The Effects of QRS Duration and Pacing Sites on the Acute Hemodynamic Changes during Right Ventricular Pacing
Article information
Abstract
Background
Has been reported that patients exhibiting prolonged paced QRS duration tend to have more serious heart disease, and the paced QRS duration can be an effective indicator of impaired left ventricular function. However, the acute and chronic hemodynamic effects of paced QRS duration and pacing sites during right ventricular (RV) pacing remain unknown.
Methods
A total of 14 patients who underwent electrophysiologic study for paroxysmal supraventricular tachycardia were examined. RV pacing was performed at 10 different sites with cycle lengths of 600 ms and 500 ms utilizing a 6-7F deflectable quadripolar electrode catheter. Systolic, diastolic, and mean blood pressures during pacing were measured once the blood pressure was stabilized.
Results
During RV pacing, blood pressures (systolic/diastolic/mean) decreased. The change of post-pacing QRS duration and pre-pacing the systolic blood pressure (SBP) were greater in the group with paced QRS duration. The differences overall were greater than 140 ms. The SBP decrease during pacing was larger in the group exhibiting paced QRS duration of greater than 140 ms. The SBP decrease during pacing showed relation to QRS duration during pacing (r=0.500, p=0.001), the change of QRS duration post-pacing (r=0.426, p=0.001), and SBP during sinus rhythm (r=0.342, p=0.001) on linear correlation analysis. The pacing site, on the other hand, did not affect acute hemodynamic changes during pacing.
Conclusion
Ventricular pacing of less than 40 ms at the area of paced QRS duration is recommended.
INTRODUCTION
Intraventricular conduction defects, which are manifested as increased QRS duration, are seen frequently in patients with left ventricular dysfunction and have an adverse effect on left ventricular systolic and diastolic function1, 2). Also, conduction disturbances are associated with poor short- and long-term prognoses of patients exhibiting acute myocardial infarction3-5). While the mechanism which prolonged QRS duration is allied with increasing risk of death is not clear in patients with acute myocardial infarction, multiple physiologic factors, including increased left ventricular muscle mass6), myocardial fibrosis6), increased area of necrosis7), participation of the conduction system in the ischemic area, and poor metabolic states which slow conduction8) might be involved.
Sumiyoshi et al9). reported that patients with an extended paced QRS duration tend to exhibit more serious heart disease, and the paced QRS duration can be an invaluable indicator of impaired left ventricular function. In addition, several clinical studies have determined that correction of conduction defects by multisite ventricular pacing has caused marked improvement in left ventricular function and in overall hemodynamic performance10, 11).
Nonetheless, little data are available about the effects of paced QRS duration and pacing sites on hemodynamic changes in relation to right ventricular (RV) pacing. To counter this lack of information, our study aimed to determine the optimal pacing site which would be able to minimize hemodynamic deterioration in patients equipped with permanent pacemakers.
