INTRODUCTION
Achalasia was first described by Thomas Willis in 1674 [1]. A Greek term, achalasia literally means “non-relaxing” and refers to the dysfunctional lower esophageal sphincter (LES). As an incurable disease, the treatment of achalasia has always been palliative, aimed at relieving the solid food dysphagia that is the hallmark symptom. Secondary endpoints of treatment include the reversal of weight loss and the arrest of progressive esophageal dilation. In patients with end-stage achalasia, treatment may be directed toward the prevention of chronic aspiration.
Achalasia is a rare disease. The population incidence of idiopathic achalasia is estimated to be 1:100,000 and is remarkably consistent geographically. There is a bimodal age distribution, with most patients in the 20 to 40 and 60 to 70 age groups [2]. Achalasia related to Chagas disease is regionally endemic throughout Central and South America and associated with the presence of the parasite (Trypanosoma cruzi) vector, the reduviid beetle [3]. Public health policy and early parasite treatment have dramatically decreased the number of Chagas-disease-related achalasia cases worldwide, but this form of the disease remains a problem in poorer rural areas.
The etiology of achalasia is poorly understood despite > 200 years of investigation. An exception is the primary dysmotility resulting from infection with T. cruzi, as mentioned above [4]. Chagas disease is a multi-organ condition, the esophageal manifestations of which have a manometry profile similar to that of standard achalasia, i.e., no primary peristalsis in the esophageal body and a non-relaxing LES. There is also an extremely rare genetically linked form of achalasia that is associated with severe genetic abnormalities such as triple A syndrome [5]. According to current thinking, achalasia is probably an autoimmune disorder, perhaps a cross-immune reaction against herpes simplex virus or other viruses [6]. Regardless of the etiology, once aperistalsis is established it is not reversible by any currently available treatment, although there are anecdotal reports of vestigial primary peristaltic contractions following a peroral endoscopic myotomy (POEM) procedure [7]. Nonetheless, most forms of treatment result in a substantial palliation of symptoms in the majority of patients, allowing them to resume a more or less normal diet, sustain their weight and avoid the progressive dilation that eventually leads to esophagectomy or death from aspiration.
DIAGNOSTICS
Achalasia is diagnosed based on the clinical symptoms and the results of imaging and physiology studies. Symptoms almost universally include solid food dysphagia, with associated symptoms of regurgitation, chest pain and heartburn. Weight loss, once a uniform component of achalasia presentation, is more variable today due to the widespread availability of high-calorie liquid foods. Because many achalasia patients complain of symptoms mimicking those of gastroesophageal reflux disease (GERD), especially heartburn reflux, they are often erroneously diagnosed with GERD and treated accordingly. However, these symptoms are most likely related to esophageal stasis and not to gastro-esophageal reflux, as the LES is non-relaxing. Chest pain is also a highly variable and non-specific symptom and may be from other sources, such as cardiac disease, or other esophageal spastic disorders, such as diffuse esophageal spasm. Achalasia symptoms are routinely quantified by the Eckhardt score [8], which, while not truly validated as a quantitative score, is widely used in the follow-up of patients and is an important assessment tool in this chronic, non-curable disease (Table 1).
