METHODS
Study population
All data of the study population were derived from the Korea Acute Myocardial Infarction Registry-National Institutes of Health (KAMIR-NIH) registry, based on a nationwide, multicenter, and web-based observational cohort study. This registry incrementally collected data on patients with AMI from approximately 20 PCI-eligible major cardiovascular hospitals between November 2011 and December 2015. It contains clinical information on the characteristics and outcomes of patients with AMI in the Republic of Korea. These data were obtained by attending medical doctors and trained clinical research coordinators via the web-based case report form in a clinical data management system. The published protocol for the KAMIR-NIH was approved by the ethics committee of each participating hospital [
5].
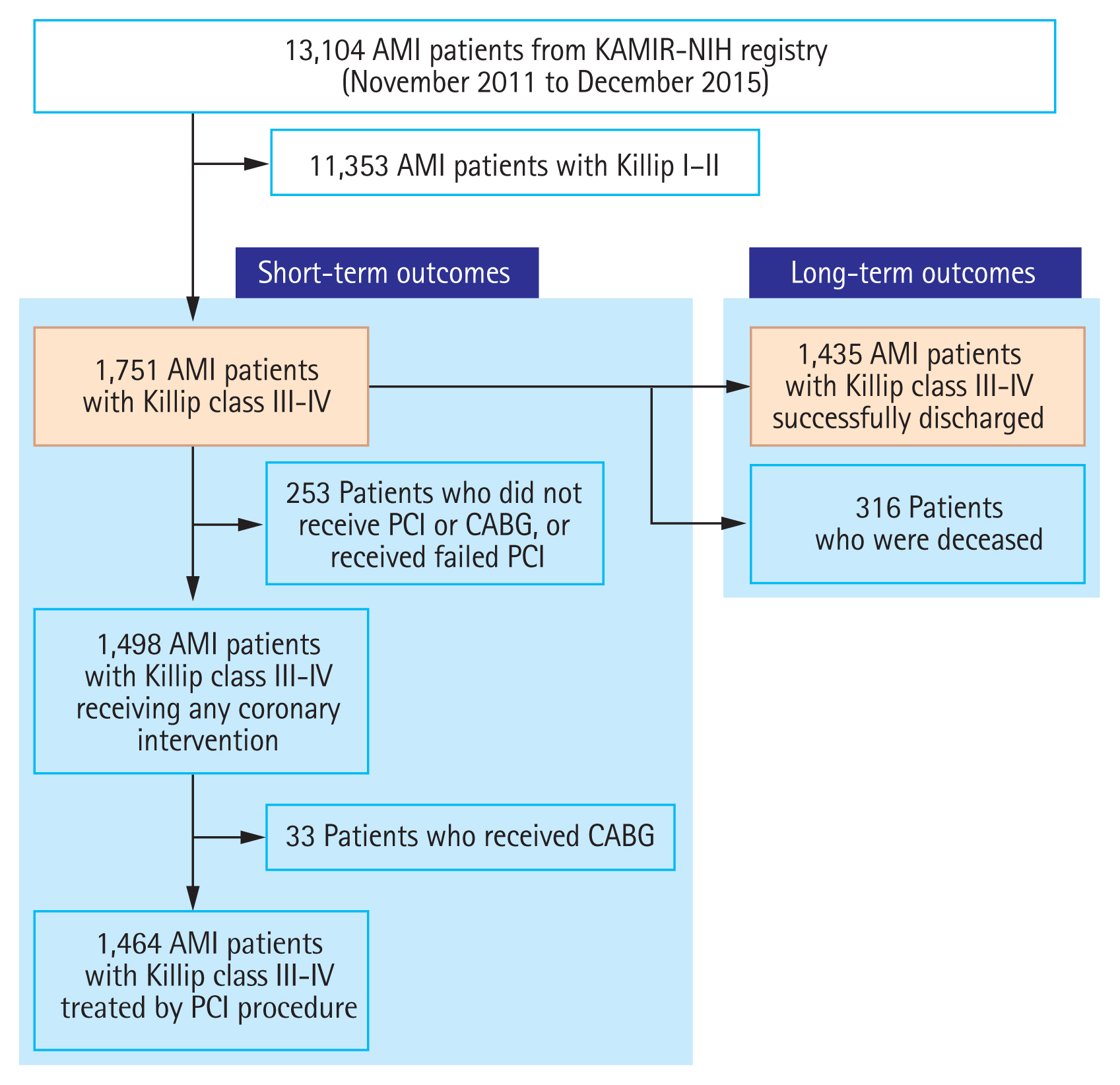
In the KAMIR-NIH registry, 13,104 patients with AMI were initially screened. After 11,353 patients with AMI who presented with Killip classes IŌĆōII were excluded, a total of 1,751 patients with Killip IIIŌĆōIV AMI were selected, and their short-term outcomes were assessed. Among them, 316 patients who died during the index hospitalization were excluded, and long-term outcomes of a total of 1,435 patients were analyzed. All study patients were allocated into two groups according to the date and time of hospital visit for PCI procedure (i.e., off-hour vs. on-hour group). All survivors were followed up through outpatient visits at regular intervals. The study design is illustrated in
Fig. 1.
