Encapsulating peritoneal sclerosis: case series from a university center
Article information
Abstract
Background/Aims
Encapsulating peritoneal sclerosis (EPS) is an often-fatal complication of long-term peritoneal dialysis (PD). We here report the clinical features of EPS in Korean PD patients from a single university center.
Methods
The data were collected retrospectively from 606 PD patients at Kyungpook National University Hospital, between August 2001 and August 2011. The diagnosis of EPS was based on clinical signs and symptoms, and confirmed by radiological findings.
Results
Eight patients (1.3%, four males) were diagnosed with EPS. The mean age of the patients was 48.5 years (range, 33 to 65). The mean duration of PD was 111.8 months (range, 23 to 186). All patients except for one had three or more episodes of peritonitis. Seven patients were diagnosed with EPS after stopping PD, and only one stayed on PD after initial diagnosis and treatment. Total parenteral nutrition and corticosteroids, in addition to tamoxifen therapy, were used to treat most of the patients, and one patient underwent surgery (adhesiolysis). The overall mortality rate was 50%.
Conclusions
EPS is a serious, life-threatening complication in patients on long-term PD. To reduce the incidence and mortality rate of EPS, careful monitoring and early diagnosis is needed.
INTRODUCTION
Encapsulating peritoneal sclerosis (EPS), a serious complication of long-term peritoneal dialysis (PD), is characterized by a progressive intra-abdominal inflammatory process, resulting in sheets of fibrous tissue that cover and constrict the viscera, thereby compromising the motility and function of the bowel [1]. In the later stages of the disease, the small intestinal loops are encapsulated by thick adhesions, so called "cocoons."
In the literature, the incidence of EPS ranges from 0.54% to 4.4%, and increases with the length of time on PD, especially after 5 years [1-5]. After 15 years on PD, incidence may exceed 15%. EPS may develop or symptomatically progress after discontinuation of PD, and transfer to hemodialysis (HD) or transplantation [1,3]. The exact cause and pathogenesis are still not clear. Kawanishi et al. [6] suggested the two-hit hypothesis for the development of EPS; long-term use of bioincompatible solutions may induce peritoneal fibrosis and sclerosis (first hit), followed by inflammation (second hit).
As a diagnostic tool, abdominal computed tomography (CT) scans of EPS patients show peritoneal thickening, peritoneal calcification, loculated fluid collections, tethering of the small bowel, and bowel wall thickening [7].
The early clinical features of EPS may be nonspecific and are often not recognized until the patient develops complications, such as bowel obstructions. Although attempts have been made to identify biomarkers for diagnosing EPS, to date, there are no reliable biochemical or radiological screening tests, to identify patients at risk, or in the early stages of EPS [8].
The aim of this study was to examine the clinical characteristics of EPS in Korean PD patients from a single university center.
METHODS
Clinical criteria
The data were retrospectively collected from Kyungpook National University Hospital between August 2001 and August 2011. EPS diagnosis was based on medical records, including clinical features and radiological confirmation. Clinical data were obtained regarding age, gender, duration of PD prior to diagnosis, age at the start of PD, underlying causes of end-stage renal disease (ESRD), number of cumulative peritonitis episodes, causative organisms of peritonitis, treatment options and outcomes. The diagnosis of EPS was based on the guidelines proposed by the International Society of Peritoneal Dialysis Ad Hoc Committee on ultrafiltration management in PD, and was confirmed by radiological examination [5].
Radiological criteria
Two attending radiologists with more than 5 years of experience in abdominal imaging reviewed the abdominal CT scans of eight EPS patients. Before scoring, consensus was achieved on all items during the review of the images, and then independent scoring was made by each reader. The findings of the imaging review were scored according to the grading system proposed by Tarzi et al. [8]. Peritoneal calcification, peritoneal thickening, bowel wall thickening, bowel tethering, loculation, and bowel dilatation were recorded and graded. A total CT score was calculated for each scan by summing each of the six parameters.
