 |
 |
| Korean J Intern Med > Volume 38(2); 2023 > Article |
|
Abstract
Background/Aims
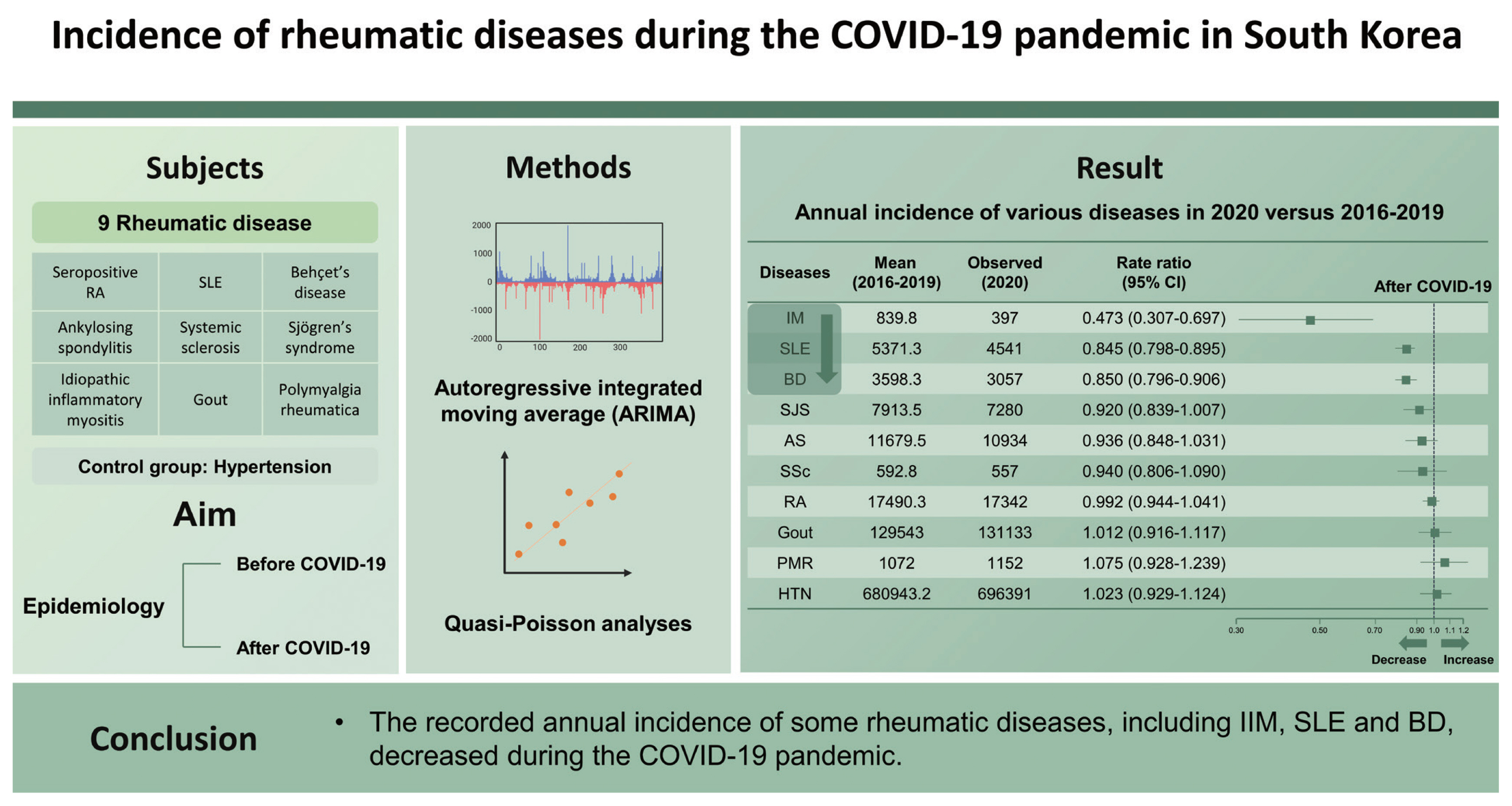
The recent coronavirus disease 2019 (COVID-19) pandemic has been associated with changes in the epidemiology of not only infectious diseases but also several non-infectious conditions. This study investigated changes in the recorded incidence of various rheumatic diseases during the COVID-19 pandemic.
Methods
The number of patients for each disease from January 2016 to December 2020 was obtained from the Korean Health Insurance Review and Assessment Service database. We compared the incidence of nine rheumatic diseases (seropositive rheumatoid arthritis, systemic lupus erythematosus [SLE], idiopathic inflammatory myositis [IIM], ankylosing spondylitis [AS], systemic sclerosis, Sjögren’s syndrome, Behçet’s disease [BD], polymyalgia rheumatica, and gout) and hypertensive diseases to control for changes in healthcare utilisation before and after the COVID-19 outbreak. The disease incidence before and after the COVID-19 outbreak was compared using the autoregressive integrated moving average (ARIMA) and quasi-Poisson analyses.
Results
Compared with the predicted incidence in 2020 using the ARIMA model, the monthly incidence of SLE, BD, AS, and gout temporarily significantly decreased, whereas other rheumatic diseases and hypertensive diseases were within the 95% confidence interval (CI) of the predicted values in the first half of 2020. In age- and sex-adjusted quasi-Poisson regression analysis, the annual incidences of IIM (rate ratio [RR], 0.473; 95% CI, 0.307 to 0.697), SLE (RR, 0.845; 95% CI, 0.798 to 0.895), and BD (RR, 0.850; 95% CI, 0.796 to 0.906) were significantly decreased compared with those in the previous 4 years.
Autoimmune inflammatory rheumatic diseases (AIIRDs) mainly affect the musculoskeletal system and connective tissues due to altered immune regulation [1]. Several diseases, including rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), ankylosing spondylitis (AS), Behçet’s disease (BD), Sjögren’s syndrome (SjS), systemic sclerosis (SSc), idiopathic inflammatory myositis (IIM), polymyalgia rheumatica (PMR), and gout are included in this classification [2]. Infection is often considered a major trigger for AIIRD [3]. In December 2019, a novel coronavirus infection (coronavirus disease 2019 [COVID-19]) was identified, and it has rapidly spread globally [4]. Nonpharmaceutical interventions (NPIs) for COVID-19 have been reported to reduce the prevalence of Kawasaki disease and the rates of hospitalisation for respiratory and chronic lung diseases [5–7]. Conversely, the COVID-19 pandemic has been associated with an increased incidence of gestational diabetes mellitus, perforated appendicitis, depression and anxiety [8–10].
