The scientific achievements of the decades in Korean Acute Myocardial Infarction Registry
Article information
Abstract
The Korea Acute Myocardial Infarction Registry (KAMIR) was the first nationwide registry data collection designed to track outcomes of patients with acute myocardial infarction (AMI). These studies reflect the current therapeutic approaches and management for AMI in Korea. The results of KAMIR could help clinicians to predict the prognosis of their patients and identify better diagnostic and treatment tools to improve the quality of care. The KAMIR score was proposed to be a predictor of the prognosis of AMI patients. Triple antiplatelet therapy, consisting of aspirin, clopidogrel and cilostazol, was effective at preventing major adverse clinical outcomes. Drug-eluting stents were effective and safe in AMI patients with no increased risk of stent thrombosis. Statin therapy was effective in Korean AMI patients, including those with very low levels of low density cholesterol. The present review summarizes the 10-year scientific achievements of KAMIR from admission to outpatient care during long-term clinical follow-up.
INTRODUCTION
The Korea Acute Myocardial Infarction Registry (KAMIR) was the first nationwide, population-based, multicenter registry, and was launched in November 2005. The ethics committee at each participating institution approved the study protocol. Informed consent was obtained from each patient. Trained study coordinators at each participating institution collected the data using a standardized format. Standardized definitions of all variables were determined by the steering committee board of KAMIR. Data were submitted via password-protected web-based electronic case report forms.
KAMIR is an ongoing registry that covers the complete spectrum of acute myocardial infarction (AMI), including long-term clinical follow-up. The registry included 55 representative centers, and contained data from ~52,000 patients over a 10-year period. A total of 122 publications have used KAMIR data, including 103 articles in Science Citation Index journals. The most important aspect of this great accomplishment is that the clinical data have been made available to all participating centers without limitations. The present review focuses on the results of publications regarding AMI, from admission to the outpatient department, over a 1-year follow-up. The publications were divided into three categories based on predictors of prognosis, treatment, and special patient groups.
PREDICTORS OF PROGNOSIS
Risk stratification
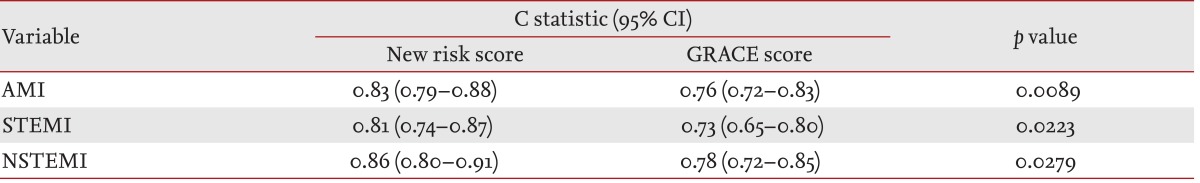
Risk assessment at the time of admission and discharge is important for deciding treatment strategy and postdischarge management. Thrombolysis in myocardial infarction (TIMI) risk score and the Global Registry of Acute Coronary Event (GRACE) risk models are examples of tools for risk stratification. However, these models were developed and validated from the late 1990s to the early 2000s. The rate of percutaneous coronary intervention (PCI) and use of clopidogrel was only 30% during that period, whereas these treatments are used in approximately 90% of patients currently. Furthermore, previous models did not consider risk factors such as: admission hyperglycemia, the presence of stroke or peripheral artery disease, and left ventricular systolic function. Most importantly, TIMI and GRACE risk scores focused predominantly on western AMI patients. KAMIR score was developed for admission and postdischarge risk prediction over a 1-year period [1,2]. The KAMIR score is composed of six independent variables related to 1-year mortality: age, Killip class, serum creatinine, no in-hospital PCI, left ventricular ejection fraction, and admission glucose (Fig. 1). The KAMIR score exhibited significant differences in prediction accuracy compared with the GRACE model in a validation cohort (Table 1). The CHA2DS2-VASc scoring system was also useful for risk stratification in patients with AMI, irrespective of atrial fibrillation [3,4].