RESULTS
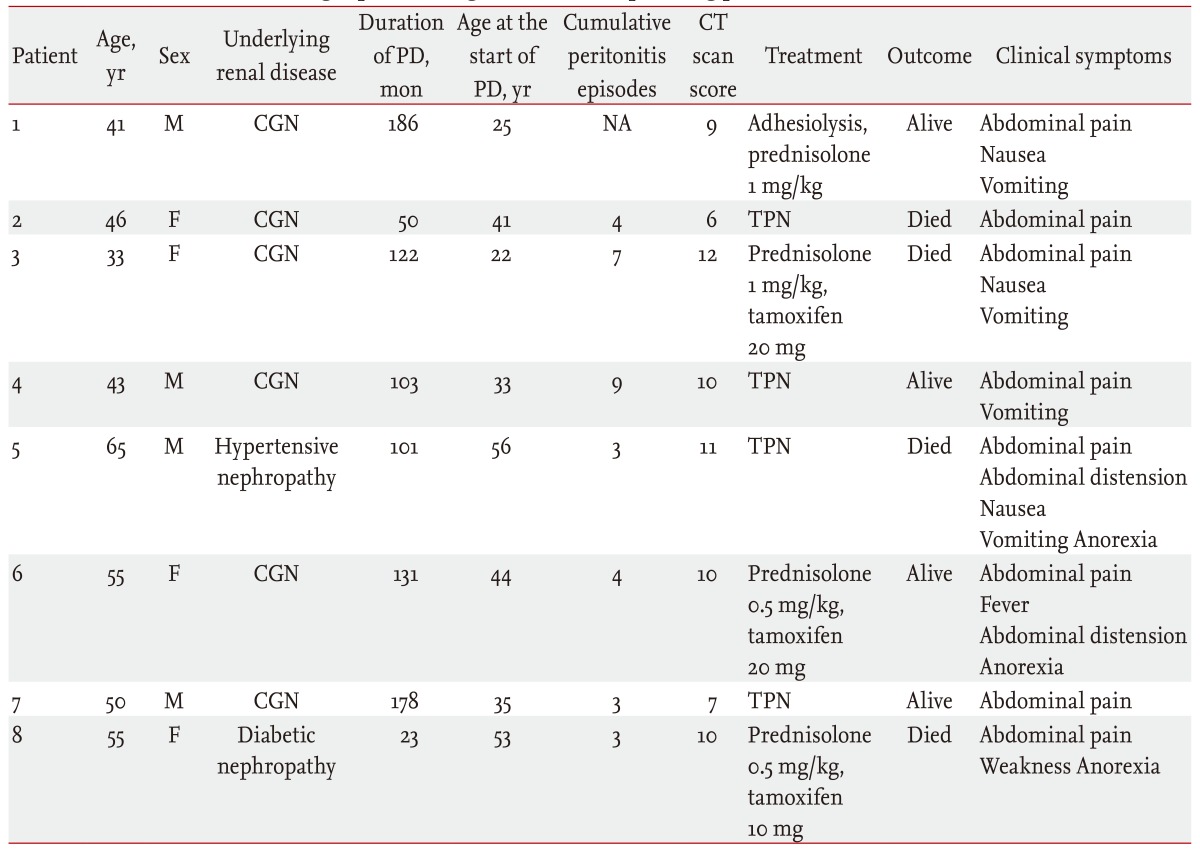
Eight patients (1.3%) diagnosed with EPS were retrospectively identified among 606 PD patients during the study period. Further demographic and clinical information is presented in Table 1. The mean age of the patients (four males and four females) was 48.5 ± 9.9 years (range, 33 to 65). The mean age at the start of dialysis was 38.6 ± 12.2 years (range, 22 to 56) and the mean duration of PD was 111.8 ± 56.4 months (range, 23 to 186). In six patients, the cause of ESRD was chronic glomerulonephritis and for the remaining two patients, it was hypertensive nephrosclerosis and diabetic nephropathy. The symptoms of EPS were predominantly anorexia, nausea, vomiting, abdominal distension, and pain. All patients had three or more episodes of peritonitis, except for one, for whom we could not clarify the number of episodes. A total of 33 episodes of peritonitis were diagnosed and the peritonitis rate was one episode every 21.5 patient-months in the seven EPS patients. There were 14 culture-negative episodes, and the most common organisms identified were methicillin-sensitive coagulase-negative Staphylococcus (five episodes), followed by the Bacillus species (four episodes), Escherichia coli (two episodes), methicillin-resistant coagulase-negative Staphylococcus (one episode), and Cryptococcus albidus (one episode). Enterococcus species and Bacillus species were identified in one episode, and recurrent peritonitis with various organisms, such as methicillin-resistant coagulase-negative Staphylococcus, methicillin-sensitive coagulase-negative Staphylococcus, Corynebacterium species, Bacillus species, Enterococcus species, Candida species, methicillin-resistant Staphylococcus aureus, and Pseudomonas species, were found in five episodes. Six patients were treated with icodextrin solution at diagnosis. Five patients were treated with β-blockers (carvedilol, 25 to 50 mg daily), and seven with angiotensin-converting enzyme inhibitors or angiotensin receptor blockers for more than 6 months prior to the diagnosis.