In the light of this and the potential mechanisms by which COVID-19 could influence the incidence of AIIRDs, this study aimed to determine if the COVID-19 pandemic was associated with changes in the reported incidence of AIIRDs. We extracted the incidence of AIIRDs in South Korea during the COVID-19 pandemic from a countrywide healthcare claims database and compared it with data from the previous 4 years.
The present work is a retrospective study comparing the incidences of 10 diseases before and after the COVID-19 outbreak. The number of outpatients with these diagnoses from January 2016 to December 2020 was obtained from the Korean Health Insurance Review and Assessment Service database in South Korea. All of the recorded diagnoses were based on the International Statistical Classification of Diseases and Related Health Problems, 10th revision. Our study included nine rheumatic diseases and one common non-rheumatic disease to control for the change in healthcare utilisation. The rheumatic diseases were seropositive RA (M05), SLE (M32), IIM (M33), AS (M45), SSc (M34), SjS (M35.0), BD (M35.2), PMR (M35.3), and gout (M10), and the non-rheumatic disease was a group of hypertensive diseases (I10–I15). The number of new cases per month was used to calculate the incidence of the disease. New patients were defined as those who had not been registered with the applicable diagnosis in the previous 5 years.
Prediction analysis was conducted using an autoregressive integrated moving average (ARIMA) to determine changes in disease incidence associated with the COVID-19 outbreak. The ARIMA model was fitted to the period before the COVID-19 outbreak from 2016 to 2019 and anticipated the incidence of diseases with confidence intervals (CIs) of 80% and 95%. It was used to compare the monthly incidence of each disease observed in 2020. Visual comparison of the annual and monthly trends as well as the monthly differences in incidence of each disease was performed using the ARIMA model. The age- and sex-adjusted annual incidence rate ratios (RRs) of each disease before and after the COVID-19 outbreak were estimated using quasi-Poisson regression analysis. Parameter selection for the ARIMA model and quasi-Poisson analysis were performed using the ‘auto.arima’ function in the forecast package and the ‘glm’ function in the stats package of R software (R Foundation for Statistical Computing, Vienna, Austria), respectively. p values <0.05 were considered statistically significant. All analyses were conducted using R software version 4.1.0.