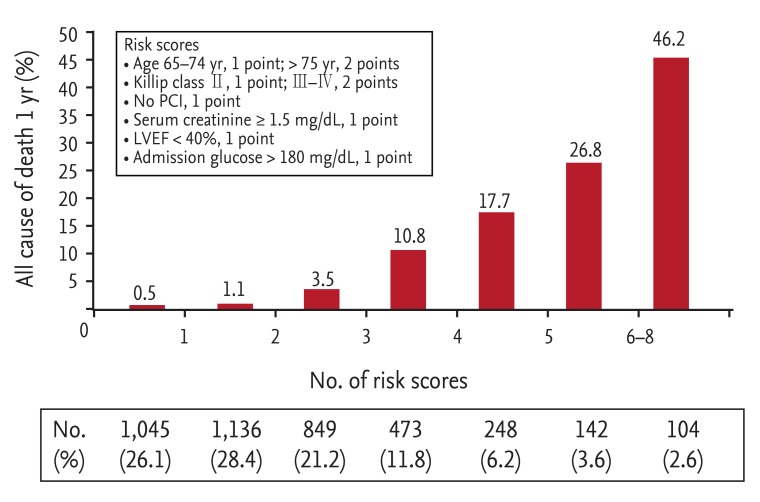
Korea Acute Myocardial Infarction Registry score for predicting 1-year mortality. PCI, percutaneous coronary intervention; LVEF, left ventricular ejection fraction.
Prognostic factors in the admission period
Coronary risk factors
Hypertensive AMI patients had worse outcomes, but antecedent hypertension was not associated with 1-year mortality [5,6]. Patients with prior cerebrovascular disease (CVD) presented more frequently with non-ST segment elevation myocardial infarction (NSTEMI), were less likely to receive reperfusion therapy, and had worse clinical outcomes compared with patients without a history of CVD [7]. A family history of coronary artery disease was an independent prognostic factor, particularly in patients with low risk profiles and female gender [8]. Surprisingly, both smoking and obesity were risk factors for AMI development, but were associated with decreased mortality rates after AMI. These phenomena were also observed in KAMIR [9,10,11,12].
Arrival timing
A disparity between ST-segment elevation myocardial infarction (STEMI) and NSTEMI was observed [13,14]. Patients admitted during off-hours had a longer waiting time until their procedure, and received less PCI compared with on-hours visitors. In contrast, there was no clinical impact in patients with NSTEMI [15]. However, in-hospital mortality was increased in patients with STEMI [16]. An additional report showed that the time delay in STEMI was not associated with in-hospital mortality [17]. In addition to treatment delay, the incidence of AMI varied according to the season and month. Meteorological parameters, including air temperature, humidity, and sunshine duration, had a significant influence on the occurrence of AMI, particularly in young and female patients [18].
Clinical findings
Painless AMI occurred in individuals that were older, female or non-smokers, or had diabetes mellitus (DM) or renal failure; these patients had worse outcomes [19,20]. N-terminal pro-B-type natriuretic peptide levels were associated with short-term mortality in patients with primary PCI [21]. Renal dysfunction and C-reactive protein also had prognostic effects for AMI [22,23,24].
Coronary artery lesions
Unprotected left main artery-related AMI resulted in fatal in-hospital outcome, even in cases with non-culprit lesions [25,26]. However, no significant differences were detected in hospital survivors during long-term follow-up [27,28]. Patients with NSTEMI and total occluded infarct-related artery had a worse outcome than did those with non-occluded NSTEMI [29]. Left circumflex artery-related AMI was associated with reduced ST-segment elevation and treatment-delay [30]. Interestingly, AMI patients with non-significant stenosis in a coronary angiogram had a similar outcome as patients with one- or two-vessel disease [31].
TREATMENT OF AMI
Pharmaceutical management
Medical treatment is an essential option and interventional management in patients with AMI. Intensive medical treatment might improve the in-hospital outcome of patients who did not undergo PCI [32]. β-Blocker treatment reduced the long-term mortality in patients with MI and preserved systolic function during PCI [33]. Insurmountable angiotensin II receptor blockers (ARB) were more effective than ARB in AMI [34]. Dual blockage of the renin-angiotensin system using angiotensin-converting enzyme inhibitor and ARB could increase the risk of adverse outcomes in severe renal dysfunction patients, without eliciting any clinical benefits [35]. Trimetazidine and nicorandil were not class I drugs in AMI. Additive effects of the use of these drugs have been reported; however, additional studies are needed [36,37].