Fig. 1 shows typical CT scans of the EPS from the study patients. The mean CT score for the eight EPS patients was 9.38 ± 2.0.
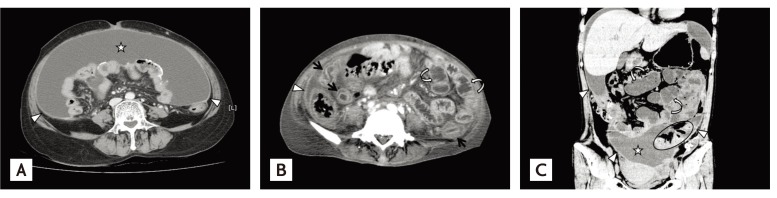
Abdomino-pelvic computed tomography (CT) scan of patients diagnosed with encapsulating peritoneal sclerosis. (A) Axial contrast-enhanced CT image showing loculated fluid collection (star), parietal peritoneal thickening (arrowheads), and peritoneal calcification. The small bowel loops are collected centrally by the encapsulating fibrotic peritoneum. (B) Axial view showing bowel wall thickening (arrows) and bowel distension (curved arrows). Peritoneal thickening (arrowhead) is also present. (C) Coronal view showing tethering of the small bowel loops (circle), parietal peritoneal thickening (arrowheads), bowel distension (curved arrows), and loculated fluid collection (star).
Among the eight patients, seven were diagnosed with EPS after discontinuing the PD due to inadequate dialysis, peritonitis, or ultrafiltration failure (mean interval, 7.9 ± 6.3 months), and one stayed on PD after the initial diagnosis of EPS.
Total parenteral nutrition was used in all patients. Three patients were treated with glucocorticoids (0.5 to 1 mg/kg/day) in addition to tamoxifen (10 to 20 mg daily) and four with total parenteral nutrition only. Only one patient received glucocorticoid treatment (1 mg/kg/day) combined with elective surgical adhesiolysis.
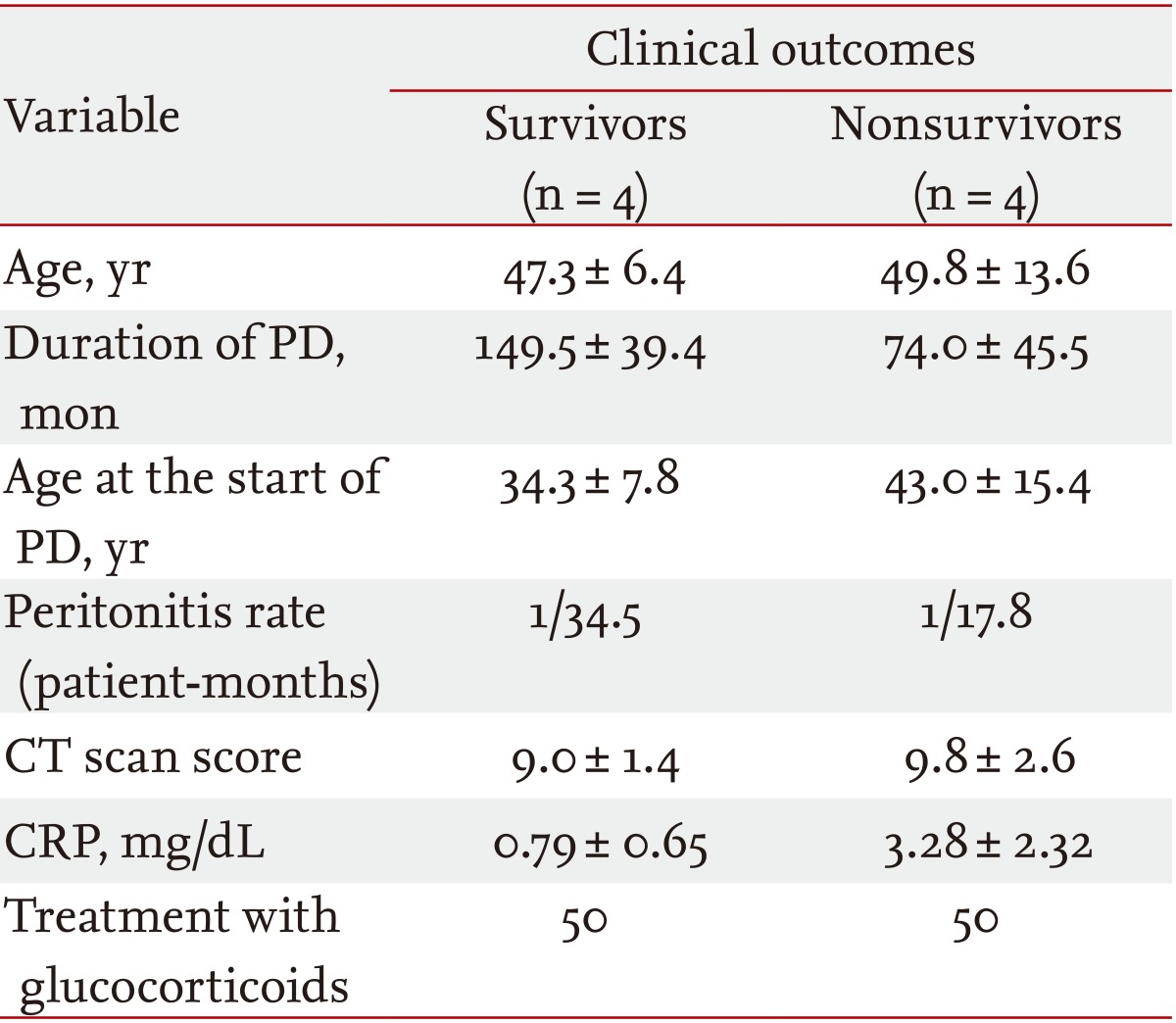
Four of the EPS patients died during the course of this study. The mean time to death from the first episode of EPS was 13.8 months. Among the four surviving patients, one remained on PD and is clinically stable, and the other three transferred to HD. One of the three patients who transferred to HD underwent a renal transplant about 17 months later. Clinical characteristics of the survivors and nonsurvivors are given in Table 2. Mean age at diagnosis, mean age at the start of PD, mean peritonitis rate, total CT score, treatment with glucocorticoids and C-reactive protein were comparable between the two groups. However, the mean cumulative duration on PD was longer in the survivors (149.5 months vs. 74.0 months).
DISCUSSION
EPS is a life-threatening complication of PD. The exact cause of EPS is unknown. However, multiple possible contributing factors may contribute, including the duration of time on PD, age at the start of PD, recurrent episodes of bacterial peritonitis, the use of acetate dialysis solution, chlorhexidine, glucose/hypertonic solution, and β-blockers [5,9].
In this study, 1.3% of patients on PD were diagnosed as having EPS, and this was similar to previous reports; 0.8% from Korea [10], 1.5% to 3.3% from the United Kingdom [11,12], and 2.7% from the Netherlands [9]. In Japan, between 2004 and 2005, the incidence was even higher; up to 17.2% for patients on PD for longer than 15 years [3,13]. A recent study from Australia and New Zealand reported cumulative incidences of 0.3%, 0.8%, and 3.9% after 3, 5, and 8 years on PD, respectively [4].