Our study was conducted according to the ethical principles of the Declaration of Helsinki, which was revised in 2013 [
6]. Written informed consent was obtained from all the enrolled patients.
Definitions and clinical endpoints
AMI was defined in accordance with current guidelines [
7], which comprise the typical rise and/or fall of cardiac biomarkers (troponin-I) in at least one of the following: (1) clinical symptoms or signs suggestive of myocardial ischemia; (2) development of pathological Q-waves in the 12-lead electrocardiogram (ECG); (3) ECG changes suggestive of myocardial ischemia (i.e., stent thrombosis [ST]-segment elevation or depression); and (4) characteristic cardiovascular imaging features suggestive of AMI (i.e., new loss of myocardial viability or newly found regional wall motion abnormality). ST-segment elevation myocardial infarction (STEMI) refers to AMI with new-onset ST-segment elevation of at least 1 mm (0.1 mV) in Ōēź 2 contiguous leads or new-onset left bundle branch block on surface ECG. First medical contact (FMC) was defined as the time at which the medical personnel arrived to support the AMI patient [
7,
8]. During FMC, emergency medical service (EMS) was used in two cases and not used in another two cases. Patients with no EMS use were divided into two groups (first immediate visit to a PCI-capable center or to a PCI-incapable center). Total ischemic time (TIT) was defined as the time from the onset of angina to the first balloon inflation during the primary PCI.
All demographic and clinical characteristics of the study patients were recorded. Left ventricular ejection fraction (LVEF) was evaluated using two-dimensional echocardiography. Body mass index (BMI) was measured using the patientŌĆÖs weight and height. Angiographic and procedural characteristics were also recorded. Image-guided PCI was defined as the use of optical coherence tomography or intravascular ultrasound during the primary PCI. Infarct-related artery referred to an epicardial coronary vessel that was blocked or stenosed by an atheromatous or thrombotic pathologic process and was directly responsible for acute coronary syndrome. The degree of coronary flow was quantitatively classified according to thrombolysis in myocardial infarction (TIMI) flow grade [
9].
All patients were classified based on the day and time of arrival to the hospital. Patients who arrived during normal working hours on weekdays from 8:00 AM to 6:00 PM were allocated to the on-hours group; patients who arrived during weekdays from 6:01 PM to 7:59 AM or during the weekend were allocated to the off-hours group. The weekend was defined as the period that included Saturdays, Sundays, and all public holidays in the Republic of Korea.
