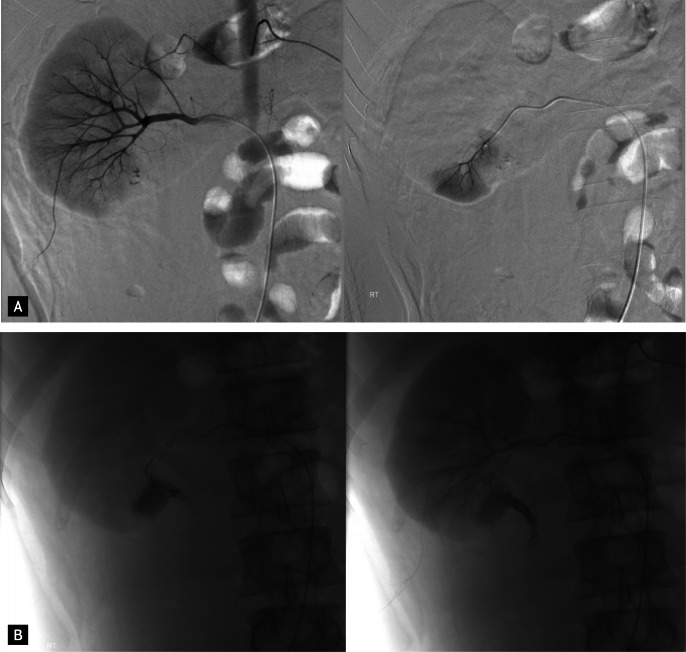
Emergency contrast-enhanced computed tomography of the abdomen and pelvis showed a huge retroperitoneal hematoma below the right kidney with surrounding complicated fluid collection, and right hydroureteronephrosis (Fig. 1). Renal arteriography was performed as well as selective right renal arteriography, which showed extravasation of the contrast medium from an AVM of the testicular vessels at the inferior portion of the right kidney (Fig. 2A). Transcatheter embolization was performed at the ruptured small branches (Fig. 2B). After embolization, renal arteriography confirmed that there was no more extravasation of the contrast medium. The antibody titer of Hantaan virus was greater than 1 : 1,280, and the patient was confirmed to have HFRS with retroperitoneal hematoma.
Urination gradually increased to 2,600 mL/day, and serum creatinine decreased to 1.34 mg/dL. Therefore, hemodialysis was halted on day 6 of hospitalization. On day 9, a follow-up computed tomography scan of the abdomen and pelvis showed that the extent of the retroperitoneal hematoma and the amount of surrounding fluid collection had decreased. The patient was discharged from the hospital after recovery, on day 19.
HFRS is a rodent-transmitted disease caused by a Hantavirus. Hantavirus infection is acquired by inhalation of aerosolized virus-containing particles or by contact with the urine, secretions, or feces of infected rodents. Classic HFRS has several prominent features, including fever, hemorrhage, hypotension, and renal failure [1,5]. However, the clinical course can be extremely variable, from asymptomatic to severe, depending on the strain of Hantavirus infection.
Increased vascular permeability appears to play a general role in the pathogenesis of Hantavirus infection. This is suggested clinically by an increase in the hematocrit and a decrease in the serum protein levels. Tracer studies have confirmed the presence of generalized vascular leaks [5]. This phenomenon can explain the bleeding tendency, retroperitoneal edema, and pulmonary edema seen in Hantavirus infections.
The mechanism of the bleeding tendency in HFRS is associated with thrombocytopenia, abnormal platelet function, vascular damage, and disseminated intravascular coagulation [4]. The cause of thrombocytopenia is not related to reduced platelet production, but rather to increased platelet consumption owing to shortened platelet survival, increased megakaryocytes in the bone marrow, and circulating giant platelets in the peripheral blood [6]. Thrombocytopenia appears at the febrile phase, worsens during the oliguric phase, and may recover by the diuretic phase. The abnormal adhesion and aggregation of platelets are thought to be associated with uremia and fibrin degradation products, which also appear at the febrile phase, worsen during the oliguric phase, and may recover by the diuretic phase. Vascular damage is due directly to the virus itself; secondary causes are adherence of circulating immune complexes to vessel walls, hypoxia, and acidemia. Findings of coagulopathy in most documented cases had normalized within 10 days of the illness. Therefore, disseminated intravascular coagulation and thrombocytopenia in the early phase, and azotemia developing later may be important in the pathogenesis of the bleeding tendency in HFRS [6].
The most common manifestation of hemorrhage is petechiae involving the skin and oropharyngeal mucosa. Hemorrhage occasionally occurs spontaneously or via minor trauma in vital organs such as the lung, kidney, spleen, brain, and pituitary gland [4,7]. The prevalence of spontaneous retroperitoneal hemorrhage in HFRS is 0.48% in Korea [3] and 0.6% in China [4]. Several cases of perirenal hemorrhage with retroperitoneal hematoma in HFRS have been reported in Korea. One case that showed active extravasation of contrast medium on selective renal arteriography was treated by renal artery embolization [8]. The present case also showed active extravasation of contrast medium on renal arteriography, and we ascertained that the cause of bleeding was a spontaneously ruptured testicular AVM, unlike the case mentioned above [8].
The treatment of spontaneous renal bleeding and retroperitoneal hematoma is decided according to the cause of the bleeding. Well-known causes are renal cell carcinoma; angiomyolipoma; vascular conditions such as renal infarction, aneurysm, and AVM; and miscellaneous causes, including HFRS and hemorrhagic cyst or abscess. When the cause is indefinite, the bleeding or hematoma has often been treated with surgery because of the probability of malignancy. In HFRS cases, the indications for surgery are progressive anemia, palpable retroperitoneal hematoma, and symptomatic peritoneal irritation [9]. However, when the cause of bleeding is a vascular abnormality, angiography is useful for the diagnosis and treatment by endovascular therapy with embolization [10]. One previously reported case in Korea was treated with renal artery embolization [8], but most have been treated with conservative management. In the present case, we performed renal arteriography to confirm the testicular AVM and transcatheter superselective testicular artery embolization, rather than surgery, to treat the bleeding and perirenal hematoma.
In summary, retroperitoneal hematoma caused by a ruptured testicular AVM is a rare complication of HFRS. In cases of vascular abnormalities, angiography is useful for diagnosis as well as treatment. We must consider a vascular lesion as a cause for retroperitoneal hematoma in HFRS.
References
1. Lee JS. Clinical features of hemorrhagic fever with renal syndrome in Korea. Kidney Int Suppl 1991;35:S88ŌĆōS93PMID : 1685206.