The optimal loading dose of clopidogrel in Asian patients has not been investigated fully. Data in the KAMIR revealed that the standard loading dose clopidogrel group had similar clinical results compared with the double loading dose group before PCI [38,39]. Low-molecular-weight heparin was associated with a better clinical outcome than unfractionated heparin in patients with AMI [40,41,42].
Interventional treatment
Strategy establishment
Early elective PCI after successful thrombolytic therapy for STEMI remains a controversial recommendation. Patients who underwent PCI within 48 hours of thrombolytic therapy had a long-term clinical benefit compared with those who underwent PCI later [43]. In early latecomer AMI (12 to 72 hours after symptom onset), PCI was associated with a significant improvement in the 12-month clinical outcome [44]. The optimal revascularization strategy in AMI patients, culprit-only or total revascularization, remains unclear. KAMIR reported different results between patients with STEMI or NSTEMI. In NSTEMI, multivessel PCI yielded a better clinical outcome without increasing in-stent restenosis and the progression of diseased vessels (hazard ratio [HR], 0.658; 95% confidence interval [CI], 0.45 to 0.96; p = 0.031) [45]. However, multivessel PCI increased target lesion revascularization without any clinical benefit in STEMI [46].
Stent implantation in AMI
Drug-eluting stents (DESs) were implanted in > 90% of AMI patients in Korea (Table 2) [47]. DESs were superior in terms of promoting target lesion revascularization and had similar safety outcomes compared with bare metal stents (BMSs) in patients with large coronary artery and renal insufficiency [48,49]. Among the DESs, sirolimus-eluting stents (SESs) and everolimus-eluting stents were similar or better than paclitaxel-eluting stents and early-type zotarolimus-eluting stents in terms of target lesion failure [50,51,52,53,54,55]. Intravascular ultrasound-guided PCI did not reduce restenosis and thrombosis in AMI patients [56]. Thrombus aspiration did not improve the clinical outcome of overall patients who underwent primary PCI. In a subgroup analysis, left anterior descending artery occlusion patients had a better prognosis when thrombus aspiration was performed. In addition, the use of a glycoprotein IIb/IIIa inhibitor had a synergistic effect with thrombus aspiration [57].
Secondary prevention
Statin after AMI
The optimal medical therapy after discharge was prescribed at suboptimal rates, particularly in high-risk AMI patients [58,59]. Early and continuous statin therapy improved the prognosis after AMI [60]. Lifesaving medications, including lipid-lowering drugs, were underused in patients with lower low-density lipoprotein cholesterol (LDL-C) levels. More intensive treatments, including lipid-lowering therapy, for AMI in patients with lower LDL-C level might improve clinical outcomes [61]. Statin therapy in patients with LDL-C levels < 70 mg/dL was also associated with improved clinical outcomes (Fig. 2) [62]. Stent thrombosis could be reduced by statins in AMI patients with levels of high C-reactive protein [63]. Statins were also effective in patients with renal dysfunction [64].
Antiplatelet treatment
Dual antiplatelet therapy (DAPT) using aspirin combined with thienopyridine agents such as clopidogrel has become a mainstay of secondary prevention strategies after AMI. Clopidogrel has complimentary effects with aspirin, and reduces adverse cardiac events, including stent thrombosis, compared with aspirin plus warfarin or aspirin alone. However, clopidogrel is a prodrug that requires activation by specific hepatic cytochrome p450 enzymes. This two-step activation process is susceptible to interference by genetic polymorphisms, which can lead to the phenomenon of clopidogrel "nonresponders." Use of an increased dose, addition of other drugs, and development of more potent drugs have been attempted to overcome these shortcomings. In KAMIR, triple antiantiplatelet therapy (TAPT; DAPT + cilostazol) resulted in significantly lower incidences of cardiac death (HR, 0.52; 95% CI, 0.32 to 0.84; p = 0.007), total death (HR, 0.60; 95% CI, 0.41 to 0.89; p = 0.010), and total major adverse cardiac events (HR, 0.74; 95% CI, 0.58 to 0.95; p = 0.019) compared with DAPT in patients with STEMI at the 8-month follow-up [65]. However, the no-reflow phenomenon is a poor prognostic factor for in-hospital mortality after primary PCI [66]. Nevertheless, TAPT was superior to DAPT in patients with AMI who had no-reflow during PCI [67].