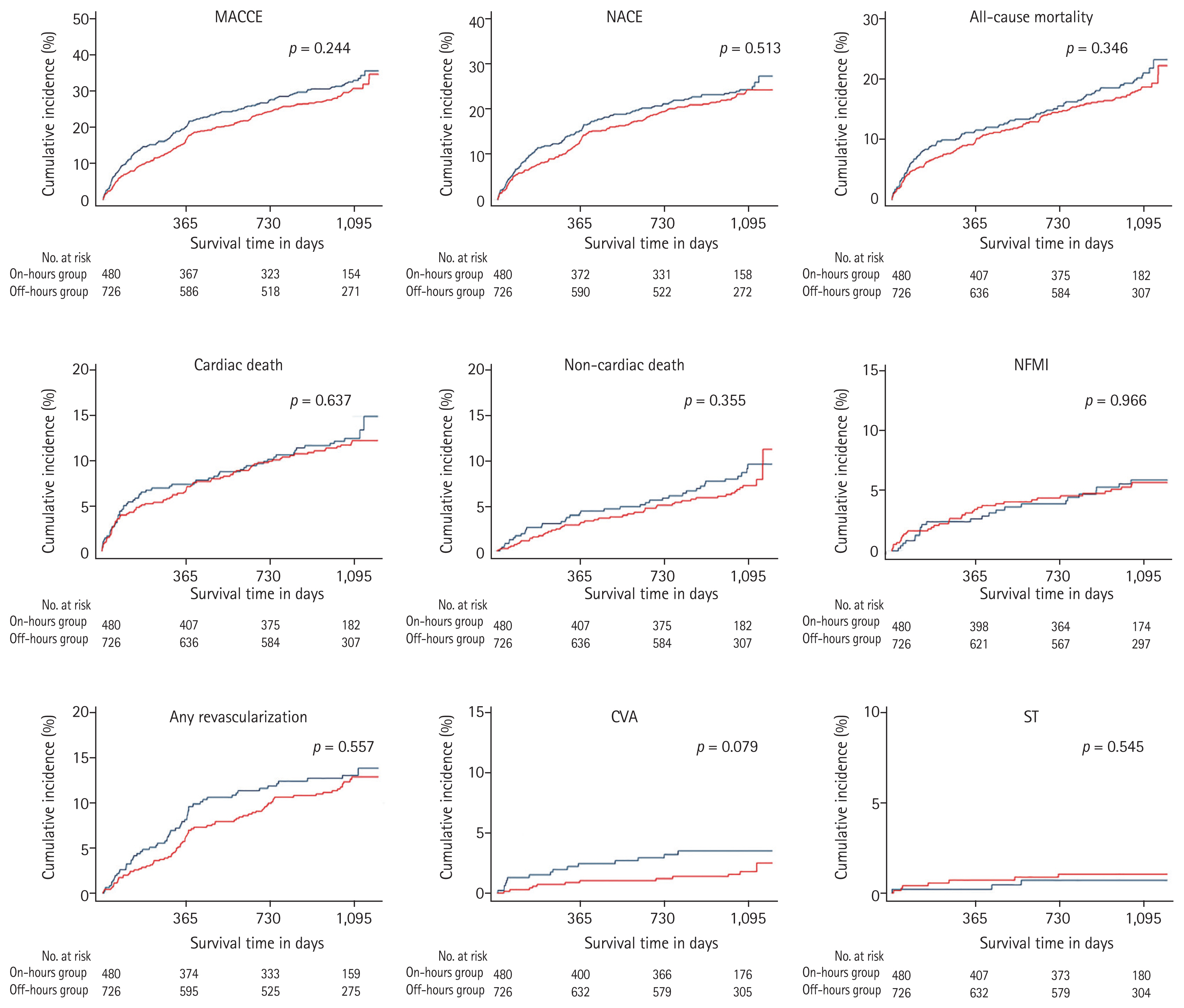
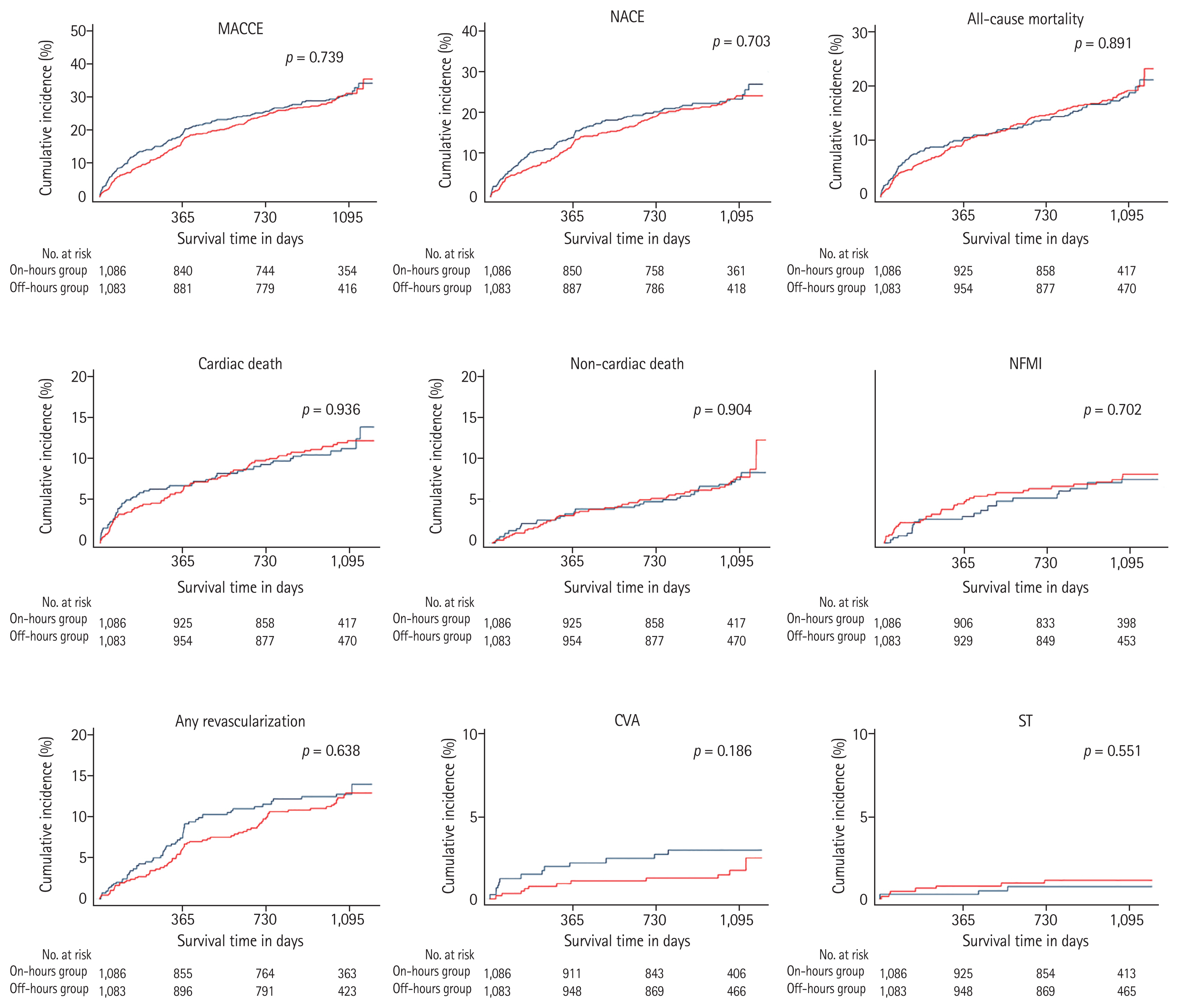
After the study commencement, the clinical follow-up was performed for 3 years. The primary outcome was the occurrence of major adverse cardiac and cerebrovascular events (MACCEs). MACCEs were defined as a composite of all-cause mortality (cardiac and non-cardiac death), nonfatal myocardial infarction (NFMI), any revascularization (any redo PCI or coronary artery bypass graft), cerebrovascular accident (CVA), and ST. As for the secondary outcomes, we also explored the occurrence of net adverse clinical events (NACEs), all-cause mortality, cardiac and non-cardiac death, NFMI, any revascularization, CVA, and ST. NACEs referred to a composite of cardiac death, NFMI, and any revascularization.
Statistical analysis
Statistical analysis was commenced to explore the differences in clinical outcomes between the two groups classified according to the date and time of hospital visit. Continuous variables were described as mean ┬▒ standard deviation and were analyzed using StudentŌĆÖs t test. Discrete (categorical) variables were described as percentages with numbers and were analyzed using PearsonŌĆÖs chi-squared test or FisherŌĆÖs two-by-two exact test. Statistical significance was set at p < 0.05.