MATERIALS AND METHODS
Subjects
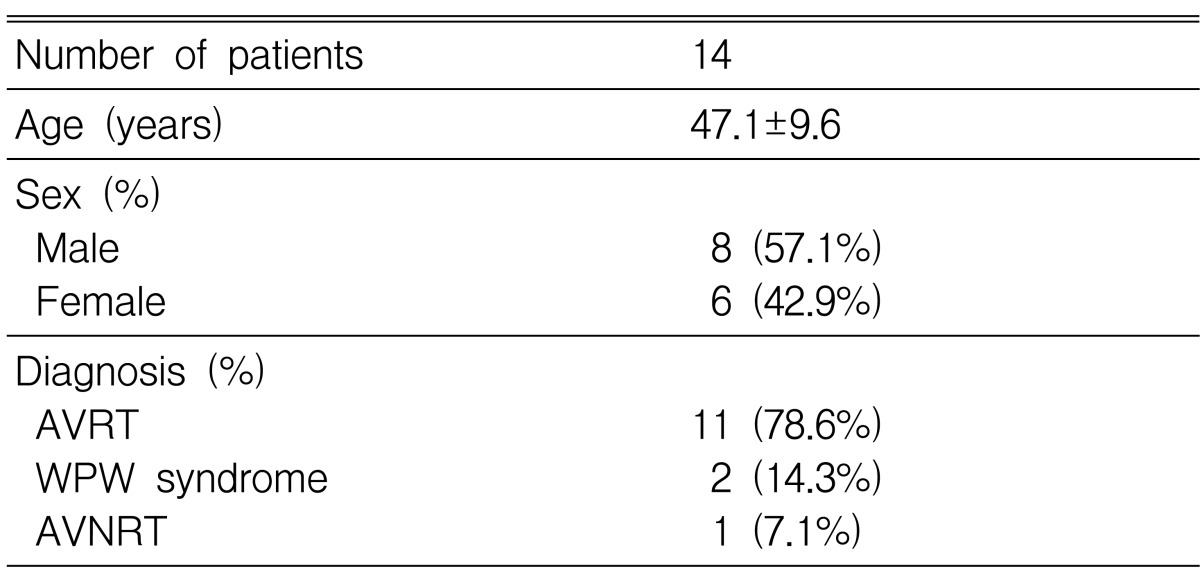
A total of 14 patients who underwent electrophysiologic study for paroxysmal supraventricular tachycardia at Chonnam National University Hospital between February 2002 and April 2003 were examined. None of the patients exhibited signs of structural heart disease.
Methods
RV pacing was carried out at 10 distinctive sites at cycle lengths of 600 ms and 500 ms using a 6-7F deflectable quadripolar electrode catheter (Livewire, St. Jude Medical, Minneapolis, MN, USA) This was done subsequent to successful radio frequency catheter ablation for paroxysmal supraventricular tachycardia. RV pacing was sustained for about 15 seconds after the stabilization of femoral arterial pressure during pacing. Paced QRS duration was measured after stabilization of blood pressure during pacing, as were systolic, diastolic, and mean blood pressures. The overall pacing figure at 10 separate sites was 116. Hemodynamic change was then compared between the group of paced QRS duration of less than 140 ms and the group of paced QRS duration of more than 140 ms during RV pacing. The factors related to the decrease in blood pressure during RV pacing were then examined.
Statistics
In order to perform the statistical analyses, the unpaired t-test, Chi-square test, and multiple logistic regression analysis were executed using SPSS-PC 11.0 (Statistical package for the social sciences, SPSS Inc. Chicago, IL, U.S.A.) and MS Windows®. The results were designated as mean±standard deviation. A value of p less than 0.05 was judged to be significant.
RESULTS
Clinical characteristics
Of all of the participants of the study, the mean age was 47.1±9.6 years and the percentage of male participants was 57.1%. The type of tachycardia diagnosed upon electrophysiologic study was atrioventricular reentrant tachycardia in 78.6% of participants, Wolff-Parkinson-White syndrome in 14.3%, and atrioventricular nodal reentrant tachycardia in 7.1% (Table 1).
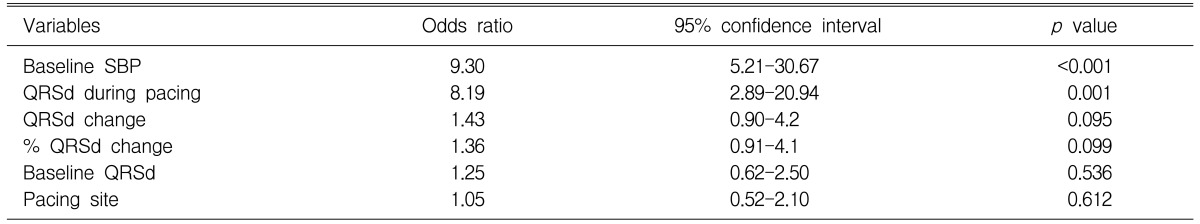
The changes of blood pressure and QRS duration according to the pacing site
The mean systolic blood pressures (SBPs) prior to pacing and during pacing were 146±31 mmHg and 128±33 mmHg, respectively. This accounts for the mean decrease of SBP during pacing of 18±13 mmHg. The decrease of SBP during pacing was striking at the upper septum (27±7 mmHg) and nominal at the right ventricular outflow tract (11±10 mmHg) (Table 2).
