INTRODUCTION
Hepatitis B virus (HBV) infection is the most common cause of chronic liver disease in Korea, and the leading cause of liver cirrhosis and hepatocellular carcinoma [1]. After the introduction of the universal HBV vaccination program and nationwide screening, the prevalence of HBV infection has decreased markedly [1]. Korea is now classified as an area of intermediate endemicity for HBV, with an estimated prevalence of approximately 3% in the 2016 Korea National Health and Nutrition Examination Survey (KNHANES) [2]. In Korea, all 19-year-old males are mandated to undergo a physical and medical examination by the Military Manpower Administration (MMA) in accordance with the conscription system. The examination includes body measurements, routine blood tests, and viral hepatitis serology. This system provides a unique opportunity to observe the temporal trends of hepatitis B surface antigen (HBsAg) seroprevalence at a population level according to birth cohorts in Korea. Using this data, we investigated the temporal trends in HBsAg seroprevalence in a cohort of 19-year-old Korean men between 2003 and 2019. In addition, we investigated the changes in metabolic abnormalities over time according to the birth year to identify the prevalence of liver disease over time at a population level in Korea.
METHODS
Study design and subjects
This was a cross-sectional study. A total of 5,355,941 19-year-old Korean males who underwent mandatory medical examinations for conscription between 2003 and 2019 were analyzed in this study. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of Samsung Medical Center (IRB No. 2021-03-003). The requirement for informed consent was waived as we only used de-identified data routinely collected during the examinations.
Study variables
The Korean MMA conducts yearly physical examinations including body measurements (height, weight, and body mass index [BMI]), blood pressure, and routine blood tests (complete blood count, aspartate aminotransferase [AST], alanine aminotransferase [ALT], glucose, and HBsAg) to determine the suitability for military service. We collected data related to HBsAg status since 2003 (year of birth, 1984), AST/ALT levels since 2005 (year of birth, 1986), platelet levels since 2008 (year of birth, 1989), and glucose levels since 2014 (year of birth, 1995).
We defined elevated ALT as a level of > 34 IU/L. BMI values above 23 and 25 were defined as overweight and obesity, respectively. Hypertension was defined by a systolic blood pressure of Ōēź 140 mmHg or diastolic blood pressure of Ōēź 90 mmHg. We used BMI and hypertension as metabolic variables. The fibrosis-4 (FIB-4) index, a simple noninvasive index to predict significant fibrosis, was calculated as [age (years) ├Ś AST (U/L)] / [platelet count (109/L) ├Ś ŌłÜALT (U/L)] [3]. Based on the FIB-4 index, the young men were categorized into those with a FIB-4 index value of < 1.45 and those with a FIB-4 index value of Ōēź 1.45. At this cutoff (1.45), significant fibrosis can be excluded with a high negative predictive value (81.4%) [3].
Statistical analysis
The variables are expressed as the mean ┬▒ standard deviation, median (range), or number (%) as appropriate. Additionally, the differences between continuous and categorical variables were analyzed for statistical significance using the StudentŌĆÖs t test (or Mann-WhitneyŌĆÖs test, if appropriate) and the chi-squared test (or FisherŌĆÖs exact test, if appropriate), respectively.
RESULTS
Changes in HBsAg seroprevalence over time among young men in Korea
HBsAg was positive in 50,003 subjects among 5,355,941 participants, accounting for an overall prevalence of 0.93%. The prevalence of HBsAg according to the year of birth in the study population is shown in Fig. 1. The prevalence of HBsAg declined steadily from 3.2% (year of birth 1984 in the cohort) to 0.2% (year of birth 2000 in the cohort).
Changes in the prevalence of metabolic abnormalities among HBsAg-positive young men in Korea
Next, we analyzed the clinical characteristics of 19,379 HBsAg-positive young men born between 1989 and 2000 as serum platelet levels were available for those who were born after 1989. When the young men were divided into four groups based on 3-year intervals (year of birth 1989ŌĆō1991, 1992ŌĆō1994, 1995ŌĆō1997, and 1998ŌĆō2000), we found a recently increased prevalence in obesity (21.0%, 20.7%, 23.9%, and 28.4% for years 1989ŌĆō1991, 1992ŌĆō1994, 1995ŌĆō1997, and 1998ŌĆō2000, respectively; p < 0.001), overweight status (15.4%, 15.0%, 15.0%, and 18.0% for years 1989ŌĆō1991, 1992ŌĆō1994, 1995ŌĆō1997, and 1998ŌĆō2000, respectively; p = 0.010), and hypertension (6.1%, 6.9%, 6.5%, and 9.1% for years 1989ŌĆō1991, 1992ŌĆō1994, 1995ŌĆō1997, and 1998ŌĆō2000, respectively; p < 0.001) among HBsAg-positive young men. About 30% of the HBsAg-positive young men born between 1998 and 2000 showed elevated ALT levels, whereas those with elevated FIB-4 levels (Ōēź 1.45) constituted a very minor proportion (< 1%).