To minimize the effect of selection bias during the statistical analysis of observational registry data, two propensity score weighting methods including propensity score matching (PSM) and inverse probability of treatment weighting (IPTW) were used. The propensity score was formulated using a multiple logistic regression model with a total of 31 covariates, which included sex, age Ōēź 65 years, FMC (EMS, PCI-capable center, and PCI-incapable center), TIT Ōēź 12 hours, onset-to-door time (O2DT) Ōēź 4 hours, door-to-balloon time (D2BT) Ōēź 90 minutes, pulse pressure Ōēź 40 mmHg, Killip functional class (III or IV), BMI Ōēź 25 kg/m2, previous history (hypertension, diabetes mellitus, dyslipidemia, prior myocardial infarction, prior heart failure, and prior CVA), smoking (current or ex-smoker and nonsmoker), family history of coronary artery disease, LVEF < 40%, final diagnosis (STEMI or non-STEMI), discharge medications (aspirin, P2Y12 inhibitor, calcium channel blocker, beta-blocker, angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, and statin), and angiographic characteristics (uses of the transfemoral approach, glycoprotein IIb/IIIa inhibitor, thrombus aspiration, and thrombolysis, preprocedural TIMI flow grade, and anatomical site of the infarct-related artery, i.e., the culprit vessel). Participants with missing data among these covariates or those who were lost to follow-up after hospital discharge were excluded from the analysis with PSM and IPTW adjustments.