All patients except for one had been on PD for more than 4 years, and the mean age at the start of PD was 38.6 years, with a range of 22 to 56 years. Another study showed that the younger the patient at the start of the PD, the greater the chance they had of developing EPS [9]. This variable does not seem to be a result of being on PD for longer, or the result of a longer follow-up duration from the start of PD. Peritoneal remodeling is a process in which injury to the mesothelial cells plays a key role. In response to multiple assaults, such as from glucose, for example, mesothelial cells secrete cytokines that subsequently lead to the recruitment of macrophages and fibroblasts. Peritoneal fibrosis is then a result of disrupted repair, with fibrin being deposition on a denudated mesothelial cell layer [14]. It may be that this repair process is more vigorous in younger patients, leading to an earlier onset of fibrosis [9].
Previous studies suggested that PD peritonitis might predispose patients to EPS, particularly if it is caused by S. aureus, fungi, and/or Pseudomonas species [2,15]. A Japanese study showed that 25% of EPS cases were associated with bacterial peritonitis [3]. Peritonitis with S. aureus is a major risk for developing EPS since this coagulase-positive organism produces an enzymatic activity capable of converting fibrinogen to fibrin, the major matrix component of intestinal adhesions [16]. However, in this study, it is difficult to conclude that any risk of EPS is associated with any particular organism due to limited information on the causative organisms, and a relatively high culture-negative peritonitis rate (42.4%). Our EPS cases were for the most part not caused by coagulase-producing organisms. The most commonly identified organism was methicillin-sensitive coagulase-negative Staphylococcus (five episodes). Coagulase-negative Staphylococcus is the second most common organism in all reported cases, with a variety of other bacteria [11], and typically causes mild peritonitis that responds rapidly to therapy. These staphylococcal species, although less virulent than S. aureus, possess determinants that contribute to both colonization and infection. The two main virulence factors involved in immune evasion are; biofilm formation and production of a poly-γ-DL-glutamic acid capsule. These virulence factors may evade the host immune defense by protecting coagulase-negative Staphylococcus from polymorphonuclear neutrophil phagocytosis, antimicrobial peptides, and deposition of antibodies and complement [17]. Therefore, coagulase-negative Staphylococcus with these factors could cause persistent peritonitis and increase the risk of EPS.