Changes of systolic blood pressure and QRS duration during right ventricular pacing according to pacing site
The mean QRS intervals prior to pacing and during pacing were 66±11 ms and 140±13 ms, respectively. A mean increase in QRS duration during pacing of 74±21 ms was exhibited. The increase in QRS duration during pacing was marked when observed at the upper septum (97±17 ms) and minimal at para-His (61±15 ms) (Table 2).
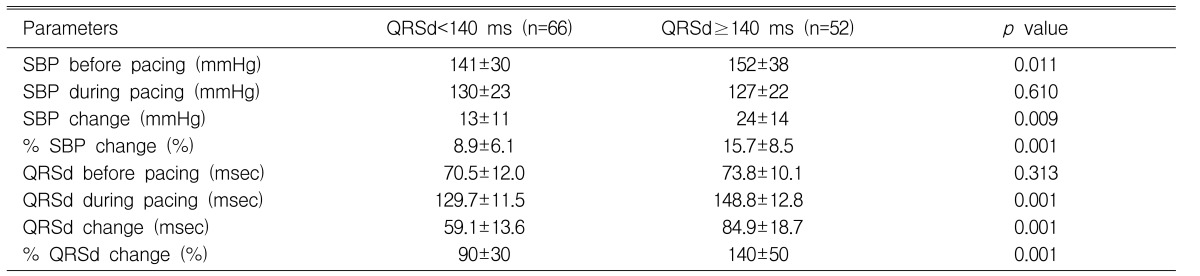
The hemodynamic change according to paced QRS duration during RV pacing
The SBP prior to pacing was higher in the group of paced QRS duration at more than 140 ms than in the group of paced QRS duration at less than 140 ms (p=0.011, 0.009, respectively). The decrease of SBP during pacing was greater in the same respective groups. The percent decrease of SBP during pacing was 8.9±6.1% in relation to the group of paced QRS duration at less than 140 ms and 15.7±8.5% in the group of paced QRS duration at more than 140 ms (p=0.001) (Table 3).
