Bacteremia With Nontyphi Salmonella and Therapeutic Implication
Article information
Abstract
Objectives:
The recent decades witnessed the increased incidence of bacteremia with nontyphi Salmonella, especially in patients with underlying diseases. To evaluate clinically the patients with bacteremia by nontyphi Salmonella, we investigated the clinical records of the patients.
Methods:
Retrospecitive study was performed on 30 cases of bacteremia with nontyphi Salmonella admitted to Soon Chun Hyang University Hospital from 1987 to 1993, and we analyzed with regard to age distribution, underlying diseases, clinical presentation and fatality.
Results:
Children below 2 years of age were seven patients and patients over 55 years of age were 8 patients. The male to female ratio was 3:2. Only five cases were nosocomially acquired. More than two-thirds (21 patients) had no discernible other illness at the time of their bacteremia. A quarter of the patients presented without gastrointestinal manifestation. There were four deaths in the 30 patients with nontyphi Salmonella septicemia (13.3%).
Conclusions:
We investigated the clinical characteristics of 30 cases of non-typhi Salmonella bacteremia, which has a relatively high incidence nowadays while, to the contrary. Salmonella typhi trends toward being on the decrease in Korea.
INTRODUCTION
Infections caused by any salmonella species other than S. typhi are termed nontyphi salmonellosis1–5). These infections can present as acute diarrhea, a septicemic syndrome, focal abscess, meningitis, osteomyelitis, endocarditis, mycotic aneurysm or can be asymptomatic. Nontyphi Salmonella species can produce a clinical syndrome characterized by prolonged episodes of intermittent fever, anorexia and persistent bacteremia. Intestinal complaints and concomitant positive stool cultures are uncommon in these patients4,5). An increased incidence of Salmonella bacteremia has been associated with immunodeficiencies in patients with hepatic cirrhosis, collagen vascular disease, leukemias, lymphomas and other neoplastic syndromes1–5). Nontyphi salmonellosis and typhoid fever are major urban health problems along the western coast of South America4,5) as well as in Asia. Salmonellosis has been a common and important infectious disease in Korea1–3), too.
We analyzed 30 patients with bacteremia by Nontyphi Salmonella treated at Soon Chun Hyang University Hospital during the period from 1987 till 1993.
PATENTS AND METHODS
We reviewed retrospectively the clinical records of all patients who presented with bacteremia by non-typhi Salmonella in this hospital from 1987 till 1993. To correlate data, we used a protocol in which we evaluated, in detail, the following points: Acquisition of the infection: we classified as nosocomially acquired those infections whose symptoms began after more than 48hours of hospitalization and, as community acquired, those where the patient presented with symptoms on admission or within 48hours. Evaluation of treatment according to the following criteria: appropriate when the isolate was sensitive in vitro to at least one of the antibiotics administered parenterally for a minimum of ten days; incorrect when none of the previous criteria were fullfilled. We classified as untreated those who received symptomatic treatment without the use of antimicrobial agents.
Evolution: we evaluated complications of the bacteremia in the form of septic metastases and mortality, with respect to direct relationship to the bacteremia.
Statistical analyses: either the chi-square test or the Fisher’s exact test was used to analyze contingency tables.
RESULTS
Among 30 cases of bacteremia with nontyphi Salmonella were 18 males and 12 females. Children below 2 years of age were seven patients (23.3%) and patients over 55 years of age were 8 patients (26.7%). In 1993, bacteremias with nontyphi Salmonella represented 4% of all bacteremias diagnosed in this hospital. Five bacteremias (16.7%) were nosocomially acquired and 25(83.3%) were community acquired. Three out of 5 patients with nosocomial infection had underlying illnesses; chronic renal failure in 2, hepatocellular carcinoma in one. The latter patient developed acute gastroenteritis during the course of bacteremia and the source was the gastrointestinal tract. In the remaining one, no underlying disease was identified. Nosocomial infections occurred separately at intervals of 5 to 10 months.
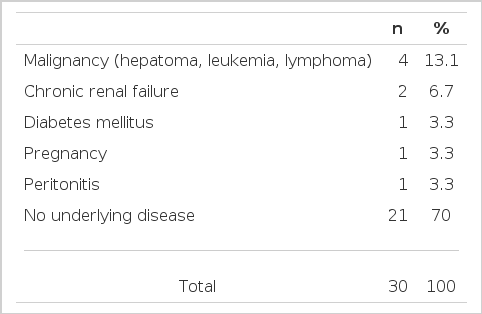
Nine patients (30%) had underlying diseases, 21 (70%) had no discernible other disease at the time of their bacteremia. Underlying diseases are presented in Table 1. Underlying disease were more frequent (85.7%) in patients with unknown portal of entry than in those whose source of infection was acute gastroenteritis (13.0%) (p < 0.05)
No cases are presented in the course of AIDS. This finding is in contrast to the report of other European or American authors.
