Synchronous second primary cancers in patients with squamous esophageal cancer: clinical features and survival outcome
Article information
Abstract
Background/Aims:
Unexpected diagnosis of synchronous second primary cancers (SPC) complicates physicians’ decision-making because clinical details of squamous esophageal cancer (EC) patients with SPC have been limited. We evaluated clinical features and treatment outcomes of patients with synchronous SPC detected during the initial staging of squamous EC.
Methods:
We identified a total of 317 consecutive patients diagnosed with squamous EC. Relevant clinical and cancer-specific information were reviewed retrospectively.
Results:
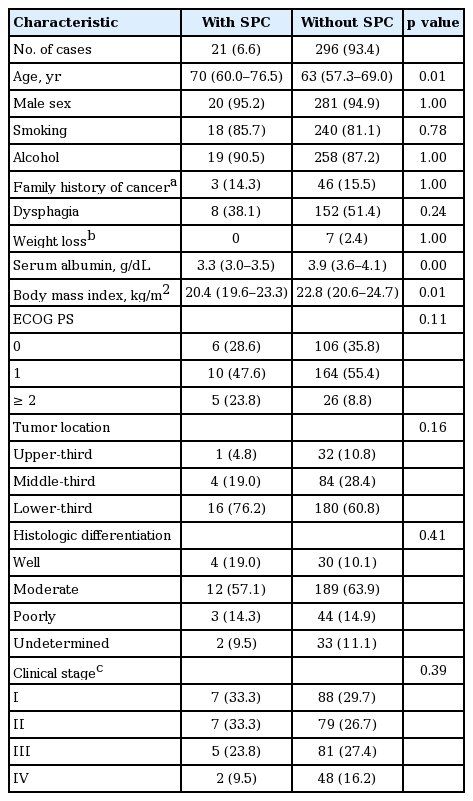
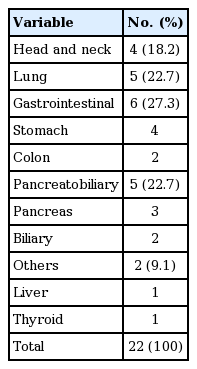
EC patients with synchronous SPC were identified in 21 patients (6.6%). There were significant differences in median age (70 years vs. 63 years, p = 0.01), serum albumin level (3.3 g/dL vs. 3.9 g/dL, p < 0.01) and body mass index (20.4 kg/m2 vs. 22.8 kg/m2, p = 0.01) between EC patients with and without SPC. Head and neck, lung and gastric cancers accounted for 18.2%, 22.7%, and 18.2% of SPC, respectively. Positron emission tomography-computed tomography (PET-CT) detected four cases (18.2%) of SPC that were missed on CT. Management plans were altered in 13 of 21 patients (61.9%) with detected SPC. Curative esophagectomy was attempted in 28.6% of EC patients with SPC (vs. 59.1% of patients without SPC; p = 0.006). EC patients with SPC had significantly lower 5-year survival than patients without SPC (10.6% vs. 36.7%, p = 0.008).
Conclusions:
Synchronous SPC were found in 6.6% of squamous EC patients, and PET-CT contributed substantially to the detection of synchronous SPC. EC patients with SPC had poor survival due to challenges of providing stage-appropriate treatment.
INTRODUCTION
The incidence of synchronous second primary cancers (SPC) in patients with squamous esophageal cancer (EC) is reported to be 5% to 10% [1-4]. The most well known SPC are head and neck and lung cancers. The association between SPCs and these cancers can be explained by a process called ‘field cancerization,’ which arises from exposure to common carcinogenic agents such as tobacco smoke [5,6]. Accurate detection of synchronous SPC should be of particular concern for patients with EC because survival of these patients has increased significantly due to advances in multimodality therapies and surgical procedures. However, data on the incidence and distribution of synchronous SPC in squamous EC patients are limited in Korea.
Positron emission tomography (PET) is a widely used diagnostic modality for a variety of malignancies. The addition of computed tomography (CT) further improves anatomic interpretation. Although PET-CT increases the detection of synchronous SPC in patients with other malignancies, the potential contribution of PET-CT has not been evaluated in patients with squamous EC [7-10].