Changes in the prevalence of metabolic abnormalities among HBsAg-negative young men in Korea
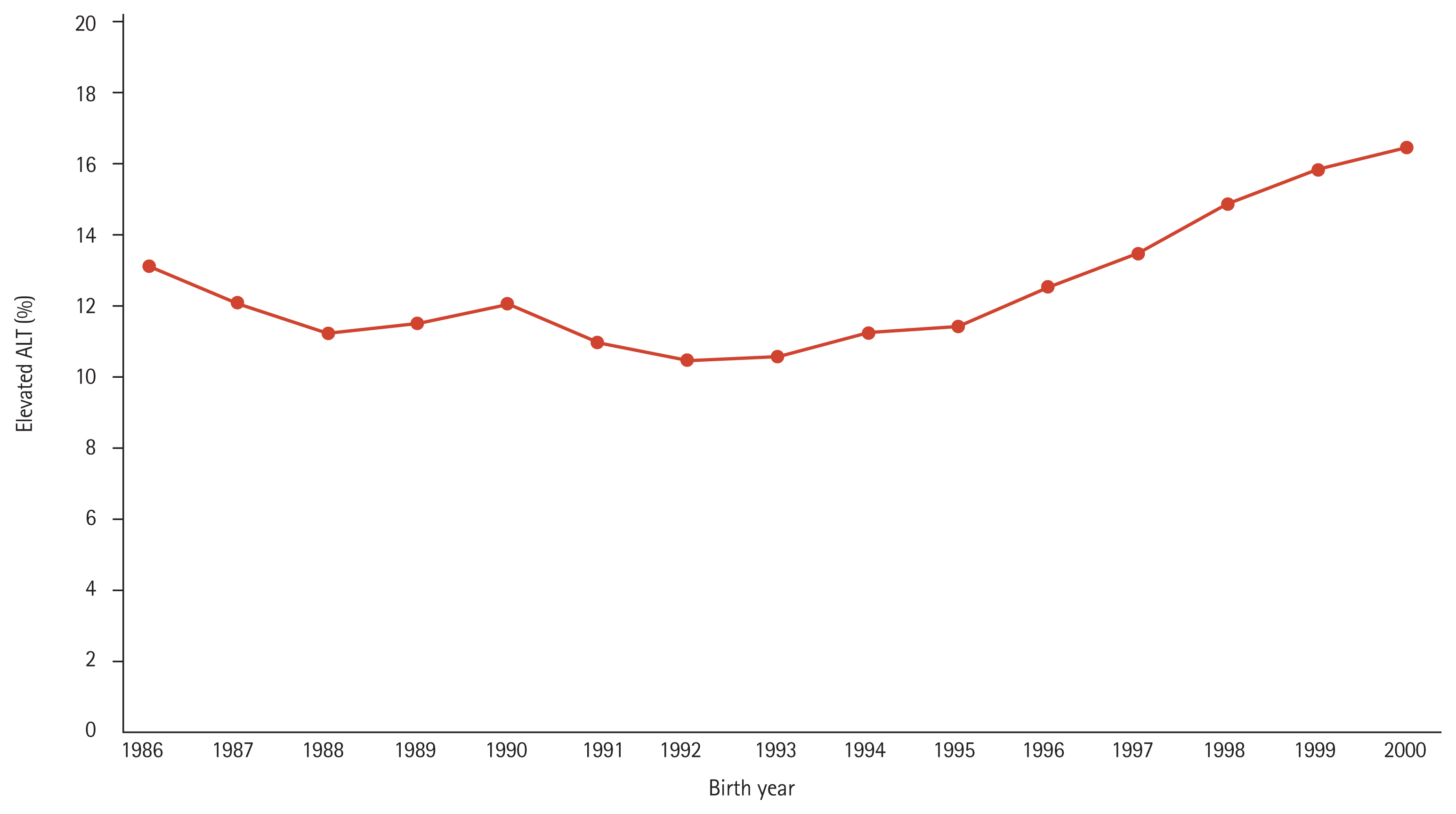
A total of 4,719,729 subjects from the database of draft physical examinations performed by the MMA between 2005 and 2019 were analyzed in the study, as serum ALT levels have been available since 2005. Among them, 589,067 subjects (12.5%) showed elevated ALT levels. The proportion of subjects with elevated ALT levels according to the birth year is shown in Fig. 2. The prevalence of elevated ALT levels was the lowest in subjects born in 1992 (10.5%), and increased each year since 1992, reaching the highest level (16.5%) in 2000.