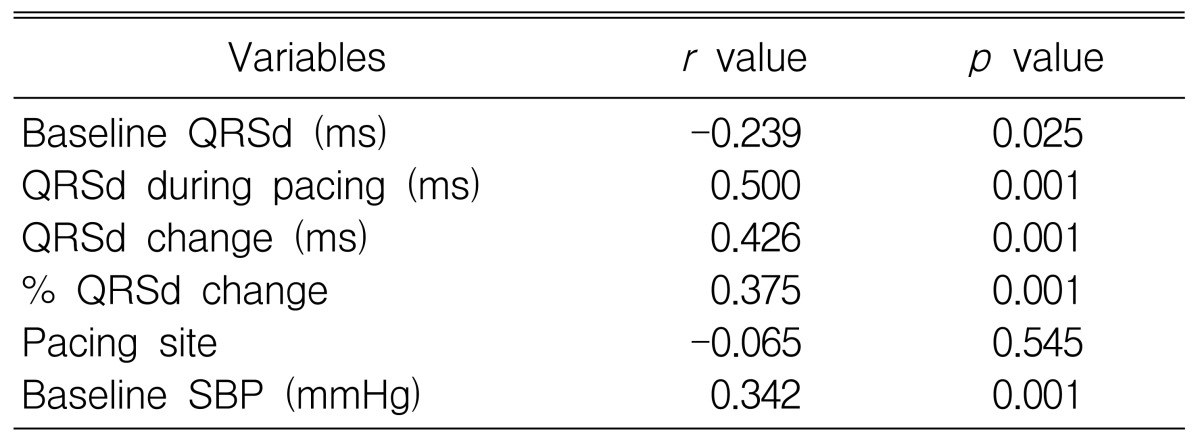
The factors related with the decrease in SBP during RV pacing
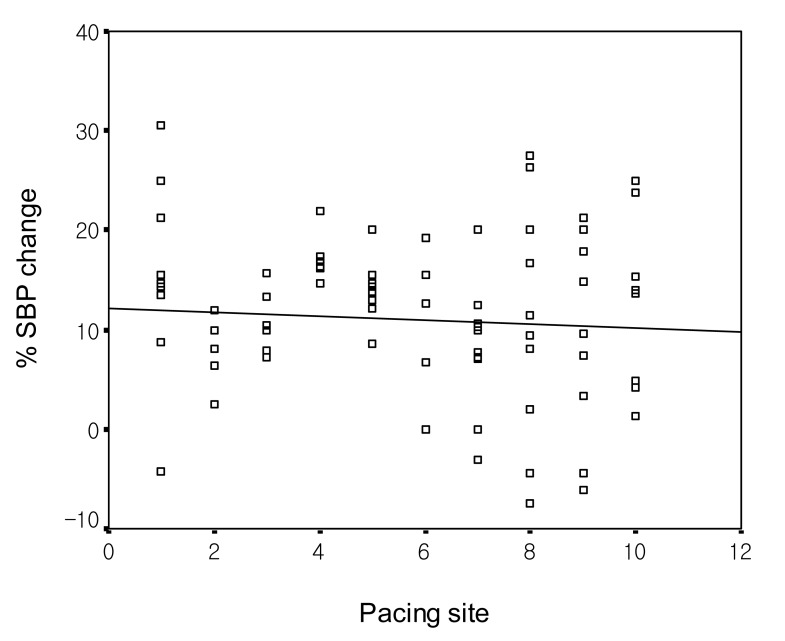
Significant affirmative correlation was found concerning the QRS duration during pacing, the change of QRS duration during pacing and the percent in relation to SBP change (r=0.500, p=0.001, and r=0.426, p=0.001) (Table 4, Figure 1, 2). A significant positive correlation which connected the baseline SBP to the percent SBP change (was also found) (r=0.342, p=0.001) (Table 4, Figure 3). No significant correlation, however, was established between the pacing site and the percent SBP change (r=-0.065, p=0.545) (Table 4, Figure 4).
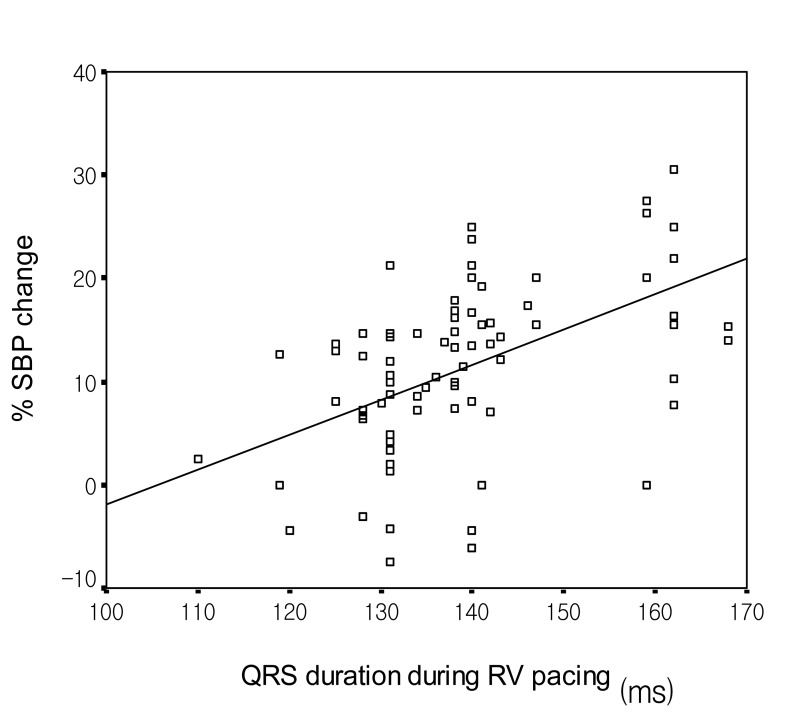
Change in systolic blood pressure according to the QRS duration during right ventricular pacing (r=0.500, p=0.001). SBP, systolic blood pressure; RV, right ventricle.