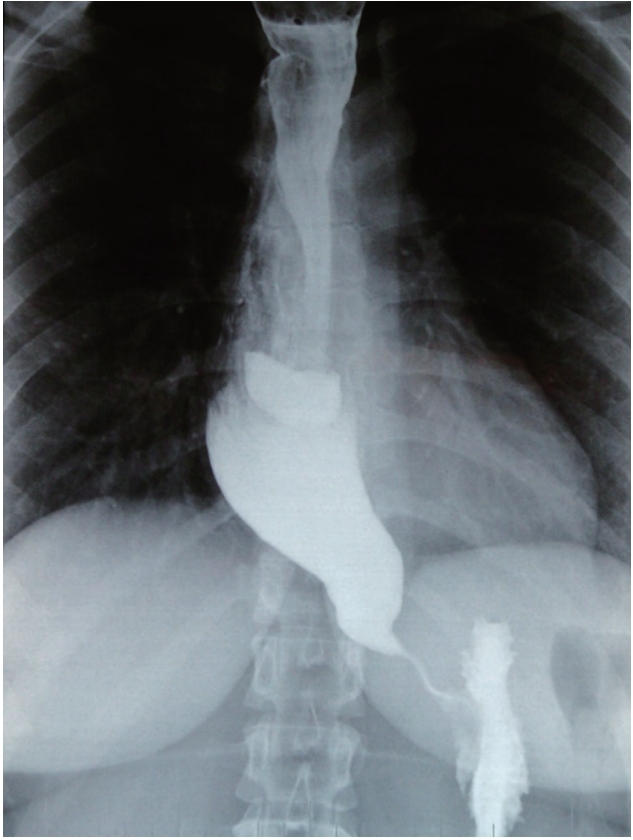
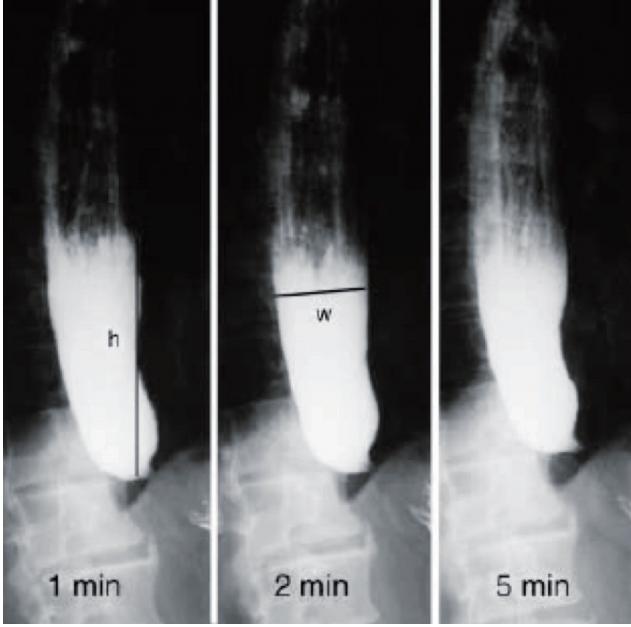
Imaging studies provide a nearly pathognomonic test. Typical findings include esophageal body dilation with distal smooth narrowing at the LES (“birds beak” deformity) (Fig. 1). A contrast X-ray, if available at the hospital’s facilities, can also serve as a quantitative follow-up tool. In a “timed barium swallow,” the patient, in an upright position, is given a standardized quantity of barium, after which still images are obtained at set intervals (5, 10, 15 minutes). The height of the retained barium column at each interval is the metric, with a normal esophagus clearing the barium dose by 5 minutes (Fig. 2).
Patients with achalasia who complain of GERD symptoms typically undergo 24-hour pH testing, but the test results are difficult to interpret as they are often positive due to the stasis and fermentation associated with achalasia. Therefore, the test is not diagnostically useful, as achalasia patients almost never have true GERD and, even if they did, their treatment options would not change substantially.