2. Kim SH, Kim S, Lee JS, et al. Hemorrhagic fever with renal syndrome: MR imaging of the kidney. Radiology 1990;175:823ŌĆō825PMID : 1971450.


3. Cho BY, Koh CS, Lee MH. A clinical observations of complications in Korean hemorrhagic fever. Korean J Intern Med 1979;22:22ŌĆō30.
4. Guang MY, Liu GZ, Cosgriff TM. Hemorrhage in hemorrhagic fever with renal syndrome in China. Rev Infect Dis 1989;11(Suppl 4):S884ŌĆōS890PMID : 2568678.


5. Cosgriff TM, Lewis RM. Mechanisms of disease in hemorrhagic fever with renal syndrome. Kidney Int Suppl 1991;35:S72ŌĆōS79PMID : 1685203.

6. Lee M. Coagulopathy in patients with hemorrhagic fever with renal syndrome. J Korean Med Sci 1987;2:201ŌĆō211PMID : 3151765.



7. Peters CJ, Simpson GL, Levy H. Spectrum of hantavirus infection: hemorrhagic fever with renal syndrome and hantavirus pulmonary syndrome. Annu Rev Med 1999;50:531ŌĆō545PMID : 10073292.


8. Choi HS, Lee YS, Hwang JC, Lim JH, Kim KS, Yoon Y. Renal artery embolization of perirenal hematoma in hemorrhagic fever with renal syndrome: a case report. Korean J Radiol 2007;8:348ŌĆō350PMID : 17673847.



9. Valiakhmetov RZ, Gafarov AI, Memkhes VS, Galimzianov VZ. Spontaneous rupture of the kidneys in hemorrhagic fever with renal syndrome. Urol Nefrol (Mosk) 1990;50ŌĆō53PMID : 1982474.
Figure┬Ā1
Contrast-enhanced computed tomography scan of the abdomen and pelvis showed a retroperitoneal hematoma below the right kidney with surrounding complicated fluid collection, and right hydroureteronephrosis.
Figure┬Ā2
Renal angiography of the case. (A) Renal arteriography and selective right renal arteriography showed extravasation of the contrast medium from an arteriovenous malformation of the testicular vessels at the inferior portion of the right kidney. (B) Transcatheter embolization was performed at the ruptured right testicular arteriovenous malformation



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