The analysis of cumulative events was commenced with time-to-event data through the KaplanŌĆōMeier method. Patients were censored at the time of the event or at the final follow-up. KaplanŌĆōMeier survival curves were created for the time of occurrence of clinical outcomes and compared using the log-rank test.
All analyses were performed using SPSS version 25.0 (IBM Corp., Armonk, NY, USA).
Statement of human rights
The present study was conducted according to the ethical principles of the Helsinki Declaration. The study protocol for KAMIR-NIH registry was previously published and approved by the ethics committee of each participating medical center (IRB No. CNUH-2011-172). The present study was conducted retrospectively based on the KAMIR-NIH registry (IRB No. CNUH-2021-380).
DISCUSSION
We evaluated the short- and long-term clinical outcomes among patients with Killip IIIŌĆōIV AMI, depending on the time and date of hospital presentation. We analyzed a total of 1,751 consecutive patients with a confirmed diagnosis of Killip IIIŌĆōIV AMI, which was derived from the KAMIR-NIH registry. This study revealed that the long-term outcomes of these patients admitted during off-hours were similar to those admitted during on-hours. The off-hour group had a higher proportion of pre-hospital EMS utilization but a lower proportion of O2DT Ōēź4 hours than the on-hour group. In terms of procedural characteristics, the off-hour group was found to receive a higher frequency of thrombolysis treatment than the on-hour group.
Contrary to our common belief that off-hour presentation may be related to delayed reperfusion time, the TIT in both groups was significantly comparable. Notably, the off-hour group showed shorter O2DT than the on-hour group. There may be various reasons for the disparities of O2DT between both groups. Considering the lower EMS utilization rates in the on-hours group, it was thought that on-hours patients tended to visit the hospital directly or wait patiently despite the occurrence of angina symptoms and signs. However, a longer D2BT was observed in the off-hour group, which was considered to be insignificant. Considering that most patients with Killip IIIŌĆōIV AMI were more hemodynamically unstable than the general AMI population, it can be inferred that sufficient backup for these medical conditions including the availability of skilled staff, level of staffing capacity, and the number of paramedics may be inadequate during off-hours as compared to during on-hours. It can also be assumed that these points were involved in the slight increase in D2BT in the off-hour group. Based on these findings, it could be considered that the short O2DT, mainly induced by the high EMS utilization rate in the off-hour group, compensated for the slightly long D2BT and led to a similar TIT.
In addition to the present study that focused on the long-term clinical outcomes of these patients who presented during off- versus on-hours, we also analyzed the short-term clinical outcomes. At first, in-hospital outcomes included in-hospital death, hopeless discharge, in-hospital complications, and supportive treatment, which are summarized in
Supplementary Table 1. Unlike all analyses of long-term clinical outcomes, this investigation included all patients with AMI and Killip class IIIŌĆōIV who underwent PCI. Although it was statistically insignificant, the off-hours group tended to have higher proportions of cardiogenic shock (36.8% [n = 328] vs. 32.5% [n = 186],
p = 0.096), new-onset heart failure (16.4% [n = 146] vs. 13.1% [n = 75],
p = 0.090), and multi-organ failure (10.5% [n = 94] vs. 8.0% [n = 46],
p = 0.083). Nonetheless, there was no significant difference in terms of in-hospital death nor hopeless discharge. Among 1,435 survivors, 6-month outcomes, which included MACCE, NACE, all-cause mortality (cardiac and non-cardiac death), NFMI, any revascularization, CVA, and ST, demonstrated no significant difference between the two groups (
Supplementary Table 2).