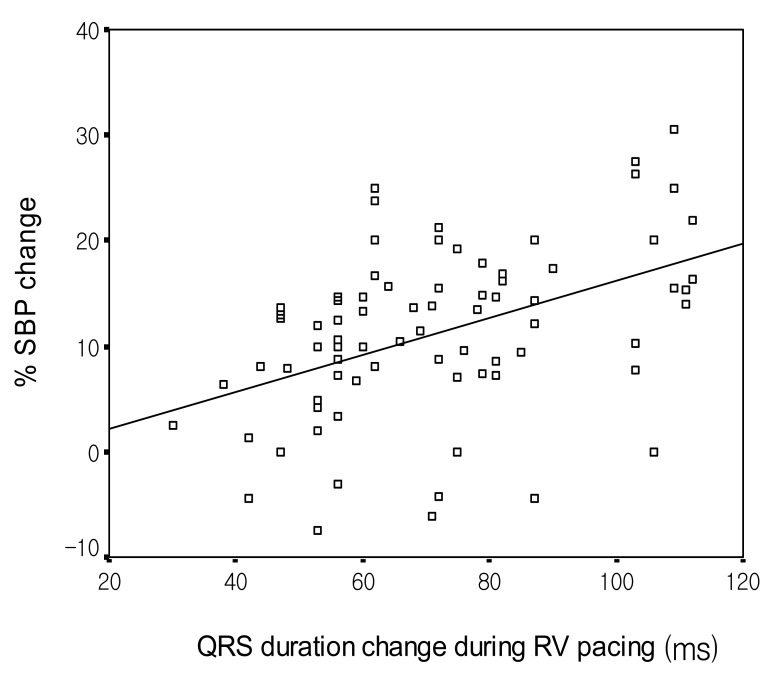
Change in systolic blood pressure according to the change in QRS duration during right ventricular pacing (r=0.426, p=0.001). SBP, systolic blood pressure; RV, right ventricle.
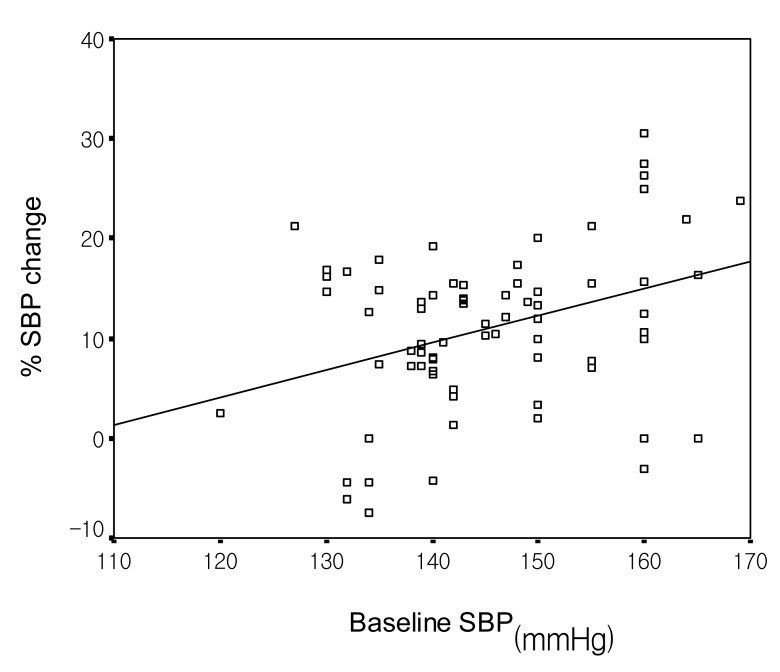
Change in systolic blood pressure according to the baseline SBP (r=0.342, p=0.001). SBP, systolic blood pressure.
The change of SBP and QRS duration according to the baseline SBP
The SBPs observed prior to pacing were 125±14 mmHg and 158±17 mmHg The SBP during pacing was detected to be 114±11 mmHg and 137±13 mmHg, and the decrease of SBP was noted to be 11±10 mmHg and 20±13 mmHg in relation to the group of baseline SBP below 140 mmHg and in the cluster with baseline SBP at more than 140 mmHg, respectively (p<0.001, =0.008, <0.001, respectively) (Table 5).