The baseline characteristics between subjects with normal ALT levels and those with elevated ALT levels were different. Young men with elevated ALT levels showed higher BMI, hypertension, platelet levels, elevated FIB-4 index values, and fasting glucose levels. Among those with elevated ALT levels, 80.8% showed overweight status (13.7%) or obesity (67.1%).
When the young men were divided into four groups of 3-year intervals based on the year of birth (1989ŌĆō1991, 1992ŌĆō1994, 1995ŌĆō1997, and 1998ŌĆō2000), a higher proportion of subjects born in more recent years (1998ŌĆō2000) showed elevated ALT levels (15.7%), overweight status (17.1%), obesity (30.7%), and hypertension (9.6%) than those born in earlier years.
DISCUSSION
In this study, we noticed a decline in HBsAg-positivity over time among young men in Korea. The HBsAg-seropositive rate decreased from 3.19% to 0.18% between those born in 1984 and 2000. Korea has been an endemic area of HBV infection [1]. Several nationwide strategies have been implemented to decrease HBV transmission, including the universal screening of pregnant women for HBV and a universal HBV vaccination program for all infants [1,4]. Several studies have shown a marked decline in HBsAg-positive rates, especially for younger generations in Korea [2,5]. These studies used a nationwide representative cross-sectional sample with stratified, clustered, multistage probability sampling based on geographic area, age, and sex [6,7]. In this study, the participants were composed of all 19-year-old male subjects born between 1984 and 2000 in Korea. Thus, this study accurately reflected the prevalence of hepatitis B in the general population (approximately 300,000 subjects) by birth year in Korea. To our knowledge, this was the first to assess HBsAg seroprevalence in all men by birth year and can be the most reliable reference for HBsAg seroprevalence in Korea.
The prevalence of obesity and hypertension was increased in HBsAg-positive subjects in this study. In a population-based study using the Korean National Insurance Service database, metabolic risk factors (obesity, hypertension, hypercholesterolemia, and diabetes) were associated with an increased risk of hepatocellular carcinoma, cancer, and all-cause mortality in patients with chronic hepatitis B (CHB) [8]. Metabolic abnormalities that co-exist in CHB patients can increase future healthcare burdens in later life. Thus, an active and early intervention to decrease metabolic burden is needed.
Increased metabolic abnormalities were more evident in the HBsAg-negative subjects. The prevalence of obesity and hypertension increased along with the number of those with elevated ALT levels. Non-alcoholic fatty liver disease (NAFLD) is one of the most common causes of elevated liver enzymes [9]. In this study, the HBsAg-negative subjects with elevated ALT levels showed metabolic abnormalities, indicating that NAFLD can be a major cause of elevated ALT levels. The prevalence of NAFLD is rising due to the rapid increase in obesity [10]. A Western study using a large population sample from the National Health and Nutrition Examination Survey (NHANES) 1999 to 2016 survey reported that the prevalence of possible NAFLD among United States adolescents had risen substantially over the past two decades [11]. As Korea is also experiencing the Westernization of diets and lifestyles, the prevalence of NAFLD among Koreans is likely to increase over time. Kang et al. [12] showed that the prevalence of NAFLD in Korean men had increased rapidly with a linear trend from 1998 to 2017 and will likely approach 40% in 2030. This study showed that liver disease associated with metabolic abnormalities will become a significant health threat.
This study had some limitations. First, this study included only men since we used data from MMA examinations. Further data is needed to determine whether the changes seen in this study are similar in women. Second, we used data generated for MMA examinations. Hence, several important variables (e.g., diabetes, dyslipidemia, presence of hepatic steatosis, and the use of medications) to assess metabolic abnormalities were missing. Nonetheless, this population-based study provides compelling evidence for a decline in HBsAg seroprevalence and an increase in metabolic abnormalities over time.
In summary, this study provides population-based data on HBsAg seroprevalence and metabolic variables. This epidemiologic data can not only provide information on the changing epidemiology of liver disease but also serve as a reliable reference for planning public health strategies.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





