To the Editor,
Breast cancer is not a single disease entity but rather a heterogeneous disease with various biological behaviors. Breast cancer subtypes can be identified by gene or protein expression profiling using immunohistochemistry (IHC). The expression patterns of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) as detected by IHC are important factors in determining treatment modalities such as hormone therapy, HER2-targeted therapy, and cytotoxic chemotherapy. In recent years, discordance in ER, PR, and HER2 statuses between primary and recurrent breast cancer has been reported, but the discordance rate varies highly. Generally, a change from positive to negative status for ER and PR is more common than a gain of receptor expression, and more patients gain rather than lose HER2 expression [1,2]. Here, we report the unusual case of a patient who was diagnosed initially with triple-negative breast cancer (TNBC) but whose cancer progressed as ER-positive diffuse skin metastases after a short time.
A 38-year-old female visited our hospital with a palpable right breast mass in July of 2011. Breast magnetic resonance imaging (MRI) showed a nodular mass with a diameter of 4.0 cm in the upper outer quadrant of the right breast and multiple enlarged lymph nodes in the right axillary region. A core needle biopsy of the breast mass was performed. Pathological examination revealed a poorly differentiated invasive ductal carcinoma, which was negative for ER, PR, and HER2. F-18 fluorodeoxyglucose (FDG) positron emission tomography (PET)-computed tomography (CT) also showed a nodular mass and multiple lymph nodes with high FDG uptake (maximum standardized uptake value [SUVmax] 4.7) in the right breast and axillary region. There was no evidence of any other distant metastases. On the basis of these results, the patient was diagnosed with TNBC (cT2N3M0) and received three cycles of neoadjuvant chemotherapy with docetaxel and epirubicin. After the three cycles of chemotherapy, a partial response was confirmed by a breast CT scan, and the patient underwent a modified radical mastectomy in November of 2011. Histopathological examination revealed an invasive ductal carcinoma with necrosis and 11 metastatic lymph nodes among the 11 dissected axillary lymph nodes. We found lymphovascular invasion and tumor emboli in dermal lymphatic vessels combined with skin invasion. Immunohistochemical analyses showed negative staining for ER, PR, and HER2. The patient received an additional three cycles of adjuvant chemotherapy with docetaxel and epirubicin, and adjuvant radiotherapy of the right chest wall and regional lymphatics.
In September of 2012, a surveillance PET-CT scan showed multiple enlarged lymph nodes with high FDG uptake (SUVmax 6.0) in the left supraclavicular, cervical, and internal mammary lymph nodes, and small nodular lesions with focal FDG uptake (SUVmax 1.9) in the right upper lung and left lower lung fields. A chest CT scan also showed a few tiny peripheral nodules in the right upper lung and left lower lung fields. On physical examination, there were several palpable masses in the left neck. An ultrasound-guided core needle biopsy of the cervical lymph node was performed, and pathological examination revealed an invasive ductal carcinoma. The expression of ER, PR, and HER2 was concordant with the prior right breast cancer, which was negative for ER, PR, and HER2. Subsequently, the patient received six cycles of palliative chemotherapy with docetaxel and cisplatin until January 2013. A follow-up PET-CT scan and chest CT scan showed a near-complete radiological response in the previous multiple metastatic lymph nodes and tiny lung lesions, and there was no evidence of active lesions with abnormal FDG uptake. Therefore, we planned to stop the chemotherapy and to follow up with the patient regularly.
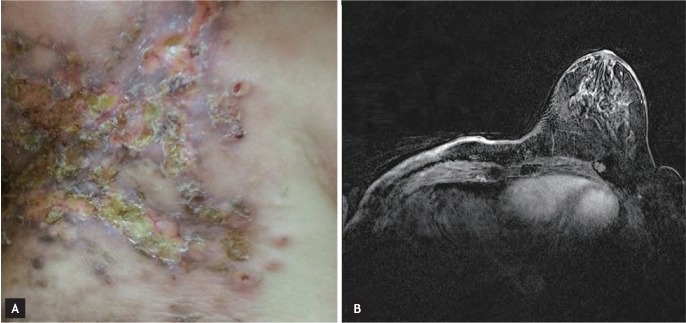
Two months later, the patient complained of multiple reddish nodules on her right chest wall, shoulder, and upper arm (Fig. 1A). Breast MRI showed skin enhancement of the right chest wall with an even thickness, and postoperative or postradiation skin changes were suspected (Fig. 1B). A skin biopsy was performed, and the slides were independently reviewed by two pathologists. ER and PR expression was scored using the semiquantitative Allred system, which takes into account the proportion of positive cells (graded from 0 to 5) and the staining intensity (graded from 0 to 3). Pathological examination showed an invasive ductal carcinoma with diffuse lymphatic invasion (Fig. 2A) that was positive for ER (intensity score, 3; proportion score, 3) and negative for PR and HER2 (Fig. 2B). A PET-CT scan showed heterogeneous hypermetabolic activity of the skin throughout the right chest wall and small hypermetabolic nodular lesions in the parasternal area, but there were no other visceral metastases. The patient, who was premenopausal, was administered hormone therapy comprised of a gonadotropin-releasing hormone agonist and tamoxifen (20 mg daily). After three cycles of hormone therapy, follow-up breast MRI showed stable disease for the skin enhancement of the right chest wall.