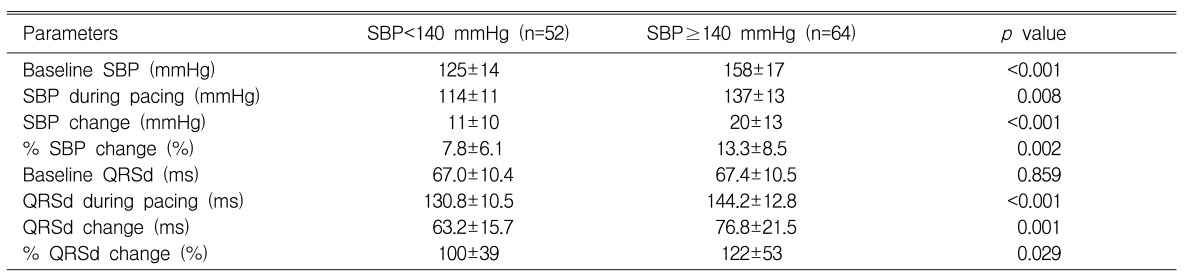
Change in systolic blood pressure and QRS duration according to the baseline systolic blood pressure
The QRS duration and the increase of QRS duration during pacing were greater in the cluster with baseline SBP at more than 140 mmHg than in the group of baseline SBP below 140 mmHg, respectively (p<0.001, =0.001, respectively) (Table 5).
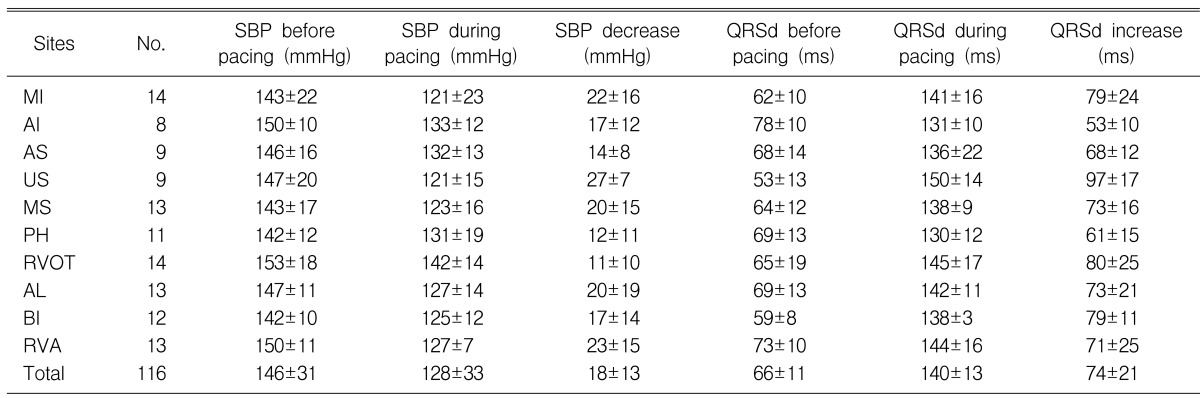
Multivariate analysis for the prediction of decrease in SBP during RV pacing
Multiple logistic regression analysis was carried out in order to predict the decrease in SBP during RV pacing. The baseline SBP and the QRS duration during pacing acted as independent indicators for the decrease in SBP during pacing (p<0.001, =0.001) (Table 6). The QRS duration prior to pacing and the pacing site were not deemed to be independent predictive factors (Table 6).
DISCUSSION
Intraventricular conduction disturbances, as manifested by amplified QRS intervals, are linked to poor short- and long-term outcomes in patients suffering from congestive heart failure1, 2). Silvet et al.12) tested the hypothesis that increased QRS duration seen in patients with moderate or severe left ventricular dysfunction resulted in higher mortality. They separated the patients into two groups; those with normal (<110 ms) QRS duration and those with prolonged (≥110 ms) QRS duration. Patients with increased QRS duration tended to be older, had lower ejection fractions, lower heart rates, larger left ventricular cavities, larger left atrial sizes, and longer QT intervals. They also had 6-year survival rates of 40%, as compared to 60% for patients exhibiting normal QRS duration. This allowed them to conclude that QRS protraction is associated to an increase in mortality. This is independent of the levels of ejection fraction, rhythm, and age.