The unexpected diagnosis of synchronous SPC complicates physicians’ therapeutic decision-making because details on the treatment and survival of EC patients with SPC are limited. As such, we examined clinical features and survival outcomes of patients with SPC detected during initial staging of squamous EC using PET-CT.
METHODS
Patients
From a consecutively collected database, we identified a total of 317 patients diagnosed with squamous EC between June 2005 and December 2007. Of these, 21 patients had synchronous SPC that developed in a different organ. Relevant clinical, pathological and cancer-specific data were reviewed retrospectively. Multiple primary malignant tumors arising from other organs were defined according to the criteria of Warren and Gates [11]: (1) the tumors must be clearly malignant on histologic examination, (2) the tumors must be separated by normal mucosa, and (3) the possibility that the second tumor represents metastasis must be excluded. Accordingly, SPC in this study were distinguished from metastatic EC by cancer cell morphology, gland architecture, specific molecular markers and the pattern of tumor spread. All pathological results for both EC and SPC were confirmed at our institution.
The Institutional Review Board of the Asan Medical Center approved this study.
Diagnostic workup
Diagnostic evaluations included a complete medical history, physical examinations, laboratory blood analyses and pulmonary and cardiac function tests. All patients underwent esophagogastroscopy with biopsy, endoscopic ultrasonography, esophagography, chest-abdomen CT with contrast enhancement and 18F-fluorodeoxyglucose PET-CT. Bronchoscopy was performed if the EC was located at or above the carina. Tumor stage was determined according to the TNM staging system [12].
Treatment of squamous esophageal cancer
Patients with squamous EC were treated according to guidelines and institutions [13-16]. Briefly, patients with locally advanced and resectable EC (stage II and III; T2–3N0M0 and T1–3N1M0) were treated with preoperative chemoradiotherapy (CRT) followed by esophagectomy. Preoperative CRT consisted of cisplatin plus fluoropyrimidine-based chemotherapy with concurrent radiotherapy (46 Gy/23 fractions) over a 4-week period. Esophagectomy was performed 4 to 6 weeks after the end of preoperative CRT. Primary esophagectomy or endoscopic mucosal resection was performed for early EC (stage I; T1N0M0). Definitive CRT or palliative therapy was provided to patients with unresectable EC.
Statistical analysis
Baseline variables are presented as the number (percentage) and median (interquartile range, IQR). Continuous variables were compared using the Student t test and categorical variables were compared using the chi-square test or Fisher exact test. Survival outcomes were calculated using the Kaplan-Meier method and compared using the log-rank test. All p values were 2-sided and p > 0.05 were considered statistically significant. All statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Clinical features of esophageal cancer patients with and without synchronous second primary cancers
Median age of the study patients was 63 years (IQR, 58 to 70) and 95.0% of the patients were male (Table 1). Of patients with squamous EC, 21 (6.6%) had synchronous SPC and one patient had two SPC that arose from the stomach and lung. The majority of the patients had a history of smoking and alcohol consumption. There were significant differences in the median age (70 years vs. 63 years, p = 0.01), serum albumin level (3.3 g/dL vs. 3.9 g/dL, p < 0.01), and body mass index (20.4 kg/m2 vs. 22.8 kg/m2, p = 0.01) between EC patients with and without SPC. The Eastern Cooperative Oncology Group performance status, distribution of histologic grade and clinical EC stage were similar between the two groups.