Fever, diarrhea, chill, abdominal pain, nausea and vomiting were present in 53.3%, 50%, 30%, 30% and 26.7% of patients with bacteremia by nontyphi Salmonella at admission, respectively. The portal of entry was gastrointestinal tract in 23 patients (76.7%) judged by clinical decision, including microbiologic investigation. In four patients this origin was confirmed by the presence of the same strain of Salmonella in the stool culture. However, in seven patients(23.3%), the source of infection was not an episode of acute gastroenteritis. Leukopenia was seen in 13.3% of the cases with bacteremias with nontyphi Salmonella.
S. enteritidis was the bacteria isolated in 12 patients(40%), in 11(36.7%) S. paratyphi A, while in seven(23.3%) group B Salmonella.
In four cases (13.3%) ampicillin resistant strains were isolated. Two strains among them were resistant to both ampicillin and chloramphenicol. Other two strains were resistant to chloramphenicol and two strains to piperacillin. All isolates were susceptible to third generation cephalosporins, trimethoprim-sulfamethoxazole and fluoroquinolones, although the last two were not tested in all isolates. 20 isolates (67.7%) were susceptible to all the antimicrobials tested at the time of bacteremia.
Antibiotic therapy was administered in 28 patients(93.3%) of which 26(92.9%) were considered appropriate. Three patients(10%) presented clinical findings compatible with septic shock, three patients died of illnesses directly related to the bacteremia and one patient died of underlying disease (Table 2). No case with DIC or ARDS was found.
We found the incidence of bacteremia with nontyphi Salmonella trended toward being on the increase, as compacted with typhoid fever (Fig. 1).
DISCUSSION
Salmonellae are gram-negative bacilli of the family Entrerobacteriaceae. Isolation of nontyphi Salmonella from blood is relatively uncommon; frequencies of 5–10% were noted in two large reviews on salmonellosis6,7). However, in several reviews on salmonellosis in patients with neoplastic disease, an incidence of septicemia of up to 35% was noted, and risk factors were found to include leukemia, lymphoma, steroid therapy, cytotoxic therapy, prior surgery (especially gastrointestinal) and radiation therapy6–8). The main source of nontyphi Salmonella infection is animals, although transmission also occurs form person to person7). In our series, nosocomial infections occurred separately at intervals of 5 to 10 months and it is difficult to make a clinical or epidemiologic relevance among them, which was to be explained by outbreak.
Although nontyphi Salmonella bacteremia usually presents as a mild gastrointestinal illness, it has a wide spectrum of manifestations, especially under certanin circumstances; these manifestations include life-threatening septicemia, indolent infections and focal infections of nearly every organ in the body8). Risk factors for precipitation of overt and sometimes unusual manifestations of nontyphi Salmonella infection include underlying malignancy, corticosteroid and cytotoxic therapy, collagen vascular disease, alcoholism, liver disease, sickle-cell disease and other hemolytic illness, previous surgery and prior antibiotic therapy6–10). AIDS also an important risk factor for the recent two decades11–13). Cellular immunity plays an important role in the control of infection by nontyphi Salmonella. Although in our series no case of bacteremia with nontyphi Samonella presented in AIDS patients, other researchers published the higher frequency of bacteremias in these patients, as well as with an astounding increase in the number of AIDS patients.
There is bimodal age distribution of salmonella bacteremia as there is for salmonella infection in general6,7). We found the peak age incidence was first decade(30%) and 8 cases were over 7th decade(26.7%). The two group consisted of more than half of all patients. Nine years ago the peak age incidence of salmonellosis was between second and fourth decade3). It means that the peak incidence is active age but our data are different, probably because there were enormous alterations in every aspect of Korean society. Most of the children had no underlying disease, and presented no complications or mortality. No difference was reported between antibiotic treated group and untreated group in pediatric patients. However, in our series, there were not the same results. The low mortality of bacteremias by nontyphi Salmonella and the fact that many episodes are self-limited make it difficult to evaluate therapeutic regimens. In the light of these results, the question arises as to whether it is necessary to treat all patients with nontyphi Salmonella bacteremia with parenteral antibiotics.
Future prospective studies should define which patients must be treated, the type of antimicrobial agents to be used and the duration and the means of administration.
Antimicrobial treatment should be maintained for two weeks if the patients show indications and in the case of localized infection, a period of four to six weeks is recommended. Patients in a stable clinical state may be treated orally or with three to five day courses of parenteral antibiotics, subsequently continued with oral treatment, needless to say, always under strict medical supervision.
Our data depicted that the incidence of bacteremia with nontyphi Salmonella, at present, became higher than that in past, and which probably suggests the widespread alteration of the socioeconomicstatus in Korea.