INDIVIDUAL PATIENT SUBGROUPS IN AMI
Female gender
There were no gender differences in the initial treatment of AMI. However, the first KAMIR study showed that the success rate of PCI in NSTEMI was lower and the incidence of adverse events after 1 month was higher in females [68]. However, subsequent studies revealed that female gender itself was not an independent risk factor for in-hospital mortality in a multivariate analysis [69,70]. The gender effects might be age-dependent, or due to the presence of more comorbidities and severe hemodynamic conditions at presentation [71].
DM and metabolic syndrome
Generally, DM was a poor prognostic factor for mid-term (1 month to 1 year) clinical outcomes, but not for the short-term prognosis (~1 month) in AMI patients [72,73]. Glucose levels at the time of admission were a prognostic factor for short-term clinical outcomes in the KAMIR. Hyperglycemia at admission was an independent predictor of 1-month mortality in non-DM patients, but not in DM patients [74]. Hyperglycemia at admission was also associated with worse clinical outcomes in DM patients with poorly controlled blood sugar (hemoglobin A1c > 8.0%) [75]. In addition, metabolic syndrome was an important predictor of in-hospital mortality in STEMI patients, and the prognosis was worsen if DM or renal dysfunction was combined [76,77,78]. In metabolic syndrome patients with multi-vessel disease, coronary artery bypass graft had a favorable outcome in terms of revascularization compared with DES (4.8% vs. 12.2%, p = 0.014) [79]. However, there were no significant differences among different types of DES [53].
Renal dysfunction
The estimated glomerular filtration rate (eGFR) was associated with both short- and long-term mortality rates in AMI patients [80,81], and the association between lower eGFR and mortality weakened with increasing age [82]. However, patients with renal dysfunction had a lower likelihood of receiving optimal medical care [83]. Early invasive strategies improved the prognosis in patients with renal dysfunction, with the exception of those with severe chronic kidney disease [84].
Old age
PCI for AMI yielded favorable outcomes, even in elderly patients [85,86,87]. Generally, the clinical status of octogenarians was significantly inferior to that of nonoctogenarians in terms of Killip class ≥ II (34.8% vs. 22.5%, p < 0.001), multivessel disease (65.8% vs. 53.7%, p < 0.001). The rate of 1-year all-cause death was significantly higher in octogenarians compared with nonoctogenarians (22.3% vs. 6.5%, p < 0.001) [88]. However, elderly (> 75 years) AMI patients with cardiogenic shock had a similar outcome after PCI as younger patients [89]. Nonagenarian AMI patients had similar outcomes as octogenarians, despite the higher in-hospital and 1-year mortality rates [87].
CONCLUSIONS
The KAMIR has generated a multitude of publications. In addition, the KAMIR score provides a simple and accurate assessment tool for improving risk stratification in contemporary clinical practice. The prognosis of AMI patients differs according to the presence of coronary risk factors, the time of arrival at the hospital, and clinical findings. Before the surgical procedure, a standard loading dose of clopidogrel was sufficient for most Korean patients. Low-molecular-weight heparin had a better clinical outcome than did unfractionated heparin. DES implantation in AMI patients reduced target lesion failure compared with BMS, and had similar safety profiles. Among DESs, everolimus-eluting and SESs showed better outcomes. Statins reduced adverse cardiac events, including stent thrombosis, irrespective of cholesterol levels. The addition of cilostazol to a dual antiplatelet agent improved clinical outcomes in patients with STEMI that experienced the no-reflow phenomenon during intervention. Individual patient factors, such as female gender, very old age, and chronic kidney disease, were associated with a poor clinical status, and such patients received guideline-directed treatments less frequently. However, thorough and appropriate management could improve the prognosis in these groups.
Acknowledgments
This study was performed with the support of the Korean Circulation Society (KCS) as a memorandum of the 50th Anniversary of the KCS. This study was supported by a grant of the Korean Health Technology R&D Project (HI13C1527), sponsored by the Ministry for Health and Welfare, Republic of Korea.
Notes
No potential conflict of interest relevant to this article was reported.