Location of synchronous second primary cancers
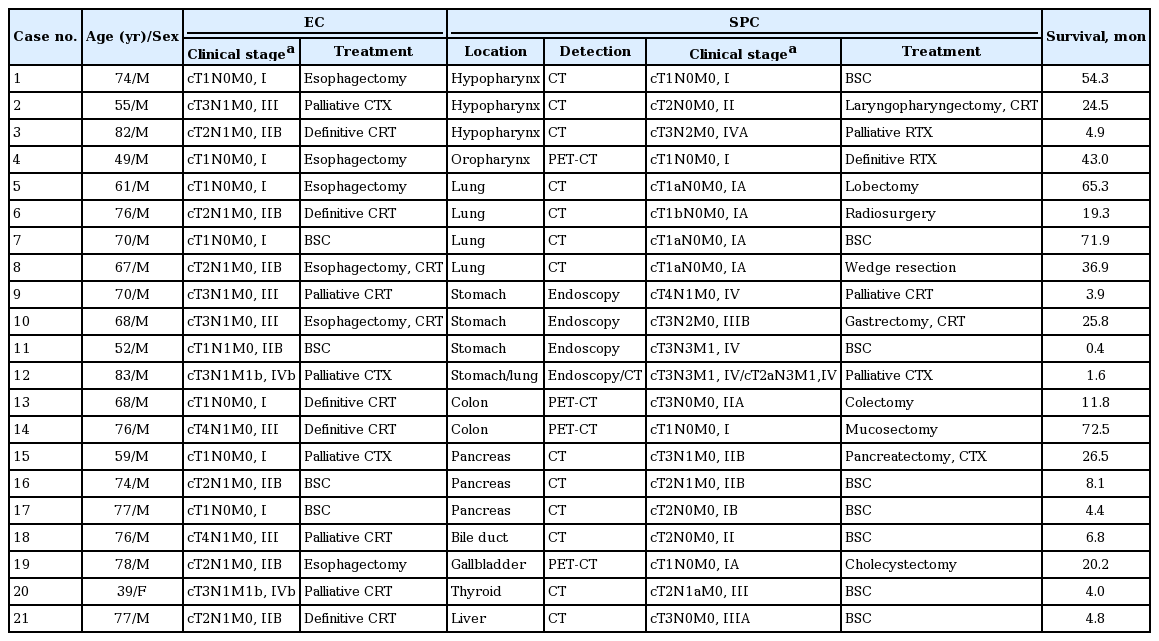
The locations of the 22 synchronous SPC are shown in Table 2. Head and neck and lung cancers were the most common SPC (40.9%), followed by gastric cancer (18.2%). Other intraabdominal SPC were diagnosed in eight patients (38.1%): pancreatobiliary cancer (five patients), colon cancer (two patients), and hepatocellular cancer (one patient). At the initial staging of EC, 14 SPC lesions were detected on chest-abdomen CT. Four cases (18.2%) of SPC, including three early-stage cancers were detected only on PET-CT (Table 3).
Treatment of esophageal cancer and synchronous second primary cancers
Treatments of the 21 patients with squamous EC and SPC are summarized in Table 3. Curative esophagectomy was attempted in 28.6% (6/21) of EC patients with SPC, whereas the rate was 59.1% (175/296) among EC patients without SPC (p = 0.006). Treatment plans were altered in 13 of 21 EC patients (61.9%) with SPC detection and were referred for non-surgical treatments including definitive CRT (five patients) and palliative therapy (eight patients).
Survival outcome of esophageal cancer patients with synchronous second primary cancers
After a median follow-up period of 19.0 months (IQR, 8.2 to 58.3), the median survival was 11.8 months (IQR, 4.2 to 31.7) for EC patients with SPC and 19.2 months (IQR, 8.8 to 58.9) for patients without SPC (Fig. 1). EC patients with SPC had a significantly lower 5-year survival rate compared with patients without SPC (10.6% and 36.7%, respectively; p = 0.008).
DISCUSSION
Patients with squamous EC have an increased risk of synchronous SPC, which has an incidence of 4.3% to 10.4% [1-4]. The most well known sites for SPC are aerodigestive tract organs, such as the oral cavity, pharynx, larynx and lung. Previous studies suggested that gastric cancer could be another common SPC, especially in regions with a high prevalence of gastric cancer [5-7]. In Japanese studies, the proportion of gastric cancer was estimated to be 17.5% to 32.6% of all SPC [1,2,4]. In our study, synchronous SPC were diagnosed in 6.6% of squamous EC patients and gastric cancer was the second most common SPC. Head and neck, lung and gastric cancers accounted for 18.2%, 22.7%, and 18.2% of SPC, respectively. Increased detection of SPC in the stomach may be due to the anatomic proximity of the organ, more frequent high-quality gastric screening with endoscopy and a high prevalence of H. pylori infection in Korea.