In the Republic of Korea, the emergency medical response system is a publicly operated system that started in 1982 through the establishment of the 119 Rescue team from > 10 fire stations [
10]. This system consists of a total of four parts: accident scene phase, transport phase, hospital phase, and communication system. Among them, the 119 Rescue team contributes to the quick transport of emergency patients to capable medical centers via emergency vehicles. The importance of the pre-hospital emergency case in terms of AMI was emphasized in a literature review [
11ŌĆō
14]. Patients with STEMI and out-of-hospital cardiac arrest tended to have significantly higher rates of system delay and mortality [
14] and were less likely to be transported directly to a PCI-capable medical center than their counterparts without out-of-hospital cardiac arrest [
13]. A meta-analysis revealed that a short transit time with lower TIT and D2BT contributed to better clinical outcomes with lower mortality. In the Republic of Korea, EMS utilization was shown to be a factor that reduces O2DT, as evidenced in a clinical study based on the KAMIR-NIH registry [
15]. Given the low EMS utilization rate and shorter O2DT in regular hours (as mentioned earlier), sufficient education on the utilization of 119 Rescue team during the daytime and public awareness about AMI is necessitated.
Off-hour presentation is traditionally attributed to worse long-term results in patients with AMI [
16,
17]. This belief has been supported by several proposed mechanisms, such as the lower likelihood of timely PCI [
18,
19], disparities in the healthcare delivery system between during off-hours and on-hours [
20,
21], reduced level of staffing capacity [
16,
22], and unbalanced inclusion of severe medical conditions, such as cardiac arrest or cardiogenic shock [
1,
17,
18]. Nonetheless, recent studies found similar long-term outcomes in the off- and on-hour groups. The 1- or 2-year mortality rates have been reported to be similar in patients with STEMI presenting during on- and off-hours [
4,
23,
24]. Suwa et al. [
4] reported that patients with STEMI presenting during off-hours had similar 3-year clinical outcomes to those who presented during regular hours. According to a meta-analysis, patients with STEMI presenting during off-hours had similar short-, intermediate-, and long-term (3ŌĆō4 years) outcomes to those who presented during regular hours [
23]. Off-hour presentation showed similar outcomes to on-hour presentation in the Korean STEMI population, as well [
25].
Additionally, we investigated the characteristics and clinical outcomes of other 253 patients who did not receive PCI or coronary artery bypass graft, or received failed PCI (
Supplementary Tables 3 and
4). In the baseline characteristics of these patients, no significant differences were noted. As for the treatment outcomes, there were also no significant differences between the off- and on-hours groups. However, the incidence of MACCE up to 3 years were as follows: overall population (51.7%), on-hours group (49.3%), and off-hours group (53.4%). These were significantly higher as compared to the MACCE rates in PCI-treated population, which indicated the effectivity of PCI for reducing mortality in the AMI population, as some previous studies have demonstrated [
26].
We investigated the characteristics of 316 patients who were deceased during the index hospitalization (
Supplementary Table 5). As compared to the overall study population, they had higher proportions of age Ōēź 65 years, STEMI, Killip functional class IV but lower LVEF, which indicated a high disease severity. Interestingly, TIT was more prolonged despite the higher EMS utilization rate. Since these patients had a higher proportion of STEMI requiring timely and rapid reperfusion, D2BT would have been shortened. Nonetheless, O2DT would have been greatly prolonged, which may be possibly due to some patient-based factors. Given that elderly patients with AMI tend to experience atypical angina or no chest pain, the inclusion of higher frequency of elderly patients would have contributed significantly to the pre-hospital delay. Hence, this treatment delay, which was mainly driven by delay of O2DT and not D2BT, consequently contributed to the poor prognosis, including in-hospital death.
We also investigated the clinical outcomes of 17 patients who received thrombolysis during the index hospitalization (
Supplementary Table 6). All patients presented with STEMI during off-hours. Thirteen patients were male, and five were aged > 65 years. Fourteen patients received PCI, and 11 among them had prolonged D2BT (D2BT Ōēź 90 minutes). Two patients who did not receive PCI and one patient who did not arrive at the hospital within 12 hours of pain onset (i.e., O2DT Ōēź 12 hours) were deceased during the index hospitalization. As for long-term clinical outcomes, only two patients experienced MACCE. This indicated that although thrombolysis was an alternative option in a clinical situation a delayed PCI, primary PCI had a clear advantage in STEMI.