A recent study suggested that icodextrin-based dialysis solutions could affect peritoneal reactivity [18]; however, Habib et al. [19] reported that icodextrin did not increase the risk of developing EPS. In this study, six of eight EPS patients used icodextrin. It is difficult to identify an association between icodextrin use and EPS development, due to the limitations of the design of this study, but it is related to increased numbers of prescriptions in patients with a decreased peritoneal ultrafiltration volume, prior to diagnosis of EPS.
In addition, we analyzed the concomitant medications in these patients. β-Blockers such as practolol were implicated in the pathogenesis of EPS in an earlier study, as they inhibited mesothelial synthesis and the release of surfactants, leading to damage of the peritoneal membrane [20]. However, recent data do not support this theory for β-blockers currently in use [2]. Additionally, the beneficial effects of a renin-angiotensin system (RAS) blockade on the peritoneal membrane have been reported [21,22]. However, there are no known clinical studies that show the protective effects of a RAS blockade on the development of EPS.
It is generally accepted that, after a diagnosis of EPS, PD should be discontinued, and the patient transferred to HD. However, it should be taken into consideration that some cases of EPS are clinically less severe, and could worsen if PD is stopped. Moreover, most cases of EPS are diagnosed only after the discontinuation of PD [3,23]. In this study, most of the patients were diagnosed with EPS after discontinuation of PD; only one stayed on PD after diagnosis and treatment of EPS.
Drug therapy with corticosteroids [24], tamoxifen [25], and immunosuppressants [26] have been reported to be beneficial for EPS in a small number of cases. Surgical enterolysis is considered for severe intestinal obstructions. Surgical mortality, which was as high as 50% in the past, can be reduced 4% [6] in the hands of an experienced surgeon. Contrary to previous small-scale case studies, a recent large-scale study in the United Kingdom showed no difference in outcomes for patients treated with steroids, immunosuppression, tamoxifen, or combinations of these, compared to patients who were not treated [27]. Therefore, early diagnosis may be the only way to improve the prognosis.
There are no predisposing conditions known to be primary causes of ESRD. In this report, only one patient had diabetic nephropathy and developed EPS within 2 years (23 months) after the start of PD, and died within 1 month despite treatment with tamoxifen and glucocorticoid. However, diabetic patients seldom develop EPS [9,28], and it is not clear whether diabetes protects against the development of EPS. However, it is possible that long-term survival on dialysis is significantly reduced in patients with diabetes, and therefore, diabetics may not live long enough to develop this complication.
To conclude, EPS is a rare but serious complication in Korean patients receiving long-term PD, and many barriers for diagnosing EPS in its early stages remain. To reduce the incidence and mortality of EPS, careful monitoring and early diagnosis are needed for patients receiving PD, and especially for those on long-term PD.
KEY MESSAGE
1. This case series has demonstrated the prevalence, clinical characteristics and prognosis of encapsulating peritoneal sclerosis (EPS) in Korean peritoneal dialysis (PD) patients from a single university center. It also discussed several associated factors for EPS, because the exact causes of EPS are still unknown, but multiple factors including the duration of time on PD, age at the start of PD, recurrent episodes of bacterial peritonitis, the use of acetate dialysis solution, chlorhexidine, glucose/hypertonic solution, and β-blockers are suggested as possible contributing factors for EPS.
2. Abdominal computed tomography scan is a good diagnostic tool in a suspicious case of EPS. In addition, drug therapy with corticosteroids, tamoxifen, immunosuppressants with or without surgical enteroloysis has been reported to be beneficial for EPS.
3. There are no reliable screening tests, especially in the early stage of EPS, and therefore careful monitoring is needed for patients receiving long-term PD.
Acknowledgments
This study was supported by grants from the Korea Healthcare Technology R&D Project, the Ministry for Health, Welfare and Family Affairs, Republic of Korea (A111345, A102065).
Notes
No potential conflict of interest relevant to this article is reported.