Given the well-known harmful effects of smoking, including increased risk of cancers such as aerodigestive tract and lung cancers, physicians should pay attention to the risk of synchronous SPC during the initial staging of patients with squamous EC [17]. In a previous study, it was found that approximately one-third of SPC were detected in the first six months after diagnosis of squamous EC [5]. These results emphasize the importance of accurate synchronous SPC diagnosis.
Recent technical progress in diagnostic methods may affect the clinical features of SPC. PET-CT is the standard modality for EC staging and planning multimodality therapy [18]. An earlier study reported that PET-CT was useful for screening SPC at the initial staging of malignancies, demonstrating 91% sensitivity and 69% positive predictive values for detecting SPC [8]. In our present study with squamous EC patients, metabolic imaging with PET-CT contributed substantially to the detection of additional synchronous SPC that were missed on conventional CT. Four cases (18.2%) of SPC in our current series, including three early-stage (cT-1N0M0) cancers, were diagnosed using PET-CT. Conventional CT on its own can miss early malignant lesions due to the mobility of body structures and normal variation [19].
Current evidence strongly recommends a multidisciplinary approach for treating patients with EC [13,15,16,20,21]. However, the unexpected detection of SPC poses difficulties for physicians’ therapeutic decision-making. Treatment plans for both EC and SPC may not be optimal due to technical complexity of surgical treatment, different biological behaviors of synchronous tumors, additional costs and increased patient anxiety. These factors may lead to stage-inappropriate treatment and, thus, poor outcome for EC patients. In our study, stage-appropriate treatment for EC could not be delivered to 13 of 21 patients (61.9%) when SPC was detected. The treatment plans for resectable EC were altered to non-surgical treatment including definitive CRT in five patients and palliative therapy in eight patients. Four patients diagnosed with early stage EC (cT-1N0M0) could not receive curative esophagectomy.
The prognosis of EC patients with SPC is unclear [1-3,6]. Our study reported poor survival outcomes for these patients: 3- and 5-year survival rates were 25.0% and 10.6%, respectively. A recent study proposed surgical treatment should be considered for select EC patients with synchronous SPC [22]. The rate of curative resections for both EC and SPC was 87.5% in patients with gastric cancer, 52.9% in lung cancer and 47.1% in head and neck cancer. Five-year survival rates after surgery for EC in patients with stomach, lung, and head and neck cancer were 52.7%, 27.0%, and 9.2%, respectively.
Under-nutrition is an important negative prognostic factor for EC patients [16,23]. Our findings that EC patients with SPC are older and have significantly lower serum albumin and body mass index than those without SPC may also contribute to poor prognosis. Significant differences in the median age at EC diagnosis, serum albumin and body mass index may be due to an increased risk for SPC with age and advanced stage of synchronous cancer in some SPC patients [5,6].
Major limitations of this study include its retrospective design and the fact that observation data were collected from a single tertiary referral center. In addition, factors known to be important to survival, such as stage of SPC and details regarding chemotherapy and/or radiation therapy for SPC, could not be evaluated in our study. Therefore a future comprehensive study should be done to analyze the treatment outcome of EC patients based on SPC stage. Furthermore, clinical implications of pre- and post-metachronous cancers could not be assessed in the present study as we focused on synchronous SPC detected during initial EC staging.
In conclusion, physicians should be aware of the co-existence of SPC with squamous EC as SPC were found in 6.6% of patients during the initial staging of squamous EC in our study. PET-CT detected additional cases of SPC that were missed on conventional CT. EC patients with synchronous SPC showed different clinical features and had poor survival due to challenges in providing stage-appropriate treatment.
KEY MESSAGE
1. Second primary cancers (SPC) were found in 6.6% of squamous esophageal cancer (EC) patients at initial staging work-ups; therefore, physicians should be aware of the co-existence of SPC with squamous EC.
2. Complementary staging with positron emission tomography-computed tomography (PET-CT) plays a substantial role in the detection of synchronous SPC that were missed on conventional CT.
3. EC patients with SPC had poor survival due to the challenges in providing stage-appropriate treatment.
Notes
No potential conflict of interest relevant to this article was reported.