This study conformed to the ethical guidelines of the Declaration of Helsinki. The need for informed consent was waived by the Institutional Review Board (IRB) because of the retrospective nature of the study using a database. The waiver from the IRB was certified by the Asan Medical Center (No. 2021-1031).
Fig. 1 represents the annual and monthly trends for each disease based on the monthly aggregated incidence data from 2016 to 2020 and the monthly predicted incidence for 2020 using the ARIMA model. During the first half of 2020, the early phase of the COVID-19 outbreak, the monthly incidences of SLE, BD, AS, and gout temporarily decreased dramatically compared with the predicted incidences of those in 2020 (Fig. 1). Conversely, the monthly incidences of SjS, SSc, PMR, RA, and hypertensive diseases during the same period were within the 95% CI of the predicted values using the ARIMA model. Although the monthly incidence of IIM was within the 95% CI of the ARIMA model’s predicted value, the actual incidence in 2020 was much lower than that of the previous 3 years (Fig. 1E).
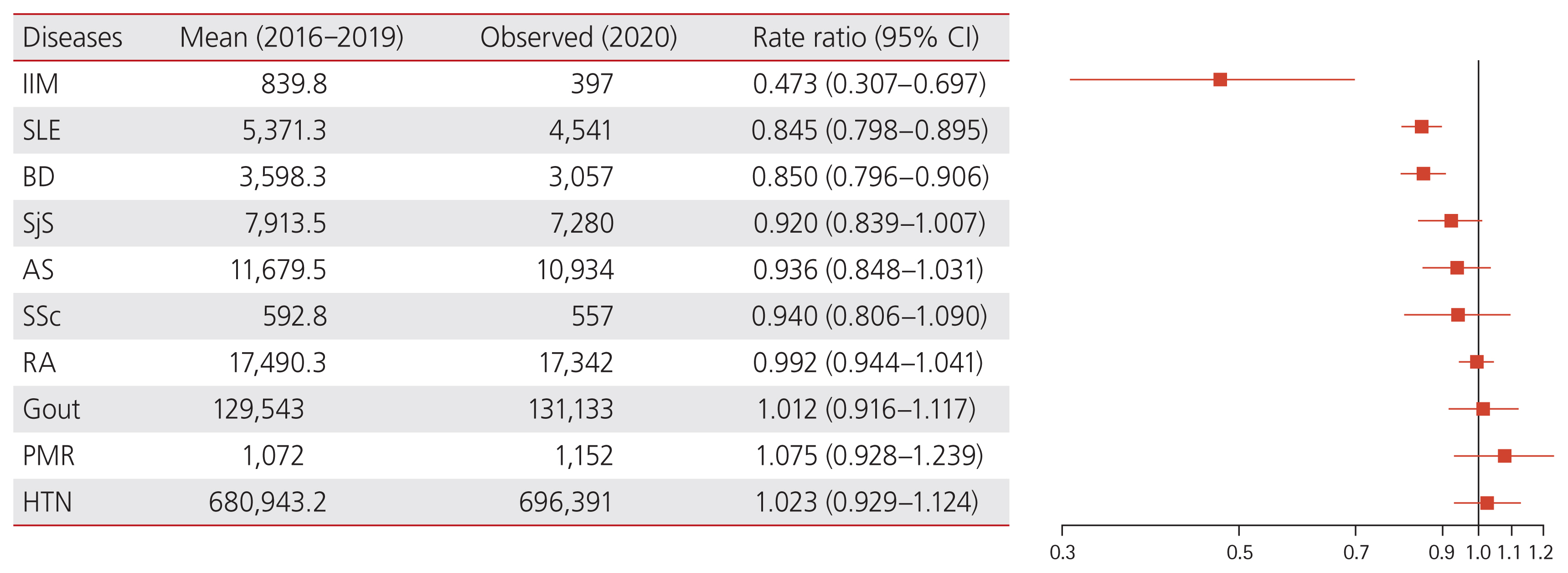
Fig. 2 presents a comparison of the annual incidence of each disease from 2016 to 2019 and the incidence of each disease in 2020 according to the age- and sex-adjusted quasi-Poisson analysis. The disease incidences in 2020 of IIM (RR, 0.473; 95% CI, 0.307 to 0.697), SLE (RR, 0.845; 95% CI, 0.798 to 0.895), and BD (RR, 0.850; 95% CI, 0.796 to 0.906) were significantly decreased compared with that of the previous 4 years, whereas the annual incidence of gout (RR, 1.012; 95% CI, 0.916 to 1.117), PMR (RR, 1.075; 95% CI, 0.928 to 1.239), and hypertensive diseases (RR, 1.023; 95% CI, 0.929 to 1.124) exhibited an increasing trend that failed to reach statistical significance.
South Korea initially gained attention in terms of the global COVID-19 response after the first COVID-19 patient was identified on January 20, 2020 [11]. In 2020, the number of cumulative confirmed COVID-19 cases in South Korea was 1.3 per thousand persons, which was much lower than that in other nations like the United States and the United Kingdom [12]. Nonetheless, the annual incidence of IIM, SLE, and BD decreased during the COVID-19 pandemic in 2020, according to this nationwide survey.