Prolonged QRS duration is also closely associated to the poor prognosis of patients with acute myocardial infarction. Brilakis et al.13) examined whether an increased QRS duration in the lack of bundle branch blocks on the presenting electrocardiogram of patients showing acute myocardial infarction is related to decreased survival. They established that QRS duration of more than 100 ms in the absence of a bundle branch block can independently predict increased mortality in patients with non-ST elevation myocardial infarction. The lower survival rate in patients with myocardial infarction can be explained, in part, with the following mechanisms. First, increased QRS duration is powerfully correlated with heart failure, both upon admission (as evidenced by worse Killip class) and upon dismissal (as evidenced by the decreased predismissal ejection fraction). Second, QRS protraction is associated with ischemia and multivessel coronary artery disease. In patients with normal coronary arteries, QRS duration diminishes with exercise, probably due to an increase in the sympathetic tone. In contrast, in patients with coronary artery disease, QRS duration actually increases during exercise testing14, 15). Michaelides et al.14) reported that exercise-induced QRS prolongation was proportional to the number of coronary arteries with stenosis. This is seen at levels of more than 70%. Mean QRS prolongation was 4.8±7.5 ms in patients with 1-vessel disease, 7.8±11.8 ms in patients with 2-vessel disease, and 13.3±12.1 ms in patients with 3-vessel disease. Third, QRS protraction is associated with development of ventricular tachycardia or fibrillation. In the 743 patients of the placebo arm of the Cardiac Arrhythmia Suppression Trial16) with stable coronary artery disease and exhibiting QRS duration of more than 100 ms, the risk ratio was 1.4 for new or aggravated congestive heart failure, 1.5 for arrhythmic death or cardiac arrest, and 1.4 for all-cause mortality. In post-acute myocardial infarction patients, QRS protraction was significantly correlated with arrhythmic events17). Therefore, QRS protraction may be seen as a marker of increased vulnerability to reentrant ventricular dysrhythmias and arrhythmic death.
In addition to QRS protraction seen on resting electrocardiograms, increased QRS duration during pacing may be connected to serious cardiac disease. Sumiyoshi et al.9) studied 114 patients who had undergone pacing for atrioventricular block. The patients were divided into one group with paced QRS duration of more than 180 ms and a second group with paced QRS duration of less than 180 ms. The incidence of underlying heart disease was higher (83% vs 32%, p<0.01) and reduced left ventricular ejection fraction (49±17% vs 68±10%, p<0.01) and increased left ventricular end-diastolic dimension (57.1±7.9 mm vs 48.5±5.6 mm, p<0.01) were more prominent as seen in the group with paced QRS duration of more than 180 ms than in the group with paced QRS duration of less than 180 ms. They were then able to conclude that patients with a prolonged paced QRS duration had more serious heart disease, and the paced QRS duration could be valuable in indicating impaired left ventricular function.
Ventricular pacing, such as VVI or VVIR, is the most frequently used vertircular pacing mode worldwide18). However, the major limitation of this particular ventricular pacing mode is that synchrony between atrium and ventricle cannot be maintained.
Ventricular dysfunction may develop after prolonged VVI(R) pacing at the RV. This is associated with prolonged QRS duration during pacing. Correction of this conduction defect by multisite ventricular pacing improves left ventricular function and its hemodynamic performance10, 11). In the present study, a significant positive correlation was found between the paced QRS duration and percent SBP change. Affirmative correlation between the baseline SBP and percent SBP change was also found. The baseline SBP and paced QRS duration turned out to be independent predictors of acute hemodynamic deterioration during pacing.
Our results suggest that the ventricular pacing lead should be placed at the site where the paced QRS duration is minimum during permanent pacemaker implantation. This should preferably be at a level of less than 140 ms.