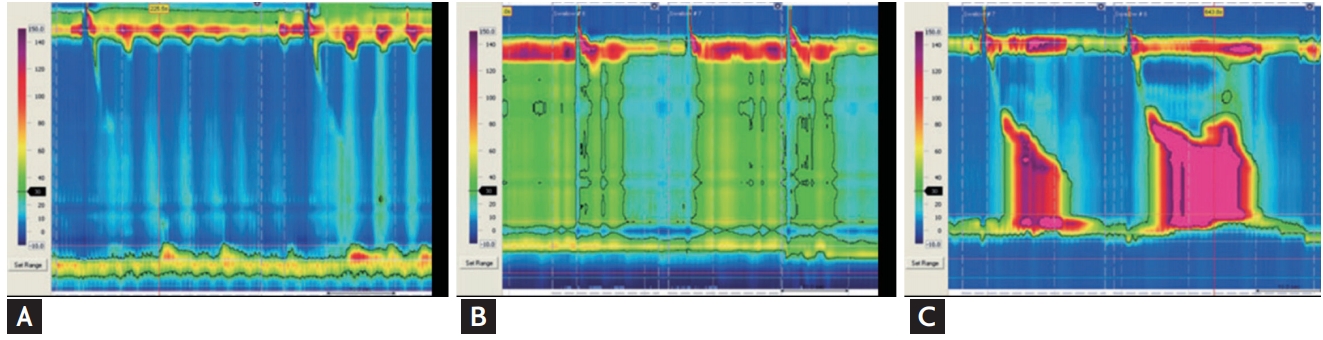
The most critical diagnostic test is esophageal manometry and, in particular, high-resolution manometry (HRM). In fact, the very definition of achalasia is based on the manometry criteria: a complete absence of progressive primary peristaltic contractions and an incompletely relaxing LES (not a hypertensive LES as once described, as the LES can be hypertensive, normotensive or even hypotensive). Since early 2000, the large volume of data collected by HRM has contributed to a further understanding of achalasia and has led to the development of the Chicago classification scheme, which separates achalasia into types I, II, III [9]. In type I, there is a complete absence of esophageal contractions, in type II simultaneous pressurization, and in type III high-pressure non-peristaltic body contractions (Fig. 3). Moreover, the Chicago classification correlates with treatment outcome, as different success rates can be expected in the treatment of disease with different classifications [10].
TREATMENTS
Currently, there are several relatively good palliative treatments for achalasia, each with its advantages and disadvantages, and a place in the treatment algorithm.
Botox
The injection of botulinum toxin into the LES has been a popular form of palliation since it was first described by Pasricha et al. [11], in 1993. The typical treatment regime is the injection of 100 units of reconstituted Botox, divided into four aliquots, into the LES in four quadrants. This can also be done under endoscopic ultrasound visualization, even though there is no convincing evidence that it improves outcome. While Botox is safe, relatively effective (80% early dysphagia relief) and minimally invasive, it has two major drawbacks that prevent it from being a frontline treatment [12]. The first is its transient effectiveness. Despite good early results, the effect substantially fades over time, with 60% of patients having recurrent dysphagia at 1 year and 80% at 2 years. The second is that intramuscular Botox injections cause submucosal fibrosis, which interferes with subsequent definitive treatments [13]. For these reasons, Botox is generally recommended only for patients who are poor medical candidates for definitive treatment or as a transient palliation for very acute cases (e.g., total outlet obstruction in patients in whom timely, definitive treatment is not possible) [14].
Pneumatic dilation
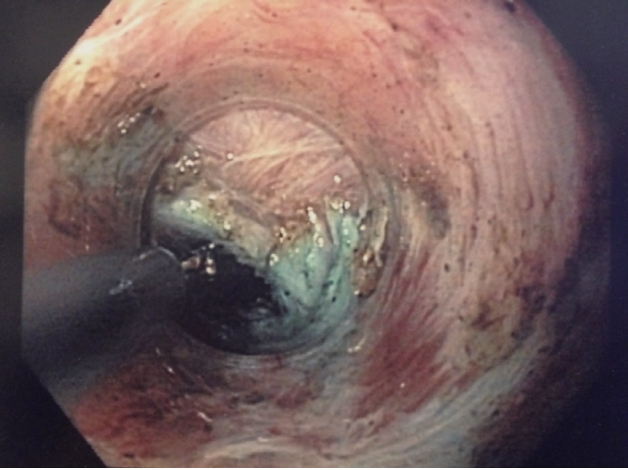
The popularity of pneumatic dilation (PD) has waxed and waned for several decades. The technique involves placement of a fixed-diameter, high-pressure dilating balloon across the LES, usually under fluoroscopic visualization. Dilation is performed until the balloon waist is seen to disappear. The balloons are typically 30 or 35 mm in diameter, with most current protocols calling for dilation with the 30-mm balloon followed by the 35-mm balloon if adequate results are not obtained [15]. Early results are good, with 70% of patients experiencing a substantial relief of dysphagia at 6 months after a mean of two dilation episodes [16]. However, late-term follow-up has documented decreasing success over time, with only 36% of patients still having dysphagia relief after 20 years [17]. Several studies have shown better results with PD in patients over 40 years of age [18] and worse outcomes in patients with Chicago type III achalasia (60% vs. 93% Chicago I/II) [19]. The risk of esophageal perforation is 3% to 6%, which is the major reason why PD remains controversial in terms of its acceptance [20], although most of the perforations occurring with PD can be treated conservatively [21]. Impedance planimetry using a proprietary 30-mm balloon allows achalasia dilation without fluoroscopy and under very controlled conditions. It may rejuvenate interest in PD (Fig. 4).