Several contributing factors can explain the reduction in the incidence of some rheumatic diseases during the COVID-19 pandemic. First, the incidence of rheumatic diseases may have temporarily decreased due to the decrease in healthcare utilisation driven by concerns about COVID-19 infection. During the COVID-19 pandemic in the United States, hospital admissions and emergency department visits were low, presumably related to a fear of COVID-19 infection [13–15]. A recent study demonstrated that the number of breast cancer screening, diagnosis and surgery cases decreased with the decrease in hospital visits, whereas the proportion of patients diagnosed with advanced breast cancer increased [11]. Essentially, according to the statistics of the Korean Health Insurance Review and Assessment Service, the total number of patients in 2020 was significantly lower than the average of the previous 4 years [16]. The monthly incidence of numerous diseases in the first half of 2020, the early phase of the COVID-19 pandemic, was much lower than that in the second half in the ARIMA analysis. It could be interpreted that the marked decrease in hospital visits in the early phases of the COVID-19 pandemic had been complementarily reversed in the second half of 2020. However, because the annual incidence of gout and hypertensive diseases did not significantly decrease in 2020 compared with before the COVID-19 pandemic, it is difficult to attribute the decrease in the annual incidence of IIM, SLE, and BD to a reduction in healthcare utilization. Second, South Korea has been thoroughly practising personal hygiene and the universal use of masks since the early days of the COVID-19 outbreak [17]. Furthermore, it strictly implemented social distancing during 2020 [18]. According to reports, these COVID-19 NPIs reduced the incidence of Kawasaki disease and the rates of hospitalisation due to respiratory and chronic lung diseases in South Korea [5,6,19]. A study using German national surveillance data also reported a decrease of respiratory and blood-borne infectious diseases, including measles and hepatitis C virus, owing to the implementation of NPIs during the COVID-19 pandemic [7]. Various viral infections are implicated in the development of autoimmune disorders through molecular mimicry and other mechanisms [3]. In particular, Epstein–Barr and hepatitis C viruses may promote uncontrolled autoantibody synthesis, resulting in AIIRDs [20]. Thorough implementation of the NPIs to prevent the spread of COVID-19 in South Korea reduced the incidence of several viral infections, which may have affected the incidence of AIIRDs.