TNBC is defined as a tumor that does not express ER, PR, or HER2; it accounts for 15% to 20% of all breast cancers. TNBC is clearly a distinct clinical subtype but a heterogeneous subgroup with diversity in both tumor biology and prognosis [3]. Over the last decade, the following characteristics of TNBC have been identified: younger patient age, BRCA1-associated cancer, higher incidence of brain metastasis, platinum sensitivity, and poor prognosis [3]. Although the metastatic potential of TNBC is similar to that of other breast cancer subtypes, TNBC is more likely to cause early visceral metastases and is associated with a shorter median time to relapse and death [3]. Our patient experienced relapse with multiple metastases in the cervical lymph nodes and lung within 14 months after diagnosis. She achieved a near-complete radiological response to docetaxel and cisplatin chemotherapy but experienced progression as skin metastases only 2 months after the termination of chemotherapy.
Skin metastases from visceral malignancies are uncommon; the reported incidence ranges from 0.7% to 9% [4]. Breast cancer is the most common cancer to metastasize to the skin, followed by lung, melanoma, colon, kidney, and ovarian malignancies. Few studies have investigated the patterns or characteristics of skin metastases in patients with TNBC. Kong et al. [5] evaluated whether the patterns of skin metastases differ according to breast cancer subtype. A retrospective analysis of 125 patients with skin metastases from breast cancer showed that such metastases were more common in hormone receptor-positive breast cancer than in TNBC (42.4% vs. 23.2%, respectively), and that erythematous infiltrations were more frequent in TNBC patients. Our patient presented with ulcerative nodular skin lesions combined with erythematous infiltration in the operation bed, and a change in subtype from TNBC to ER-positive breast cancer was found.
Growing evidence of discordance in ER, PR, and HER2 expression between primary and recurrent breast cancer has been reported. The discordance rate varies between studies and can be as high as 40%. The switch to a different tumor phenotype leads to a change in treatment for approximately 20% of cases [1]. According to previous studies, a change from a positive to negative (receptor loss) status is more common than a change from a negative to positive (receptor gain) status. A loss of PR expression is the most frequent change, and changes in ER, PR, and HER2 expression in primary TNBC are relatively rare. Heitz et al. [1] reported that 44 (80.0%) of 55 patients with primary TNBC experienced recurrence of the same triple-negative phenotype, and that only two patients (3.6%) became positive for ER and negative for HER2.
The mechanisms responsible for changes in biomarker expression between primary and recurrent breast cancer are not clearly understood, but several possibilities have been proposed, including methodological and technical errors, intratumoral heterogeneity, clonal selection caused by previous treatment, and a switch in tumor biology during progression [1,2]. In our case, we initially confirmed the negativity of the tumor for ER, PR, and HER2 and skin invasion combined with tumor emboli within dermal lymphatic channels in the primary breast cancer obtained from a surgical specimen. Considering that skin metastases occurred in the operation bed and that dermal lymphatic invasion was observed in both primary and recurrent tumor tissues, it is likely that the remaining tumor cells in the lymphatic system had progressed and spread out along the skin. This suggests a change in tumor biology during disease progression or intratumoral heterogeneity in ER expression in the primary breast tumor. Subpopulations of cancer cells in the same patient may exist across different geographical regions of a tumor or evolve over time, which is known as intratumoral heterogeneity. Another lesson from our case is that these biomarkers can change even with a short time to progression. Further study is needed to identify the mechanisms responsible for receptor gain in TNBC, the prognostic impact of a change in tumor phenotype, and the optimal therapeutic strategies.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