The results of our study emphasized that patients with Killip IIIŌĆōIV AMI admitted during off-hours had similar outcomes as those admitted during on-hours. It meant that the same medical services were provided to these patients regardless of the hospital visit time. These results may be presumably explained by technological, procedural, and pharmacological innovations in the treatment of cardiovascular disorders. As many clinical studies have shown the effectiveness and safety of PCI in reducing the mortality in patients with AMI [
26], catheter-based PCI became the mainstay of reperfusion therapy in these patients, and it underwent a series of innovations from only balloon-based angioplasty through bare-metal stents to drug-eluting stents [
27]. According to a study on the status and temporal trend of PCI in the Republic of Korea, the estimated annual PCI rate and the number of PCI-capable medical institutions have increased annually [
28]. Furthermore, the proportion of centers capable of a PCI volume Ōēź 500/year was markedly increased [
29]. Many advances have also been made in the clinical field of comprehensive post-PCI pharmacological treatment after many randomized clinical trials have focused on the optimization of the selection, dosage, and duration of antithrombotic agents. After elucidating the clinical benefit of dual antiplatelet therapy (DAPT) using aspirin and clopidogrel [
30], using Ōēź 12 months of DAPT was shown to be beneficial in the secondary prevention of ischemic events [
31], and it has become the standard treatment in the PCI era. Furthermore, new-generation P2Y12 inhibitors were introduced, and some riveting innovations were made, including the risk scoring systems to guide antiplatelet therapy post-PCI, and the evolving concept of ethnic differences regarding the safety and efficacy of these antithrombotic agents (i.e., ŌĆ£Asian paradoxŌĆØ) [
32,
33]. In contrast, the implementation of veno-arterial extracorporeal membrane oxygenation has contributed to the reduction of the mortality rate among patients with AMI [
34]. These advances may well account for the results of our study.
We investigated the clinical impact of hospital visit timing (i.e., off-hour vs. on-hour presentation) on patients with Killip IIIŌĆōIV AMI from the KAMIR-NIH registry. Since the KAMIR-NIH registry is the leading prospective multi-institutional data collection registry of South Korea, we were the first to represent the clinical characteristics and outcomes for patients in the South Korean population according to the time of hospital visit. Furthermore, although comparative studies between off-hour and on-hour targeting patients with STEMI or AMI have been conducted worldwide, there have been no studies on patients with Killip IIIŌĆōIV AMI. To the best of our knowledge, this is the first comparative study of clinical outcomes regarding hospital visit timing in AMI of advanced Killip functional classification. Our study provided new insights into the inconclusive and persistent debate over differences in clinical outcomes between off-hour and on-hour presentation in patients with Killip IIIŌĆōIV AMI, and highlighted that the off-hour hospital presentation did not affect their long-term clinical course.
Although our analysis highlighted that the date and time of hospital visit did not influence the long-term outcomes of AMI with advanced Killip functional classification, our study results must be interpreted with caution due to several limitations. First, the KAMIR-NIH registry included tertiary cardiovascular institutions that accommodated and treated high volumes of patients with AMI. In other words, this registry cannot reflect the real-world features of AMI treatment in small- and medium-sized medical institutions. Moreover, although it was predicted that during off-hours, the availability of interventional cardiologists and support from skilled nursing staff and radiologic technologists will be relatively weakened, and detailed information on them was not included in this study. Hence, it was difficult to generalize the clinical outcomes, including mortality rates and patterns of treatment practice, with respect to all medical institutions. Second, although this study was based only on a prospective, observational registry, it was a non-randomized study. Moreover, it was difficult to conduct a randomized clinical study based on the hospital visit timing in the clinical setting of AMI. Therefore, even though the propensity-score weighing methods such as PSM and IPTW were conducted to minimize the selection bias, a multicenter randomized controlled trial was necessitated. Third, despite a sufficient description of clinical outcomes in the present study, no information on rehospitalization due to heart failure was presented. Fourth, since this is just only a clinical study on the treatment environment of cardiovascular centers in the Republic of Korea, it was still questionable whether it will be translated into a worldwide trend considering the disparities in the multifactorial aspects of the healthcare system and economic status of different countries.
Despite the obvious proposition that timely and effective myocardial reperfusion was the key point in AMI management and our traditional belief that off-hour presentation may be associated with unfavorable clinical outcomes, this study highlighted the lack of significant differences in the long-term outcomes among patients with AMI of advanced Killip functional class regardless of the time of presentation.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement 1
Supplement 1 Print
Print