Laparoscopic Heller myotomy
A minimally invasive Heller myotomy (HM) involving a thoracoscopic approach was first described by Pellegrini et al. [22]. Yet, while the thoracoscopic approach replicated the classic open surgical method it was quickly abandoned due to poor results [23]. Subsequently, excellent results and great patient benefit were obtained using a laparoscopic approach, which quickly became the gold standard surgical treatment [24,25]. A landmark study by Richards et al. [26] from Vanderbilt University (Nashville, TN, USA), confirmed the need to add a partial fundoplication to the myotomy to minimize the incidence of iatrogenic GERD.
Laparoscopic HM has become a fairly well-standardized procedure: a five-laparoscopic port approach is used, with mobilization of at least the anterior 180° of the gastroesophageal junction and distal esophagus (360° if a Toupet is planned) followed by a full-thickness myotomy that is extended to the distal esophagus at least until the hiatus of the diaphragm. We tend to avoid extension of the myotomy into the free mediastinum due to the risk of late-term saccular dilation of the myotomy site. The traditional 2-cm extension of the myotomy onto the anterior stomach wall has been challenged by a prospective study by Oelschlager et al. [27], which showed better outcomes with a 3-cm extension.
The type of fundoplication that is added following the myotomy remains controversial. The Dor anterior 180° wrap and the Toupet 270° posterior wrap are the most commonly used, but there are rare anecdotal reports advocating a 360° Nissen fundoplication. Among the arguments for the Dor procedure are that it requires less hiatal dissection and covers the exposed mucosa of the myotomy site, which may offer protection in case of perforation. Advocates of the Toupet procedure claim that its 270° wrap prevents reflux more effectively, and that fixation to the edges of the myotomy helps to prevent the myotomy site from healing in a closed position. However, there are as yet no studies providing conclusive support for one or the other procedure, and the choice of fundoplication continues to be a matter of the surgeon’s preference [28,29].
Per-oral endoscopic myotomy
POEM is the offspring of the natural orifice transenteric endoscopic surgery (NOTES) procedure adopted in the late 2000s. In seeking a safe exit strategy from the gastrointestinal tract by sub-mucosal tunneling, Pasricha et al. [30] discovered that they could visualize the circular muscle of the LES clearly during tunneling, and proposed that achalasia myotomy would be feasible. They presented a proof of concept in four pigs in 2009 [30]. Inoue et al. [31], a surgical endoscopist, first applied this concept to humans in 2010 and coined the term “POEM.”