The present study has some limitations. First, the National Health Insurance claims database lacked accurate clinical information on individual patients, such as laboratory and radiographic findings as well as lifestyle factors. Second, the disorders were identified using the registered diagnosis code, which may not accurately reflect the disease severity. Third, 1 year is too short to sufficiently evaluate the changes in the incidence of various chronic diseases, including most rheumatic diseases, in association with changes in societal and environmental factors. Thus, longer-term studies in more countries are needed in the future to better elucidate the potential link between the COVID-19 pandemic and various chronic diseases. The main strength of this study is that it is the first to report a significant decrease in the annual incidence of some rheumatic diseases during the COVID-19 pandemic, based on a nationwide claims database.
In conclusion, this study showed a significant decrease in the incidence of IIM, SLE, and BD during the COVID-19 pandemic in 2020, suggesting a potential link between societal and environmental changes associated with the COVID-19 pandemic, especially NPIs, and a decrease in the incidence of certain rheumatic diseases.
1. The recorded annual incidence of idiopathic inflammatory myositis, systemic lupus erythematosus, and Behçet’s disease decreased during the coronavirus disease 2019 (COVID-19) pandemic.
2. Limited use of medical facilities and nonpharmaceutical intervention application might have influenced the recorded autoimmune inflammatory rheumatic disease incidence.
Acknowledgments
This work was supported by grant to Yong-Gil Kim from the Asan Institute for Life Sciences (grant number: 2021IL0015).
Figure 1
The monthly incidence and predicted incidence of (A) systemic lupus erythematosus, (B) Behçet’s disease, (C) ankylosing spondylitis, (D) Sjögren’s syndrome, (E) idiopathic inflammatory myositis, (F) rheumatoid arthritis, (G) systemic sclerosis, (H) polymyalgia rheumatica, (I) gout, and (J) hypertensive diseases using the autoregressive integrated moving average (ARIMA) model. The blue line denotes the monthly predicted incidence for 2020 using the ARIMA model. Blue and grey shades denote the 80% and 95% confidence intervals of the predicted incidence.
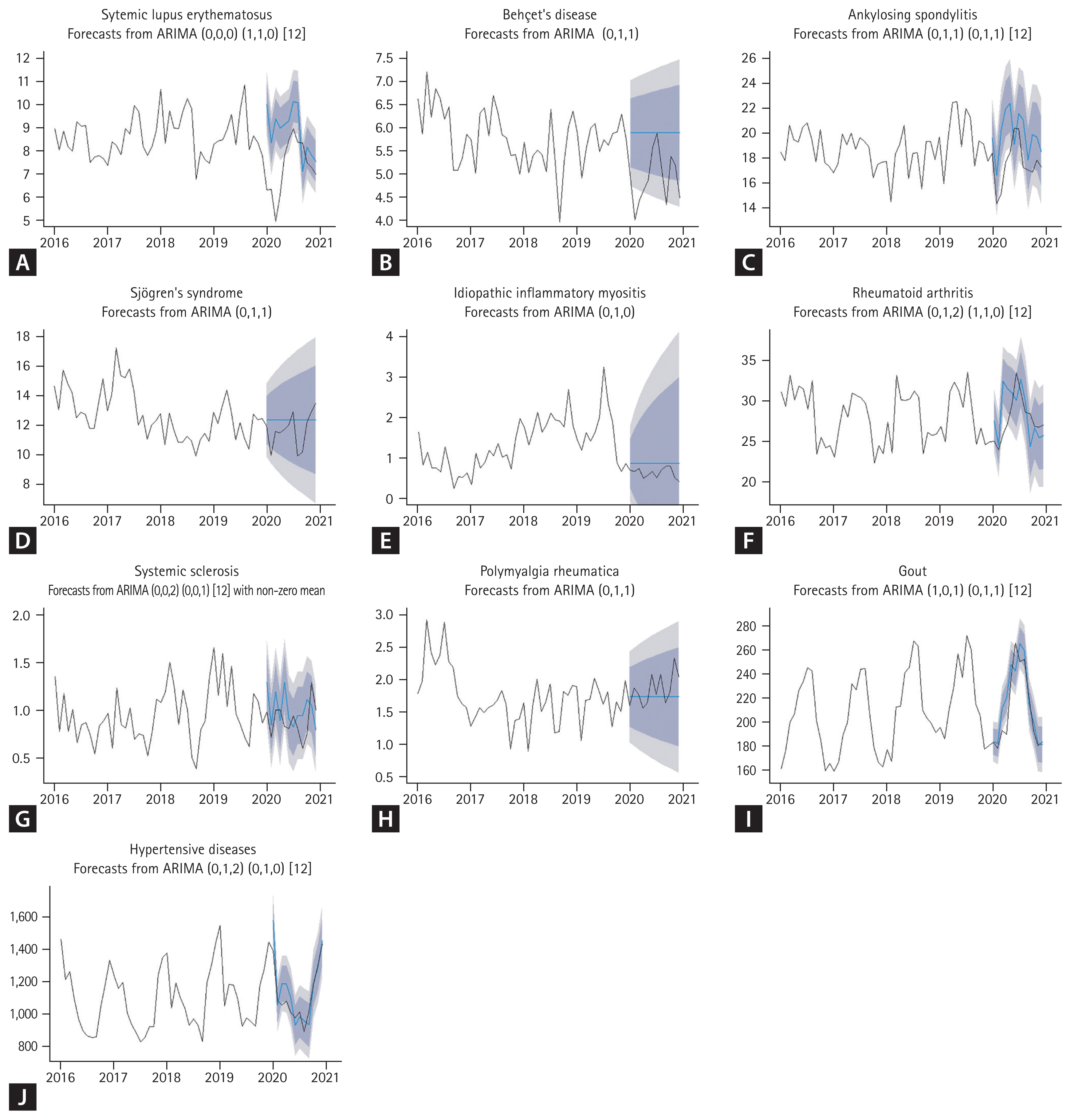
Figure 2
The annual incidence of various diseases in 2020 versus 2016–2019. CI, confidence interval; IIM, idiopathic inflammatory myositis; SLE, systemic lupus erythematosus; BD, Behçet’s disease; SjS, Sjögren’s syndrome; AS, ankylosing spondylitis; SSc, systemic sclerosis; RA, rheumatoid arthritis; PMR, polymyalgia rheumatica; HTN, hypertensive diseases.
REFERENCES
1. Seo YB, Moon SJ, Jeon CH, et al. The practice guideline for vaccinating korean patients with autoimmune inflammatory rheumatic disease. Infect Chemother 2020;52:252–280.