POEM utilizes the skills and tools common to advanced surgical endoscopy techniques, such as endoscopic sub-mucosal dissection. The procedure is designed according to the manometry findings, with a short myotomy for Chicago types I and II and a long myotomy for Chicago type III and spastic disorders. A mucosal lift with methylene blue saline is created 3 cm proximal to the planned start of the myotomy and a longitudinal incision extending to the muscularis propria is made. An endoscope fitted with a dissecting cap is introduced into this submucosal plane, after which a tunnel is dissected down to and across the LES and 2 to 3 cm onto the proximal wall of the stomach. Once the tunnel is created, the endoscope is pulled back to the proximal tunnel and the myotomy is started by selectively dividing the circular muscle fibers (Fig. 5). At completion, the mucosal opening is closed using hemostatic clips.
Over the last 10 years, POEM has been rapidly adopted and is now the primary form of treatment at the majority of high-volume achalasia centers. The literature contains an enormous number of studies, both from single centers describing short-term outcomes, including some series with more than 1,000 patients [32], and from multiple centers reporting 1- and 2-year [33,34] and even 5-year [35] outcomes. Together, these reports have confirmed the safety of POEM, as major operative and postoperative complications are rare, as is the need for conversion to a surgical approach. No studies reporting POEM-related mortality have been published to date, although there are anecdotal reports. Summarizing the literature on POEM, successful relief of dysphagia by POEM, as defined by an Eckhardt score < 3, is > 90% after short-term and > 80% after long-term follow-up. The incidence of iatrogenic GERD following POEM in the early days of the procedure varied widely, ranging from no reflux to an incidence of almost 50% [36-38]. As descriptions of GERD symptoms following any type of achalasia treatment are absolutely unreliable [39], the most reliable data are those obtained by pH monitoring. Based on several series reporting objectively determined reflux, the incidence of post-POEM GERD is between 30% and 40% [40]. The incidence of patients whose GERD symptoms cannot be controlled medically and require antireflux surgery is very low.
To date, there have been no randomized prospective studies comparing POEM with other achalasia treatments. This is due, in part, to the rarity of achalasia in the population and to the fact that non-randomized results are highly equivalent to the best endoscopic or surgical treatment, such that powering such a randomization is a daunting proposition. Retrospective comparisons between, in particular, laparoscopic HM and POEM [41] have shown similar rates of complication and a similar safety profile, slightly better relief of dysphagia, and an equal or slightly higher incidence of reflux or reflux symptoms. Again, the differences in these compiled studies between dysphagia relief and GERD incidence are so small, and the disease so rare, that an adequately powered randomized study that truly defines the best treatment cannot reasonably be expected.
EMERGING TREATMENTS
As with all chronic non-curable diseases, achalasia continues to generate new ideas aimed at addressing the symptoms or even the disease.
De Palma et al. [42] first described the use of esophageal stents in 1998 and, in the following years, have sporadically updated their experience. Initially, esophageal stenting was specifically indicated for patients with end-stage disease that had not responded to other treatments. However, several groups have since reported on stenting as a primary treatment for achalasia based on two general strategies: long-term (months) implantation of a regular-sized stent (20 to 25 mm) or short-term (< 1 week) implantation of a large-diameter (30-mm) stent. The former strategy has been largely abandoned due to high complication rates (migrations and serious erosions) and poor long-term results (49% at 36 months) [43,44]. The results obtained using a specially designed 30-mm stent implanted for < 1 week have been better, with lower migration rates (6%) and remission rates of > 80% at up to 2 years follow-up. However these larger stents are associated with significant rates of chest pain [45].
CONCLUSIONS
Achalasia as a rare esophageal motility disorder which, while seldom lethal, still represents tremendous patient morbidity and distress. While the etiology of the disease is poorly understood, there are a wide spectrum of moderately effective palliative treatments ranging from endoscopic to open surgical treatments. Today, the current "gold standard" treatment of laparoscopic heller myotomy with partial fundoplication is being overtaken by endoscopic myotomy (POEM) which has a ten year history of safety and efficacy. The issue of post procedure GERD, a problem with pneumatic dilatation and surgical myotomy, is again a topic of concern as its incidence is somewhat higher following POEM. This indicates that there is still research remaining to be done on achalasia as a disease.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