2. Kim H, Cho SK, Kim JW, et al. An increased disease burden of autoimmune inflammatory rheumatic diseases in Korea. Semin Arthritis Rheum 2020;50:526–533.


3. Rojas M, Restrepo-Jimenez P, Monsalve DM, et al. Molecular mimicry and autoimmunity. J Autoimmun 2018;95:100–123.


4. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506.



5. Huh K, Kim YE, Ji W, et al. Decrease in hospital admissions for respiratory diseases during the COVID-19 pandemic: a nationwide claims study. Thorax 2021;76:939–941.



6. Kang JM, Kim YE, Huh K, et al. Reduction in Kawasaki disease after nonpharmaceutical interventions in the COVID-19 era: a nationwide observational study in Korea. Circulation 2021;143:2508–2510.



7. Ullrich A, Schranz M, Rexroth U, et al. Impact of the COVID-19 pandemic and associated non-pharmaceutical interventions on other notifiable infectious diseases in Germany: an analysis of national surveillance data during week 1-2016 – week 32-2020. Lancet Reg Health Eur 2021;6:100103.



8. Zanardo V, Tortora D, Sandri A, Severino L, Mesirca P, Straface G. COVID-19 pandemic: impact on gestational diabetes mellitus prevalence. Diabetes Res Clin Pract 2022;183:109149.



9. Motazedian G, Aryanpoor P, Rahmanian E, et al. Incidence of pediatric perforated appendicitis during the COVID-19 pandemic; a systematic review and meta-analysis. Arch Acad Emerg Med 2021;10:e3.


10. Hajek A, Sabat I, Neumann-Bohme S, et al. Prevalence and determinants of probable depression and anxiety during the COVID-19 pandemic in seven countries: longitudinal evidence from the European COvid Survey (ECOS). J Affect Disord 2022;299:517–524.



11. Kang YJ, Baek JM, Kim YS, et al. Impact of the COVID-19 pandemic on the diagnosis and surgery of breast cancer: a multi-institutional study. J Breast Cancer 2021;24:491–503.




12. Our World in Data. Daily new confirmed COVID-19 cases per million people [Internet] Our World in Data, 2022. [cited 2022 Sep 1]. Available from: https://ourworldindata.org/explorers/coronavirus-data-explorer?zoomToSelection=true&time=2020-03-01..2020-12-31&facet=none&pickerSort=desc&pickerMetric=new_cases_smoothed_per_million&Metric=Confirmed+cases&Interval=7-day+rolling+average&Relative+to+Population=true&Color+by+test+positivity=false&country=KOR~USA~GBR
.
13. Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood) 2020;39:2010–2017.



14. Giannouchos TV, Biskupiak J, Moss MJ, Brixner D, Andreyeva E, Ukert B. Trends in outpatient emergency department visits during the COVID-19 pandemic at a large, urban, academic hospital system. Am J Emerg Med 2021;40:20–26.



15. Nourazari S, Davis SR, Granovsky R, et al. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am J Emerg Med 2021;42:203–210.



16. Healthcare Bigdata Hub. Number of patients per year [Internet] Wonju (KR): Health Insurance Review & Assessment Service, 2020. [cited 2022 Sep 1]. Available from: http://opendata.hira.or.kr/op/opc/olapHthInsRvStatInfo.do
.
17. COVID-19 National Emergency Response Center, Epidemiology & Case Management Team, Korea Centers for Disease Control & Prevention. Contact transmission of COVID-19 in South Korea: novel investigation techniques for tracing contacts. Osong Public Health Res Perspect 2020;11:60–63.




18. Yun HE, Ryu BY, Choe YJ. Impact of social distancing on incidence of vaccine-preventable diseases, South Korea. J Med Virol 2021;93:1814–1816.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



